- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Medical World News, February 2017
MANAGED CARE
Getting Insured Could Reduce Cancer-Related Deaths Among Minorities
A new report from the American Cancer Society (ACS) indicates that while the cancer-related death rate was higher among blacks than whites in 2014, this racial gap could narrow as minority patients increasingly gain access to insurance and healthcare. The claim is based on the fact that the number of uninsured black Americans fell by 50% between 2010 (21%) and 2015 (11%). A similar trend was noted among Hispanic Americans; the group saw a decrease from 31% to 16%. The authors noted the effect of the Affordable Care Act (ACA) on these improvements.
ACS collected incidence and mortality data from 1930 to 2014 from the National Center for Health Statistics. National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program and CDC’s National Program of Cancer Registries are the sources for long-term cancer incidence data. Long-term incidence and survival trends were based on data from 9 SEER areas representing 9% of the US population; 18 SEER registries were used to gather data on the lifetime risk of developing cancer, stage, distribution, and survival by stage, as well as data on children and young adults, which covered 28% of the population.
The report projects a daily diagnosis of 4600 new cancer cases in 2017, which would lead to 1,688,780 new cases of cancer in 2017; this includes 63,410 cases of breast carcinoma in situ among female patients and 74,680 cases of melanoma in situ. More women (852,630) are estimated to be diagnosed with cancer in 2017 than men (836,150); however, mortality is estimated to be higher among men than women. Of the nearly 601,000 cancer-related deaths in the coming year, 318,420 deaths are forecasted to be among men diagnosed with cancer and 282,500 among women.
More men than women are expected to be diagnosed with specific cancer types in 2017, and the trend holds across subtypes, except for breast cancer. With more than 250,000 women expected to receive a breast cancer diagnosis in 2017, women surpass men in overall cancer incidence. As for the death rate, the report states that cancers of the genital system and endocrine system will see more deaths among women than men—all other cancer types are predicted to increase mortality in men.
Among the states, California and Florida lead the tally on new cases in 2017, with both expected to have a high rate of female breast cancer incidence. Florida also has a high projected rate of new lung and bronchial cancers. Cancers of the lung and bronchus, colorectum, and prostate in men and lung and bronchus, breast, and colorectum in women will be the most common causes of cancer deaths in the country in 2017.
The report notes an overall upward trend in the 5-year survival rate over the past 30 years: survival has increased by 20 percentage points among whites and 24 percentage points among blacks, with the most pronounced improvements seen in the 50-to-64 age group. Hematologic malignancies have seen rapid progress due to better treatment protocols and the discovery of targeted therapies, the report states.
Another important finding of the report is the closing gap in racial disparity. The difference in the cancer death rate was at a peak in 1990, with the excess risk growing to 47% in black men compared with white men, the report states. It dropped to 21%, however, in 2014, which could be due to a sharp decline in smoking initiation in the black population overall. A similar trend was observed in women of both races. The authors note that after the ACA took full effect, the number of uninsured among the minority population dropped. “If maintained, these shifts should help expedite progress in reducing socioeconomic disparities in cancer, as well as other health conditions,” they wrote.
Reference
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7-30. doi:10.3322/caac.21387.
Will the Absence of Certain Cancer Centers on Insurance Exchanges Impact Outcomes?
The Affordable Care Act weaved in several provisions to improve access to health insurance within the United States—Medicaid expansion, online exchanges, and allowing young adults (until 26 years) to remain on their parent’s plans, among others. However, narrow provider networks within these federal exchanges have raised questions about access to care. According to new study results from The University of Texas, a majority of these exchanges do not include National Cancer Institute (NCI)-designated centers, which, the authors believe, might create a barrier for access to clinical trials and specialized care.1
Studies have shown that federal exchanges either have narrow provider networks or there are restrictions on certain categories of physicians or hospitals, if the regional provider network is broad, which can be a barrier for patients with complex care needs for diseases such as cancer. Although health plans are required to cover the costs of participating in a clinical trial, they are not bound to do so for out-of-network costs. Under these circumstances, the absence of NCI-designated cancer centers from exchanges could prevent patients from receiving innovative treatments currently under development in oncology.
For their study, the researchers extracted provider network data for the 2016 enrollment year, available as of December 2015. They characterized the networks that included Commission on Cancer (CoC)-accredited hospitals and NCI-designated cancer centers. Of the 4058 individual plans, network data were available for 3637 (90%) and hospital information for 3531 (87%). Of the 295 unique networks that were identified, 95% included at least 1 CoC-accredited hospital, but only 41% included NCI-designated centers. The plan type was also a determinant of whether an NCI-designated center would be included in the network: 31% of health maintenance organizations and 49% of preferred provider organizations included them, independent of the metal level of an individual plan. As the authors expected, networks available in states and counties where the NCI-designated cancer centers were located were more likely to include the center, although only half did so. The authors feel that their findings indicate lack of access to cancer care, and they reinforce the need to promote access to specialized care and clinical trials at community sites.While the question about access might hold true, do accredited cancer centers really improve patient outcomes? Not according to study results that were published in 2014,2 which showed that whereas accredited cancer centers performed better on most process and patient experience measures, they came up short on most outcome measures. So, when policy makers consider improving access for patients enrolled on marketplace exchanges, they need to be aware of the differences in outcomes among the various sites of care.
