- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
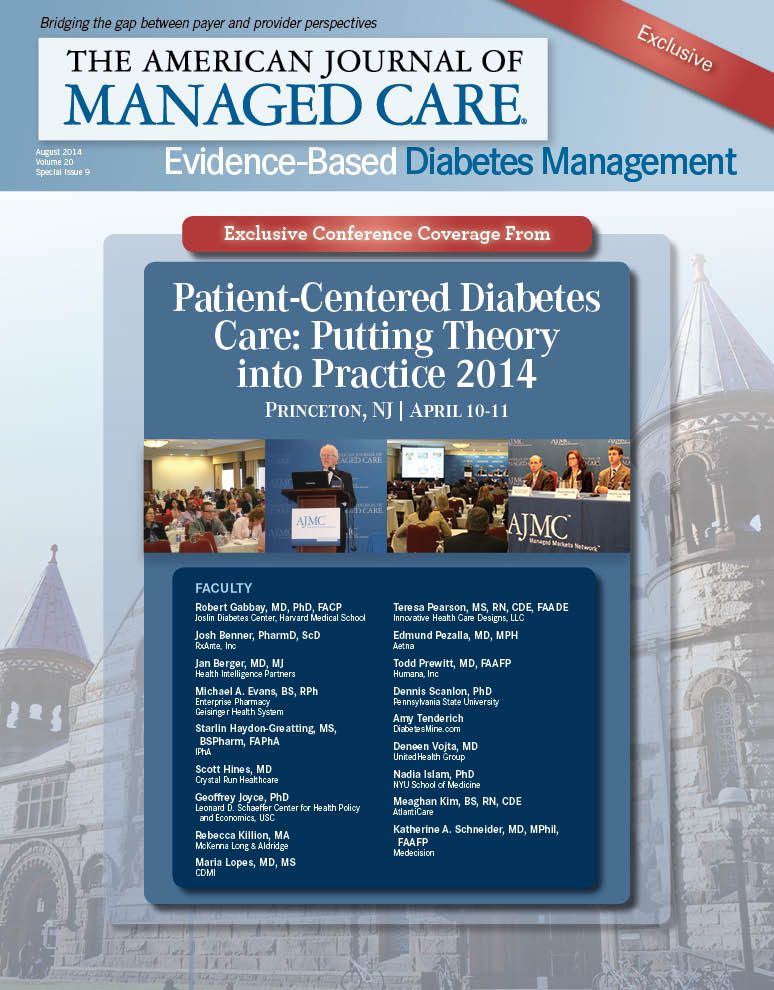
PCDC Recap
The second annual conference on Patient-Centered Diabetes Care left the audience with the message that diabetes continues to be a major healthcare issue. However, innovative healthcare management programs, which are patient-centric and involve all of the patient’s caregivers, can result in much improved disease management.
The special guest speaker, Jay Hewitt, a type 1 diabetes mellitus (T1DM) patient himself, amazed the audience with a narrative on how well he has managed to cope with, and at times win against, his condition. Managing diabetes is hard enough, but it’s a completely different ball game for an athlete. Citing his life experiences as a triathlon athlete, Hewitt emphasized the need for understanding and “respecting” the disease.
The speakers who participated in the first session addressed issues of health disparities among communities, improving medication adherence, and the use of technology for better disease management. Similar to what has happened in oncology, the realization has set in that one size does not fit all even with diabetes. The
faculty who participated in a panel discussion agreed that more individualized care could help improve the health of the population as a whole.
This was reiterated by the keynote speaker, Robert Gabbay, MD, PhD, who said physicians need to change their outlook—from a single patient model to a population model. He emphasized the need for regular quality assessments to improve care, and provided examples of various programs initiated at the Joslin Diabetes Center to improve models of care.
The sessions held on the second day of the meeting highlighted the importance of increased participation by various care providers, including integration of the pharmacist in diabetes patient care. The speakers stressed that the pharmacist is an untapped resource who can step in and provide many services of a traditional
EBDM
physician, as needed. The last panel discussion emphasized the changes brought about by accountable care organizations (ACOs) in diabetes care. Value-based care is always in the patient’s best interest, and ACOs can bring such care to the patient’s doorstep.
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
