- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Challenges in Diabetes: How to Focus on Individuals, Improve Health of Populations
During the first panel discussion at PCDC 2014, "Addressing Challenges in Diabetes," the panelists talked about individualizing patient care.
Every person with diabetes is different. Some with type 2 diabetes mellitus (T2DM) will be motivated to lose weight; many will not be. For some, T2DM is their main problem; for others, diabetes is just one of many health problems that must be managed at once.
Some patients with T2DM may be helped by advances that remind them to stick with diets and exercise, while those with type 1 diabetes (T1DM) have no use for wearing another gadget, according to one of their leading advocates.
The challenge of treating diabetes as healthcare reform takes hold, then, sometimes seems one of competing mandates: providers will increasingly be rewarded for improving the health of populations, yet the best solutions seem to be those tailored to the individual.
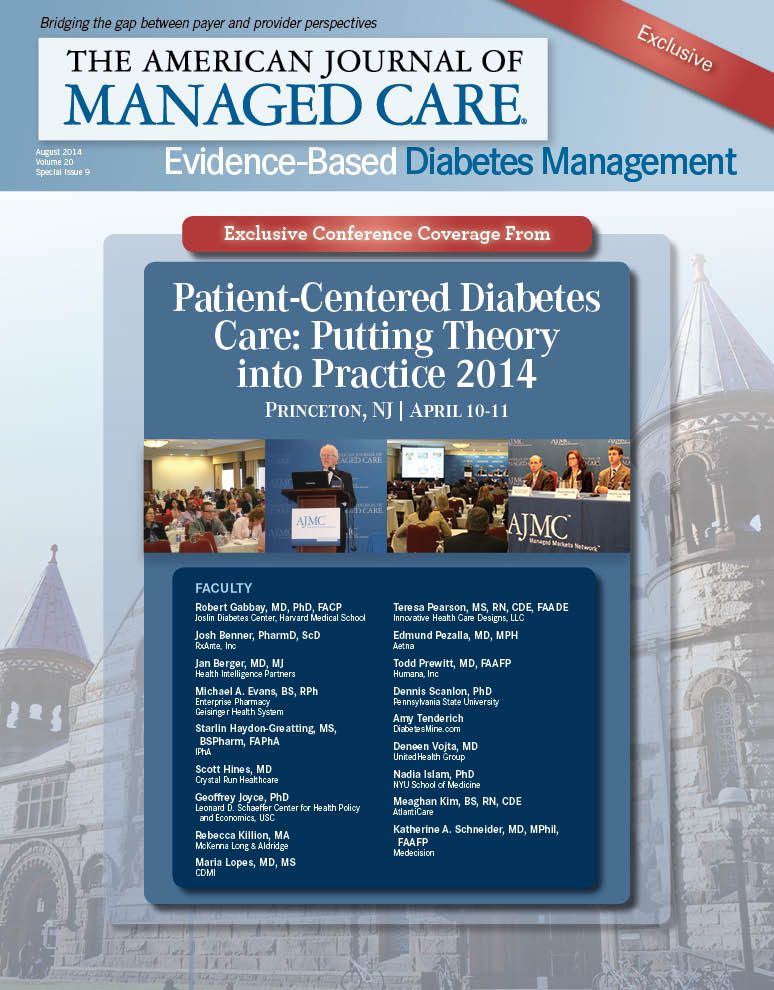
Josh Benner, PharmD, founder and president of the healthcare improvement group RxAnte, put his finger on this challenge during the panel discussion that followed the 2 presentations during the session, “Addressing Challenges in Diabetes.” This was first session of the meeting, “Patient-Centered Diabetes Care: Putting Theory into Practice,” which took place April 10, 2014, at the Princeton Marriott at Forrestal.
