- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
On-Body Delivery System enFuse Saves Time, Improves QOL for Patients
An on-body delivery system approved last fall for paroxysmal nocturnal hemoglobinuria (PNH) has seen rapid uptake and is now being studied for use with isatuximab.
Improving cancer care isn’t just about extending survival or reducing the likelihood of fevers or nausea after treatment. Engineers and designers are joining physicians in helping patients regain not only their health, but something that cannot be recaptured once lost: their time.
Hours spent in infusion chairs is so well documented as a downside of treatment that authors dubbed it “time toxicity” in a 2022 article.1 However, even as subcutaneous (SC) delivery gains popularity in cancer and other conditions, due to cost savings for payers and the time savings for patients,2 there are some patients who balk at certain SC methods due to fear of needles.3
On-body delivery systems (OBDS) address these concerns by combining speed and mobility, while addressing the “human factors.” Patients attach the drug container to the body for discreet injection. A decade ago, the convenience of OBDS in cancer care gained notice with the arrival of Neulasta Onpro, which was placed on patients after chemotherapy and delivered a dose of infection-preventing pegfilgrastim the following day, thus eliminating a return trip to the clinic or hospital.4
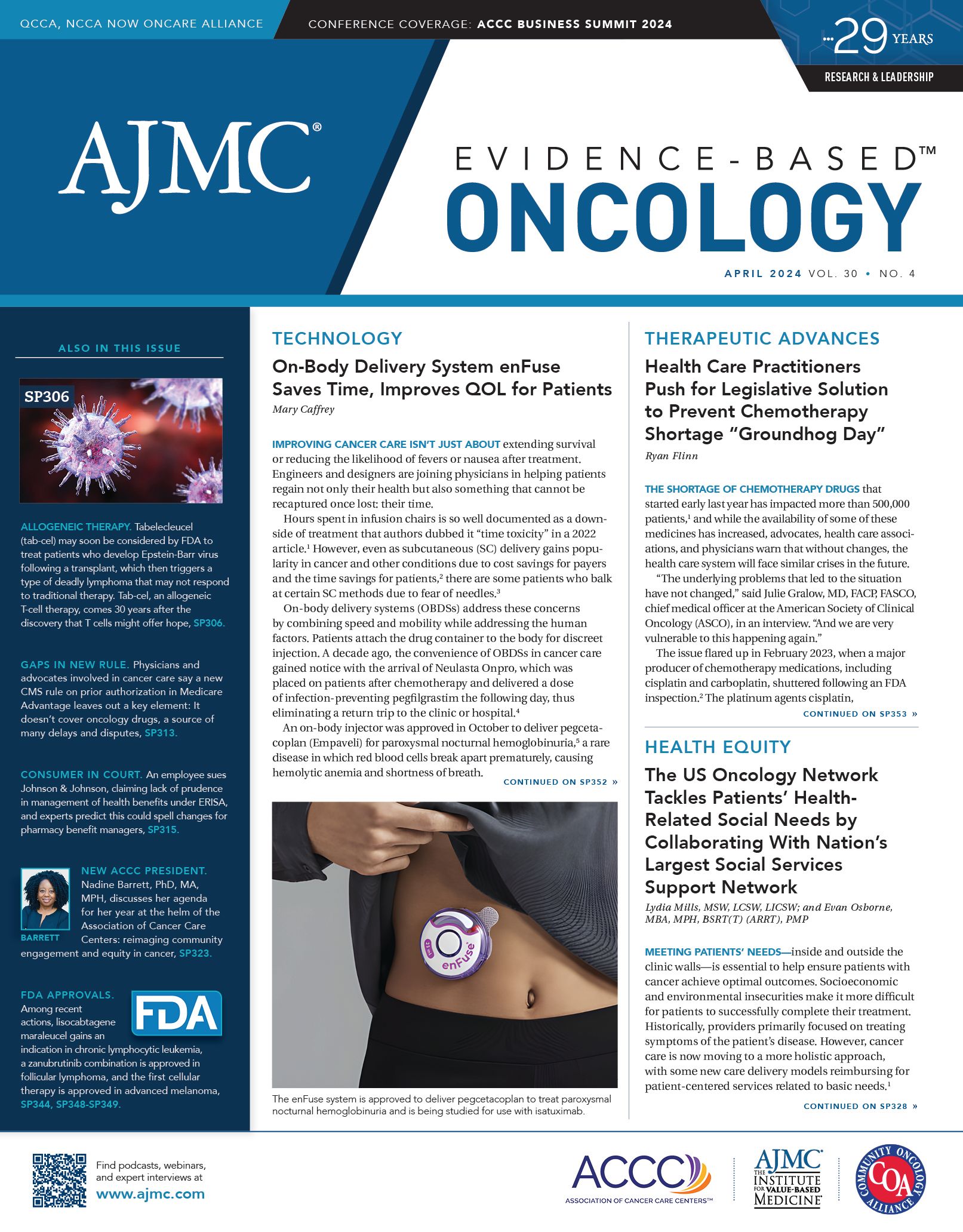
enFuse injector | Image credit: Enable Injections

An on-body injector was approved in October to deliver pegcetacoplan (Empaveli) for paroxysmal nocturnal hemoglobinuria (PNH)5, a rare disease in which red blood cells break apart prematurely, causing hemolytic anemia and shortness of breath. After only 4 months, the device is being used by 60% of existing patients and more than 90% of new patients, according to this morning’s earnings call with Apellis Pharmaceuticals,6 which reported patient compliance is up to 97%.
