- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
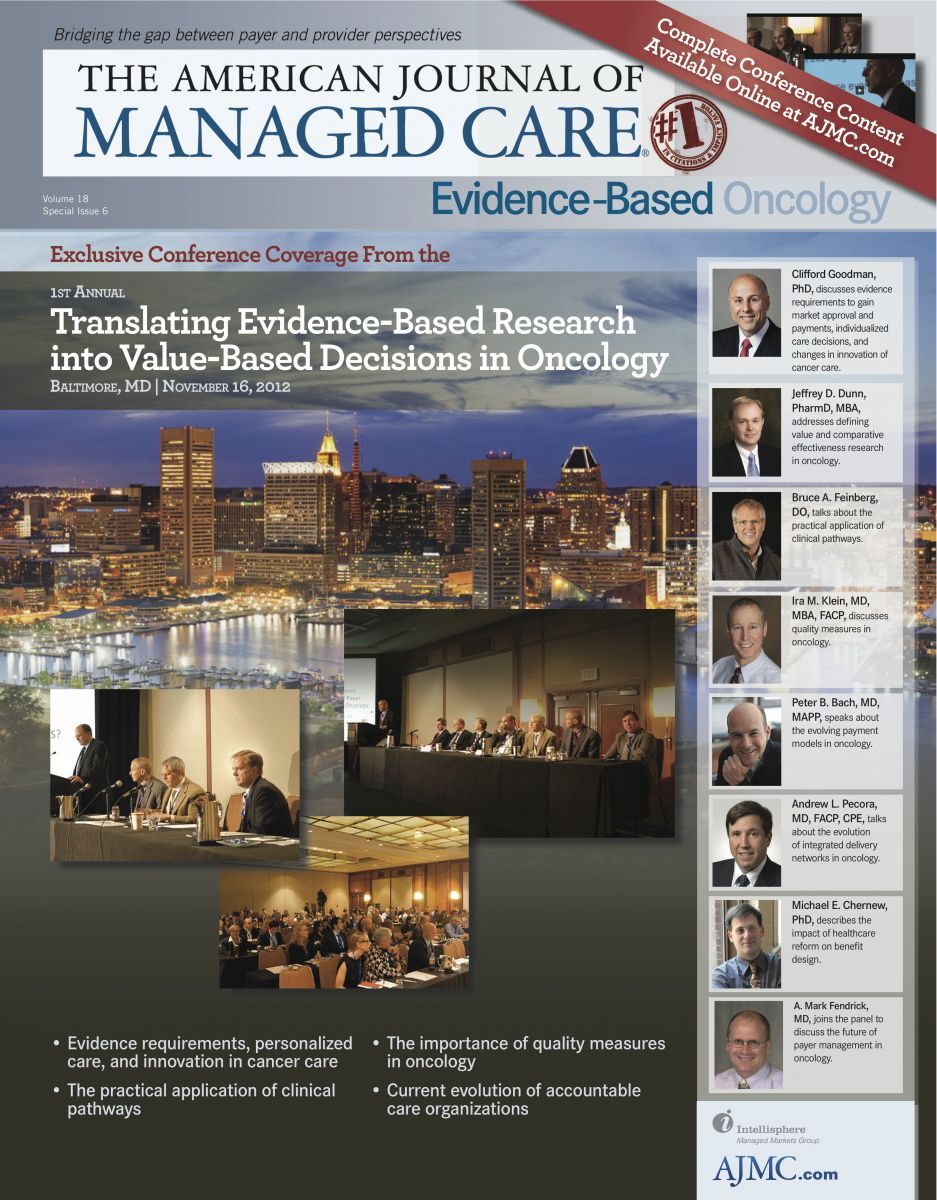
Practical Application of Clinical Pathways
The cost of care for any patient generally follows a variation of Parkinson’s Law. “The more you have available to give to a patient, the more the patient will receive and that requires us to be thinking of different paradigms and not applying medical economics to classical economics,” began Bruce A. Feinberg, DO, vice president and chief medical officer, Cardinal Health Specialty Solutions, in his presentation entitled Practical Application of Clinical Pathways. Adding to that belief, the more that is spent on medical care, the more likely there will be increased wasteful spending. One way to get around these problems is to use pathways, because they can provide local peer-reviewed guidelines that allow clinicians to treat patients as they see fit. As a result, local clinicians will be better equipped to avoid unnecessary costs since their reference points for care will be local and they will be cognizant of the best way to efficiently treat each patient.
In that regard, Dr Feinberg compared clinicians with jazz musicians or chefs. A jazz musician will look at sheet music and a chef will look at a recipe before proceeding. But, both will use their training and experience to expand on what they see in front of them to create music or a meal that is unique to the surroundings. That is what guidelines/pathways can provide to clinicians—a means to provide peer-reviewed guidance while still focusing on the individual patient.
Pathways
“One of the great misconceptions about pathways is that somehow they represent some alternative universe—and they don’t. They are a subset of the universe,” said Dr Feinberg. To clarify, Dr Feinberg showed a graphic representation of the universe with areas that depicted the US Food and Drug Administration, the National Comprehensive Cancer Network (NCCN), and others. According to Dr Feinberg, pathways can stretch across those different regulatory bodies and create treatment guidelines that are specific to the clinician’s and patient’s part of the universe. To illustrate, he said that the NCCN guidelines for adjuvant HER2-negative, node-positive breast cancer has 16 regimens listed. However, most doctors only prescribe 3 or 4 of those regimens on a regular basis. Dr Feinberg’s employer, Cardinal Health, would ask the 300 or so physicians in a given provider network to agree to those same 3 or 4 regimens. By doing that, they believe there will be a reduction in treatment variance that further refines treatment and can lower costs.
