- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
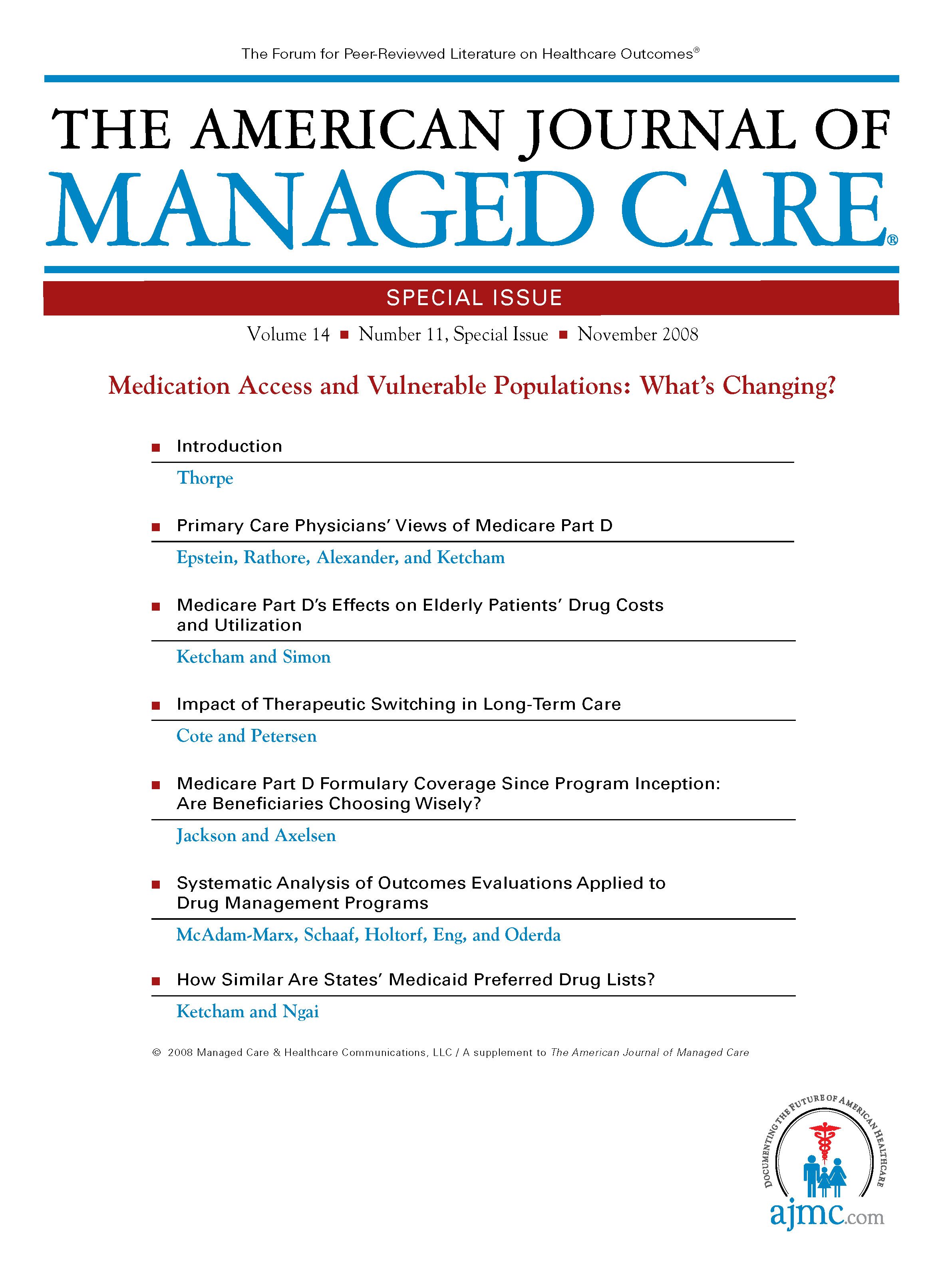
Introduction
Nearly 3 years have passed since the implementation of the Medicare prescription drug benefit, Part D, which subsidizes beneficiaries’ drug costs. Out-of-pocket drug costs are one of the most significant barriers to prescription adherence. Part D has provided important access to needed medicines for millions of beneficiaries, particularly low-income seniors and those without drug coverage prior to Part D, who generally paid the highest prices for prescriptions.