This device, the enFuse injector by Enable Injections, is now being studied as a SC option for isatuximab (Sarclisa), an anti-CD38 monoclonal antibody for patients with relapsed/refractory multiple myeloma (RRMM). Isatixumab has distinct clinical features separating it from daratumumab, but unlike daratumumab, it is not currently approved in an SC formulation.7 The enFuse injector is also being studied for use with FcRn (neonatal crystallizable fragment receptor) inhibitors to treat immunoglobulin G (IgG)-mediated autoimmune disorders.8
The enFuse Injector
Enable Injections’ enFuse product is a palm-sized plastic disc the weight of a ballpoint pen. Company officials described the approved single-use Empaveli injector as “the first purely mechanical, large volume, on-body subcutaneous drug delivery device.”5
Mehul Desai, PharmD, MBA | Image credit: Enable Injections

The simple-looking injector took 12 years to develop, combining years of research into earlier devices. “A good way to think about enFuse is that it’s a wearable injector, and it combines the ease of use of an auto-injector with the volume capacity of a pump. It’s not very easy to create something like that,” said Mehul Desai, PharmD, MBA, vice president, medical/clinical affairs, Enable Injections, in an interview with The American Journal of Managed Care®.
Desai explained that developing the current design meant moving away from other devices with a 3.5-mL capacity to one with 5 to 25 mL, which would align with active intravenous (IV) drug volumes—but take IV volumes to SC.
“We did that while also being the smallest injector with the largest capacity, but also trying to be the one that’s purely mechanical,” Desai said, “because sustainability matters when you’re treating chronic conditions.”
This was the most challenging part, he said, because it required “inventing something totally new.”
enFuse transfer system | Image credit: Enable Injections

The system uses a transfer device that allows either the patient or a health care provider to directly deliver the original vial of therapy into the on-body disc, eliminating waste and added costs. Other products have a custom container, which Desai said can add $10 million to $25 million in costs and 12 to 24 months of labor, delaying a launch. Once the empty disc is filled with therapy, the patient places it on the abdomen, where it stays in place with adhesive. The patient presses a button that inserts the needle and starts the injection, so the patient never sees the needle. When the injection is complete, the needle pops out and he patient removes the single-use device and throws it away.
Each FDA approval will be therapy specific, he said, so whether a patient can use the injector at home or with a health care provider at a clinic will depend on the therapy involved, not the device. Cancer therapies might be administered in a clinic for safety reasons, but patients would still be able to move around during delivery.
Strong Payer Interest
Results of a payer survey showed that 90% of payers felt that the OBDS fulfilled an unmet medical need, with the ease of use and the hidden needle cited in particular.9
“The most interesting finding was that 82% stated that they would actually pay a premium for a drug delivered with the enFuse vs a standalone vial format—and these premiums ranged from 5% to 20%,” Desai said.
Just as the Empaveli injector was approved as a combination product, Desai explained, any new uses would be approved following separate trials with each therapy and the injector.
“The benefit to us going this route—and getting the combination product status—is that there’s no separate billing, because it’s not separate medical equipment; it’s billed the same as an auto-injector,” he explained.
When conducting clinical trials, he added, “the drug is already [subcutaneous]; it’s a much more abbreviated pathway.”
Lissa Pavluk, spokesperson for Apellis, confirmed in an email that the device is provided by Apellis “at no cost to the patient, payer, and provider.”
Results for Isatuximab
Final results for a phase 1b study (NCT04045795) involving 56 patients with RRMM were presented at the International Myeloma Society (IMS) meeting in September 202310; these data covered patients treated with isatuximab plus pomalidomide and dexamethasone, including 12 patients treated with IV isatuximab 10 mg/kg, 12 treated with isatuximab SC infusion pump (IP) 1000 mg, 10 with isatuximab SC IP1400 mg, and 22 treated with isatuximab OBDS, administered by a health care provider. Patients had a median follow-up of 33 months for the IV group, 39 months for the IP1000 group, 33 months for the IP1400 group, and 19 months for the OBDS group.