Allowing Physicians to Be Physicians
Cardinal Health is working with physicians to establish them as democratic representatives of their network. Usually, a representative sample of about 12 local physicians (for a network there could be 100 to 300 physicians across the state or geographic area) will develop their own pathway in collaboration with the payer. Dr Feinberg said, “The goal is always best patient outcome.” Patient compliance is usually set at 80% for each pathway to allow a 20% leeway for those patients who will require a treatment that deviates from the pathway’s suggested treatment options.
Using this setup, all parties should “win.” Patients will see better outcomes with more refined care as physicians will be using a specific list of treatment options for a particular population. Also, payers will benefit from lower variance and less cost. Dr Feinberg thinks that pharmaceutical companies will like this model because it will provide a tremendous opportunity to increase accrual rates in clinical trials. He said, “If you have these networks, you have captive audiences to embrace clinical trials,” adding, “If we can decrease clinical trial accrual time in this country from 12 years to 6 years, we can halve the cost of drugs when they come to market.”
CareFirst Oncology
To illustrate the efficacy, safety, and cost savings of the pathways approach to healthcare, Dr Feinberg discussed the CareFirst Program. The program started in 2008 with 177 providers; by 2010, it had grown to 229. The key to the success of the program is compliance. In 2008, 77% of the practices were compliant; by 2012, 92% were compliant. Dr Feinberg added that the program only works if all parties are compliant. Therefore, “If a practice is noncompliant for 2 consecutive quarters, they get dropped, and if they then go back into compliance for 2 consecutive quarters, they’re allowed back in.”
In 2010, the first results from the program were presented at the American Society of Clinical Oncology (ASCO) annual meeting. Scott et al evaluated the potential cost savings of a payer-based “pay for quality” oncology program that applied clinical pathways.1 The analysis compared 57 participating practices (176 physicians, 10,432 patients) with 43 nonparticipating practices (194 physicians, 14,137 patients). The study determined that the estimated cost savings for anticancer drugs, supportive care drugs, and non-drug services was over $12 million. After adjusting for additional fees to participate in the program, the total yearly savings was over $8.5 million.
Second Generation
The second generation of CareFirst is a pilot program currently under way that mimics a medical home with the goals of: (1) shifting reimbursement from drugs to cognitive services; (2) aligning incentives; (3) developing a continuous quality improvement (CQI) program; and (4) developing an end-of-life care initiative.
With a reimbursement plan, there is a fee for service, and in oncology those fees are for cognitive patient care, chemotherapy administration, and reimbursement of drug. Given the increasing cost of drugs, those margins have swelled such that the margin on drugs accounts for up to 70% of the oncologist’s income. Policy makers are concerned that such reimbursement design incents more and more expensive (higher-margin) chemotherapy-prescribing behavior. The medical home model realigned incentives by moving the dollars related to drug margin to cognitive services, allowing participating physicians to remain financially whole but without generating income from the sale of drugs.
So far, 14 practices, comprising 31 physicians, in the Maryland/Washington, DC, area have volunteered. Dr Feinberg stated that this pilot program is interesting because there is a possibility that it will dramatically shift how patients are managed and how clinicians treat them. Some of the questions the study was designed to answer include: Will cognitive work increase and at what cost? Will the use of chemotherapy decrease? Will there be a shift away from brand drugs if there are no longer significant margins for brand drug delivery? Will the CQI program decrease emergency department visits and hospitalizations? And will there be an impact on end-oflife care? So far, these questions have not been fully answered, but Dr Feinberg provided some preliminary data from the pilot study. He cautioned, however, that due to the small sample size, the observed results cannot be considered statistically significant. One interesting observation was that the 31 physicians (in the aggregate) received 4.7% more reimbursement money compared with the year before (prior to joining the pilot program). If those physicians had been in the first-generation program, fees would have been 11% higher. However, when one dives deeper into the data from the aggregate to the individual practice level, there were clear winners and losers based on their patient mix. Dr Feinberg said, “This is where it’s really problematic when you look at this kind of modeling, because often it may make sense in the aggregate but it can break down dramatically when you get down to the specifics.” Further analysis demonstrated very little difference in physician prescribing behavior as both patient encounters and chemotherapy prescribing remained essentially the same despite the dramatic differences in reimbursement.
While the results from this pilot program may at first appear counterintuitive, it did provide: (1) validation of the unique medical home model among disparate providers; (2) evidence that significant savings (>3:1 return on investment [ROI]) can be achieved in a provider group already compliant with a mature pathways program (note: this was comparing the 4.7% increase in costs with the 11% increase that theoretically did not occur); and (3) a CQI program that directly and favorably impacted patient outcomes and ROI via reduced toxicities, emergency department visits, and hospital admissions.
Dr Feinberg noted that the pilot program will need further enhancements to sustain further savings, but he is very excited that the program can also be used as a springboard for better dialogue about end-of-life care. Whether or not the medical home concept can be exported across the entire plan remains to be determined, according to Dr Feinberg, but he is optimistic that some aspects of this program will lead to innovative programs in the future.
1. Scott JA, Wong W, Olson T, Fortner BV. Year one evaluation of regional pay for quality (P4Q) oncology program. J Clin Oncol. 2010;28(15 suppl):6013.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More