Amy Tenderich, founder and editor of DiabetesMine.com, said the challenge of treating diabetes starts with understanding what it means to live with the disease every day. Yes, persons with T1DM or T2DM are “patients,” but they also identify as professionals, parents, travelers, students, or other roles that have nothing to do with a disease. She challenged the audience to “think about what you did in the past 3 days, and then think about doing that with diabetes.”
The healthcare system, she said, doesn’t always grasp how hard it is to stay motivated on a specialized diet or exercise program, or how taxing it can be to constantly monitor devices attached to the body to avoid blood sugar levels that are too low or too high. “It’s a huge challenge,” Tenderich said. “It’s incredibly important to keep that in mind.”
“There’s a breakdown in the recognition of what the reality is of living with a chronic disease like diabetes,” she said, and if that reality were better understood by payers, providers, and the pharmaceutical industry, “we would have better solutions today.”
Solutions can start with data, and Maria Lopes, MD, MS, of AMC Health, said health plans often have plenty of it. The problem is taking the data and figuring out how to make it useful, both in managing individual cases and in tackling the disease among a group of patients. For example, “patient engagement” seems like an answer, but not if that means a patient gets multiple phone calls from different parts of the healthcare delivery system, all asking the same thing.
When payers think about the challenge of patient engagement, she said, they are thinking, “How do you make it scalable? How do you individualize that degree of scalability?” Payers must tailor programs to individuals, but they also deal with limited resources. That’s why the idea of a patient-centered medical home (PCMH) is so important, she said. “The physician still has 5 minutes to spend with the patient, but there are a lot of outbound calls—the behavioral interviewing, the motivational interviewing.”
These efforts will get at what’s behind the huge problem of nonadherence, Lopes said, and how best to direct resources. That’s why developing a personalized approach is so important, Benner added. “The past 2 decades of old-style disease management have proved to us that you can’t blast a population with a one-size-fits-all intervention and expect your problems to go away.”
Part of developing more personalized approaches means understanding changing demographics in the United States, including the arrival of new immigrant groups, the changing face of poverty, and the changing nature of the workforce, said Nadia S. Islam, PhD, of NYU Medical Center.
For example, 1 evidence-based diabetes prevention program supported in the literature has 16 core sessions and 22 recommended sessions. “How is that going to work for people working 6 to 7 days a week, 12 to 16 hours a day?” Islam asked.
One source of hope, said moderator Jan Berger, MD, MJ, of Health Intelligence Partners, is that diabetes has become a global struggle, and perhaps the solutions can be global as well.
Tenderich encouraged the panel to keep in the mind the perspective of the person with diabetes, who has to live with the disease every day. One “intervention”
that would cost nothing is for the person to get encouragement over time from his or her physician. “I don’t know anyone with type 1 who is an adult who hasn’t experienced clinical depression,” Tenderich said. “It is extremely difficult to stay motivated, and I think what we all lack is some sense of accomplishment.” More than all the technology and “apps,” she said, what would help most is rewards for patients who keep glycated hemoglobin (A1C) monitored and in check.
Lopes said health plans will look for evidence before they act. “We are spending a lot on patients who are diabetics, who are not at goal, who are on multiple drugs and still not at goal,” she said. Using clinical pathways and addressing “clinical inertia,” which will be needed when physicians are measured on how well patients do, are possible answers.
Islam agreed that innovations in treating diabetes would “have to go beyond technology.” Reaching the patients where diabetes is increasingly going to be concentrated means training workers who can meet specialized needs and gain patients’ trust. Berger agreed.
EBDM
“I actually think our largest challenge is the fragmentation and the segmentation of the people who are involved, in both the problem and the solution and the lack of trust,” Berger said. “If we all sit down and talk, we’ll learn that maybe we have more in common than we have (qualities) that are different.”
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Exploring Pharmaceutical Innovations, Trust, and Access With CVS Health's CMO
July 11th 2024On this episode of Managed Care Cast, we're talking with the chief medical officer of CVS Health about recent pharmaceutical innovations, patient-provider relationships, and strategies to reduce drug costs.
Listen