No patient stopped isatuximab early due to a treatment-emergent adverse event (TEAE); 5 patients (2, IP1000, and 3, IP1400) and 6 patients (1, IP1000; 3, IP1400; and 2, OBDS) stopped pomalidomide and dexamethasone, respectively, due to a TEAE. Two patients in the OBDS group died, 1 in complete response had a cardiorespiratory arrest not related to treatment, and another had treatment-related Listeria-related meningitis.
The median duration of OBDS injections was 10 minutes. All OBDS injections were completed without interruptions. Local tolerability was good; 7 patients (32%) had 10 injection site reactions, all grade 1 across 581 administrations (1.7%). In terms of efficacy, the overall response rate was comparable between the IV and SC groups: 66.7% in IV, 66.7% in IP1000, 80% in IP1400, and 72.7% in OBDS.
Among 8 patients who received isatuximab via OBDS and completed a questionnaire, 7 patients (87.5%) said they were very satisfied or satisfied and very confident or confident in the treatment approach. None found the administration method painful. As a result of these findings, a phase 3 study (NCT05405166) is ongoing.10
For Patients, Device Fits in With Lifestyle
Jennifer Estep | Image credit: LinkedIn

For conditions that do not require clinic oversight during treatment, patients can use the injector without interrupting their daily activities, said Jennifer Estep, Enable Injections senior director for global marketing & commercial strategy.
“Normally, the syringe pump would take some time to set up with needle sets, etc,” Estep said. “We heard from a patient who recently switched to the Empaveli injector. He and his wife were out to dinner and went back to their friends’ house. And they’re sitting having a glass of wine, and [the patient] knew he needed to do his injection. Usually, he has to stop everything to do this. Instead, he went into the kitchen, did his enFuse, applied it to his stomach, pressed the button, and went back and joined his friends. No one noticed he had left. He felt the button pop, which is silent.”
About an hour later, she said, the man’s wife asked, “Weren’t you supposed to do your injection?”
“He said, ‘I’ve already done it.’ For him that was a major triumph,” Estep said. “We’re really excited about stories like that.”
References
- Gupta A, Eisenhauer EA, Booth CM. The time toxicity of cancer treatment. J Clin Oncol. 2022;40(15). doi:10.1200/JCO.21.0281
- Harvey MJ, Zhong Y, Morris E, et al. Assessing the transition from intravenous to subcutaneous delivery of rituximab: benefits for payers, health care professionals, and patients with lymphoma. PLoS One. 2022;17(1):e0261336. doi:10.1371/journal.pone.0261336
- Bolge SC, Eldridge HM, Lofland JH, et al. Patient experience with intravenous biologic therapies for ankylosing spondylitis, Crohn’s disease, psoriatic arthritis, psoriasis, rheumatoid arthritis, and ulcerative colitis. Patient Prefer Adherence. 2017;11:661-669. doi:10.2147/PPA.S121032
- Mahler LJ, DiBlasi R, Perez A, Gaspard J, McCauley D. On-body injector: an administration device for pegfilgrastim. Clin J Oncol Nurs. 2017;21(1):121-122 doi:10.1188/17.CJON.121-122
- Enable Injections receives first US Food and Drug Administration approval. News release. PR Newswire. October 2, 2023. Accessed February 27, 2023. https://www.prnewswire.com/news-releases/enable-injections-receives-first-us-food-and-drug-administration-fda-approval-301943533.html
- Apellis Pharmaceuticals reports fourth quarter and full year 2023 financial results. News release. Apellis Pharmaceuticals. February 27, 2023. Accessed February 27, 2023. https://investors.apellis.com/news-releases/news-release-details/apellis-pharmaceuticals-reports-fourth-quarter-and-full-year-5
- Shen F, Shen W. Isatuximab in the treatment of multiple myleoma: a review and comparison with daratumumab. Technol Cancer Res Treat. 2022;21:15330338221106563. doi:10.1177/15330338221106563
- Viridian Therapeutics announces partnership with drug delivery innovator Enable Injections. News release. Enable Injections. May 8, 2023. Accessed February 27, 2024. https://enableinjections.com/viridian-therapeutics-announces-partnership-with-drug-delivery-innovator-enable-injections/#:~:text=(NASDAQ%3A%20VRDN)%2C%20a,volumes%20of%20up%20to%2025mL.
- Desai M. Exploring US payer perspectives on a large-volume subcutaneous on-body delivery system: a double-blinded preference study. Presented at: 2023 PDA Universe of Pre-filled Syringes and Injection Devices Conference; October 17-18, 2023; Gothenburg, Sweden.
- Hang Q, Parmer G, Ocio EM, et al. Final results of a phase 1b study of subcutaneous isatuximab: administration of an on-body delivery system (OBDS) plus pomalidomide and dexamethasone in R/RMM. Presented at: International Myeloma Society; September 27-30, 2023; Athens, Greece, Abstract P-306.