- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Model Accurately Predicts SCD Pain Scores Using Apple Watch Data
Patients with sickle cell disease (SCD) who wore an Apple Watch and reported daily pain scores could have their pain scores accurately predicted during hospital admission for vaso-occlusive crises and after discharge.
Patients with sickle cell disease (SCD) who had vaso-occlusive crises (VOC) that required hospital admission could have their high pain scores accurately predicted during admission and after discharge through wearing an Apple Watch, according to a study published in Frontiers in Digital Health.
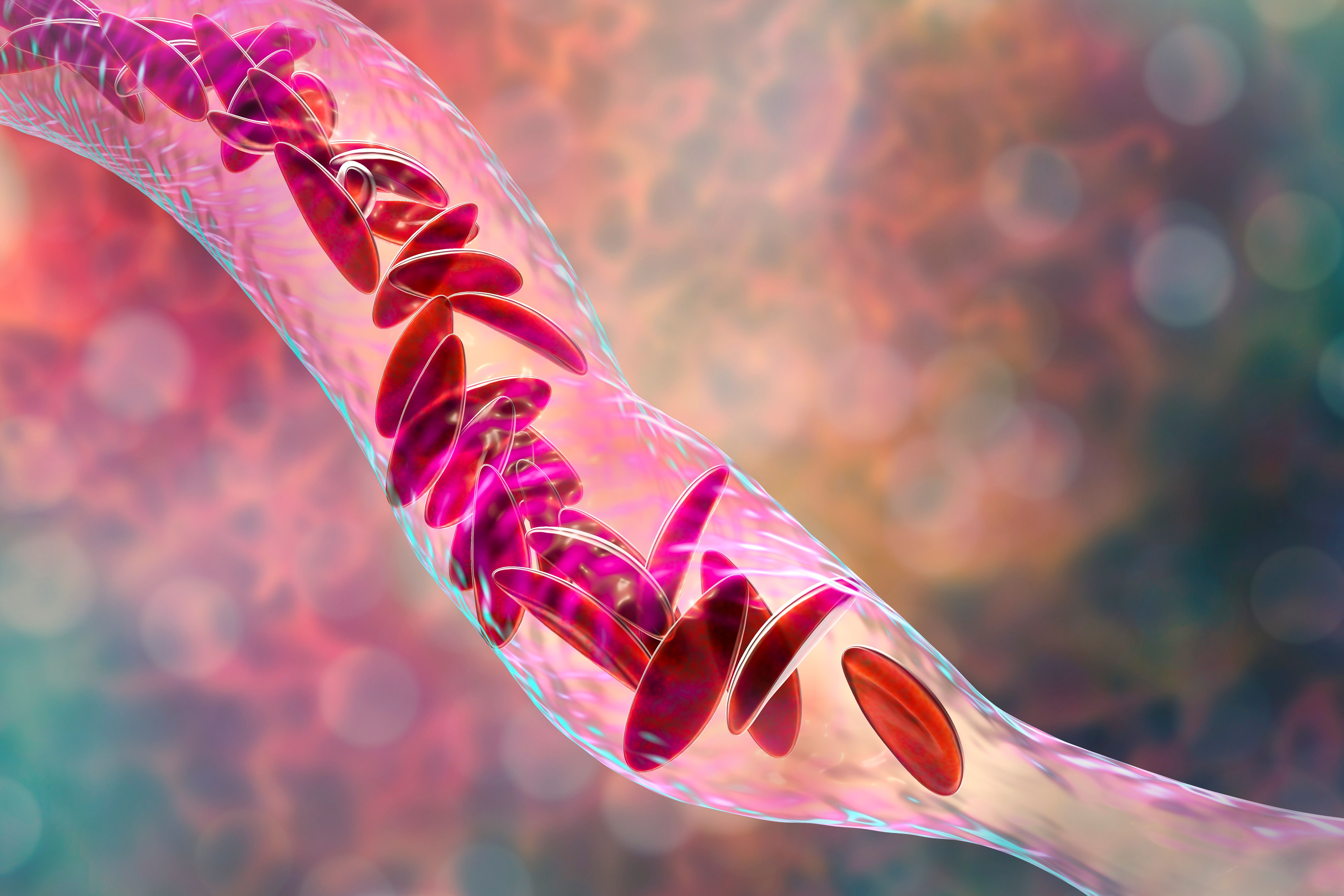
SCD is a severe red blood cell disorder that affects 20 million individuals around the world. VOCs, which are recurrent episodes of acute and severe pain, are the most common complication of SCD, and they can affect any part of the body. Treatment of VOCs often starts at home but could require hospitalization if home remedies fail. Predicting VOCs is near impossible as there are no reliable tests to diagnose or predict their occurrence. This study aimed to evaluate a machine learning model that predicted pain scores by extending the monitoring to 30 days after discharge and by refining the development of machine learning models.
Sickle cell anemia, 3D illustration. | Image credit: Dr_Microbe - stock.adobe.com
Patients were eligible for this study if they had SCD, were 18 years or older, and received care at Duke University Hospital. Patients who were admitted for a VOC between April and June of 2022 were eligible. Participants enrolled in the study during hospitalization and up to 30 days after their discharge. All participants received the mobile app of Nanbar Health on their Apple iPhone and/or an Apple Watch series 3. Patients were to report pain scores daily and were asked to wear the Apple Watch at all times. Patients were also contacted once a week as a reminder to record pain scores. Demographic information was collected from all participants.
Pain scores were reported on a scale of 0 to 10, with 0 being no pain and 10 being intense pain. The Apple Watch also collected heart rate, heart rate variability, resting heart rate, average heart rate, and step count for every participant. The machine learning models were also compared with 2 null models, a random model, and a mode model.
There were 19 patients included in this study who had a median (IQR) age of 30 (22-34) years and 58% of whom were women. The median (IQR) duration of hospital stay was 5 (2-9.8) days. Acute chest syndrome was not seen in any of the patients, although 1 patient required oxygen; all of the patients were treated with opioids. A total of 74% of patients needed medical care after discharge for pain.
There was a median (IQR) of 79 (16-142) pain data points per participant, with a total of 2395 pain data points when combining pain points recorded in the electronic medical record and the app. The patients most frequently reported a pain score of 7, with no responses of 0 or 1. Patients wore their watch a median (IQR) of 28 (22-34) days.
The machine learning models had accuracy that outperformed the null models. An accuracy of 92% was found in the random forest model, with a micro-averaged F1 score of 0.63, an area under the curve of 0.9, and a root-mean-square error of 1.1. The highest cross-validation accuracy was also found in the random forest model (62%), which had the lowest SD (0.7%). These scores indicated that the random forest model was most likely to outperform all other models. Step count (>0.30) and resting heart rate (<0.20) had the highest feature importance when calculating pain score risk through the random forest model.
There were some limitations to this study. There were a small number of participants who self-reported their pain data, which meant that the study could not stratify by SCD genotype and type of pain.
The researchers concluded that the Apple Watch represents a useful, noninvasive, and patient-friendly method of collecting data in patients with SCD. This data collection could help with early detection of a VOC and other acute pain to better treat patients with SCD in a variety of locations due to its accessibility.
Reference
Vuong C, Utkarsh K, Stojancic R, et al. Use of consumer wearables to monitor and predict pain in patients with sickle cell disease. Front Digit Health. Published online October 25, 2023. doi:10.3389/fdgth.2023.1285207
