- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Putting the Patient Back at the Center of Patient-Centered Care
From the editor-in-chief of Evidence-Based Oncology™.
Tho’ much is taken, much abides;
and tho’
We are not now that strength
which in old days
Moved earth and heaven,
that which we are, we are;
One equal temper of heroic hearts,
Made weak by time and fate,
but strong in will
To strive, to seek, to fi nd,
and not to yield.
https://doi.org/10.37765/ajmc.2020.43000
Ulysses
Alfred Tennyson
At this tie of breathtaking innovation in cancer diagnostics and therapeutics, it is easy to become distracted (even mesmerized) by the extraordinary advances in care technology to the point of losing sight of the fundamental fact that a patient’s cancer journey is a human, not a technological, experience.
Throughout the past 3 decades, as I have spoken with patients and their families about a new cancer diagnosis or a change in their goals of care, our discussions have never focused upon molecular biology, genomics, or abstract ideals about targeted drug design. I have yet to engage any patient or family in a discussion of the arcane details of any of the value-based care models. Instead, our discussions are focused on the more meaningful human dimensions of navigating the flood of emotion that stems from a cancer diagnosis; the focus is upon identifying grounded next steps; finding ways to chart a navigable, sustainable steps of a path that culminates in a restoration to wholeness. For some this is a journey that culminates in a cure; for others the focus is upon recovering a sense of wholeness for a patient and their family when a cure is no longer possible. Each patient travels their respective hero’s journey. The reality is that our technological advancements are simply deployable tools for supporting the patient throughout that journey. How care we more eff ectively use these tools to humanize the cancer journey for patients and their families? How can we put the patient back at the center of patient-centered care? How can we more effective and humanly support the patient’s heroic journey?
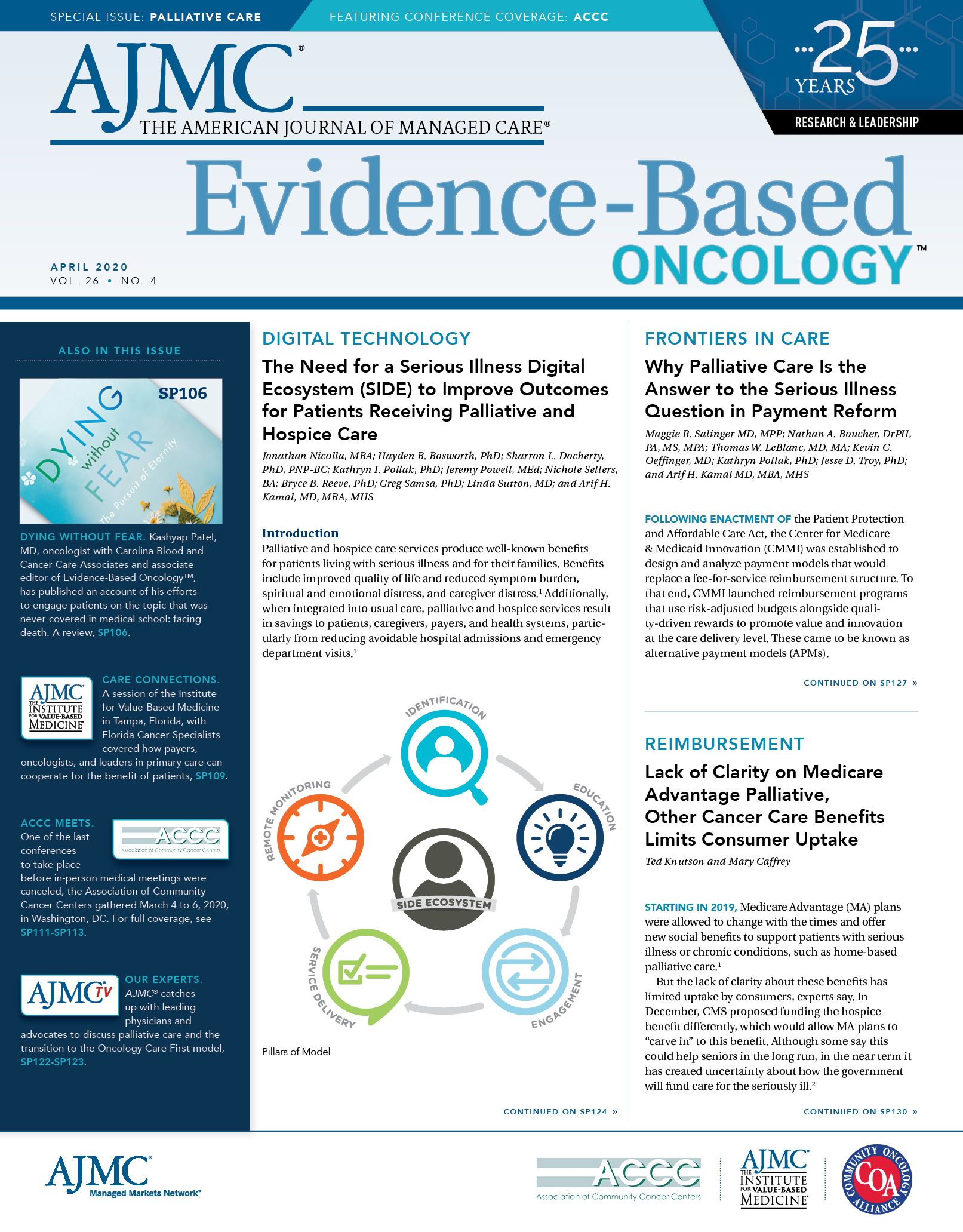
In this issue of Evidence-Based Oncology™ we explore the human dimensions of the cancer care experience in the hope of better understanding how better systems of care can more effectively serve patients and their families. Maggie L. Shaw provides us with the highlights from the Association of Community Cancer Centers’ (ACCC) 46th Annual Meeting on disruptive, innovative ways to improve patient access to care. Jonathan Nicolla and colleagues discuss ways of using digital monitoring to more eff ectively assess outcomes for patients who are receiving palliative and hospice care. Maggie Salinger, MD, and her colleagues discuss the importance of payment reform in ensuring better and more eff ective access to palliative care. Finally, Florence Caffrey Bourg, PhD, reviews Dying Without Fear: The Pursuit of Eternity by Kashyap Patel, MD, which explores the deeply human nature of patients’ cancer journeys.
Advances in care technology have indisputably improved patient outcomes, reduced treatment toxicities, and provided new opportunities for patients with advanced and relapsed cancers to live longer with a better quality of life. Our systems of care, however, have not evolved in ways that engender a more human care experience for either patients or their physicians. As clinicians navigate the near-infi nite number of clicks needed to perform relatively simple care tasks on modern electronic health records and struggle to decipher the evolving rules of billing and reimbursement, the precious left to spend with our patients and their families is increasingly compromised by indifferent systems of care, many of which ironically claim to be patient-centered. In Ulysses, Tennyson writes of the transcendent strength that can arise when we fi rst acknowledge the pain, fragility, and humanness that form the underpinnings of our journey. Building systems of care that acknowledge and build upon this are essential to realize the aspiration of delivering truly patient-centered care.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