Beneficiaries who want to enroll in this benefit can choose to join a stand-alone prescription drug plan (PDP) or to receive their drugs along with their medical care in a Medicare Advantage plan that provides a Part D benefit (MA-PD). One segment of the Medicare population was automatically enrolled in the PDPs in the new program, the low-income beneficiaries eligible for both Medicare and Medicaid (the so-called “dual eligibles”), who formerly received drug benefits from state Medicaid programs. These beneficiaries account for roughly 29% of all Part D enrollees. Many beneficiaries in nursing homes are dual eligibles and experienced a change in benefits when they were enrolled in PDPs.
Enough time now has passed to allow for a meaningful examination of Part D’s effects. The benefit was projected to add $49 billion to Medicare outlays in 2007 ($40 billion net of state payments and beneficiary premiums). That alone makes it a vital policy topic, particularly in our current economic environment. Aside from finances, the central question is: How has Part D affected beneficiaries, both those with new drug coverage and the particularly vulnerable dual-eligible beneficiaries whose prior source of drug coverage was replaced by Medicare Part D? How has it affected their health and healthcare?
This special issue includes a number of studies that investigate the impact of Medicare Part D. Epstein et al’s survey of physician attitudes toward Medicare Part D reveals that primary care physicians have a favorable view of Part D overall, although their impressions of access depend on whether a patient had prior drug coverage.1 If beneficiaries had prior Medicaid drug coverage, there is the sense that Part D is not as generous, although negative sentiments are not as strong for physicians practicing in states with very restrictive Medicaid formularies. Other analyses have shown that Part D coverage in the largest PDPs is less restrictive than many state Medicaid preferred drug lists; Epstein et al’s survey results might reflect the existence of multiple PDP formularies, any one of which could be more restrictive than the single state’s preferred drug list for a specific drug or class.
Ketcham and Simon examine how the availability of Medicare drug coverage for seniors has changed their drug utilization and out-of-pocket costs.2 They found that utilization by Medicare-eligible seniors increased significantly relative to utilization by older nonseniors after implementation of Part D and that out-of-pocket costs for prescription drugs were reduced significantly -- strong evidence that Part D is having a positive effect on many Medicare beneficiaries.
The article by Cote and Petersen exposes the risks of therapeutic switching in the long-term care setting.3 Their survey of nurses, physicians, and pharmacists working in nursing homes reveals that many of the nonmedical therapeutic switches for Part D beneficiaries that resulted from the adoption of a PDP formulary in place of the specialty pharmacy formulary led to reduced efficacy. Switching institutionalized patients away from drugs on which they have been stabilized to comply with a new formulary can be medically risky, especially for patients with certain conditions such as heart disease, HIV, and bipolar disorder.
Jackson and Axelsen’s study points out the need for special precautions for dual-eligible patients.4 Dual eligibles are automatically assigned to a PDP that meets certain cost criteria, although they have the option of self-enrolling in the PDP of their choice. The Jackson and Axelsen analysis reveals that random assignment into plans for dual-eligible beneficiaries may not provide the best coverage for drugs most used by low-income beneficiaries. This analysis suggests that some dual eligible beneficiaries could receive better coverage by switching to another plan, but most do not. Given that these seniors typically have less education and fewer resources for decision assistance, they may need additional support to re-enroll in an eligible plan offering coverage of their needed medications.
The 2 remaining articles in the special issue focus on the critical issues associated with management of Medicare Part D benefits. The article by McAdam-Marx et al suggests a dearth of quality impact analyses of drug utilization management programs.5 Most studies consider either economic outcomes or patient outcomes such as clinical or humanistic endpoints, but few integrate both types of outcomes, without which quality impact cannot be accurately measured. This finding should spur more comprehensive analyses in the future. Finally, Ketcham and Ngai compare Medicaid preferred drug lists and find very little consistency in coverage decisions across states.6 Their research serves as a warning that any national entity that might eventually be charged with making coverage decisions for the entire Part D program would be susceptible to the same challenge of correctly interpreting clinical evidence.
In summary, these 6 articles suggest that, although Medicare Part D can be considered successful on a number of fronts, a few cautionary lessons can be drawn. These lessons should be seriously considered by policy makers as they debate changes to the Part D program.
Author Affiliation: From the Department of Health Policy and Management, Emory University, Atlanta, GA.
Funding Source: None reported.
2. Ketcham JD, Simon KI. Medicare Part D’s effects on elderly patients’ drug costs and utilization. Am J Manag Care. 2008;14(11 Spec No.):SP14-SP22.
4. Jackson EA, Axelsen KJ. Medicare Part D formulary coverage since program inception: are beneficiaries choosing wisely? Am J Manag Care. 2008;14(11 Spec No.):SP29-SP35.
6. Ketcham JD, Ngai JK. How similar are states’ Medicaid preferred drug lists? Am J Manag Care. 2008;14(11 Spec No.):SP46-SP52.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