References
1. Kehl KL, Liao KP, Krause TM, Giordano SH. Access to accredited cancer hospitals within federal exchange plans under the Affordable Care Act [published online January 9, 2017]. J Clin Oncol. 2017. doi: 10.1200/JCO.2016.69.9835. 2. Merkow RP, Chung JW, Paruch JL, Bentrem DJ, Bilimoria KY. Relationship between cancer center accreditation and performance on publicly reported quality measures. Ann Surg. 2014;259(6):1091-1097. doi: 10.1097/SLA.0000000000000542.
Patient and Provider Education on Pain in Cancer: A Cost-saving Intervention
An experiment by an integrated healthcare delivery system to document personalized pain management goals (PPGs) for patients in oncology clinics lowered documented pain and simultaneously reduced treatment costs. While achieving a pain level of 0 may not be possible, the authors suggest that achieving the patient’s PPG is a good start.
As part of Park Nicollet Health Services quality-improvement course, a team that included a medical oncologist, oncology nurse practitioner, oncology nurse, pharmacist, statistician, computer programmer, and quality-improvement leaders documented pain values from the electronic health records (EHRs) of oncology patients in the outpatient clinics. This information included:
- Pain levels during a predetermined 18-month period
- Reporting and achievement of PPG
- Monthly tabulation of opioid prescriptions
Following analysis of this data, the researchers introduced a pain intervention that included patient education on pain management (using a handout), clinician education on opioid cost-effectiveness, and instituting a nursing protocol to document PPGs. The patient education handout detailed appropriate opioid use and the complications associated with using opioids, such as constipation. Physician education included a combination of a discussion with a palliative care physician and cost information data on various opioids extracted from a hospital pharmacy.
The study determined that 15% of patient encounters reported moderate to severe pain. Whereas PPGs were marked at 16% prior to the pain intervention, in June 2014, they crossed the 70% mark 1 year after its introduction in the oncology clinic, in June 2015. The authors write that the actual achievement of a PPG per EHR data was at 84% at the time.
Prescribing practices saw a simultaneous change, too, with a significant downturn observed in the prescription of high-cost opioids following clinician education on their cost. While low-cost and high-cost opioids were prescribed at the same rate prior to the intervention, June 2015 saw double the number of low-cost opioid prescriptions (n = 71) compared with high-cost prescriptions (n = 35)—a 10% drop in the prescription of high-cost opioids.
The authors believe that a PPG is a much better strategy over the standard pain measure that is commonly used in oncology clinics, considering that each patient will have unique pain thresholds, writing that PPGs can improve patient satisfaction because they signify to the patient that their physician is listening to their concerns and is focused on providing them with personalized quality care. The authors also note an indirect impact of the intervention on workflow efficiency and a shift in the nurses focus away from prior-authorization requests (due to the use of low-cost opioids) toward patient care. An average saving of 90 minutes that a nurse has to spend on processing prior authorizations (at least 3 of these each week) is 90 minutes added to patient care, the authors point out.
The researchers plan to track patient-reported outcomes through a symptom-assessment tool that exports data to the patient’s EHR for use at the point of care and to auto-generate flags on uncontrolled pain and underlying causes for why patients need to continue treatment on high-cost medications.
Reference
CLINICAL
NCI Formulary a Big Support for Cancer Moonshot
Zylla D, Larson A, Chuy G, et al. Establishment of personalized pain goals in oncology patients to improve care and decrease costs [published online January 3, 2017]. J Oncol Pract. 2017. doi: 10.1200/JOP.2016.017616.  
Described as a public—private partnership between the National Cancer Institute (NCI) and pharmaceutical and biotechnology companies, the NCI Formulary1 has been created with the expectation that it will provide researchers rapid access to anticancer drugs for use in clinical trials. This resource would be particularly valuable for researchers trying to use combination therapies that incorporate agents manufactured by different pharmaceutical companies, which, in turn, can have a big impact on patient outcomes and help get drugs to patients much faster—one of the objectives of former Vice President Joe Biden’s Cancer Moonshot Program.2
The NCI has developed a process that will eliminate the often lengthy negotiations that occur between academic researchers and pharmaceutical manufacturers. Investigators at NCI-designated cancer centers can use the agents within this formulary to conduct clinical trials on investigator-held investigational new drugs and for pre-clinical research. NCI’s mediation is expected to streamline and smoothen the process for these researchers. Currently, 6 pharmaceutical companies have partnered with NCI and contributed 15 targeted anticancer agents to the formulary (Table).
“The agreements with these companies demonstrate our shared commitment to expedite cancer clinical trials and improve outcomes for patients,” James Doroshow, MD, deputy director for clinical and translational research, NCI, said in a press release. “It represents a new drug development paradigm that will enhance the efficiency with which new treatments are discovered.”
The formulary has drawn inspiration from NCI’s Cancer Therapy Evaluation Program and the NCI-MATCH trial. The study design of NCI-MATCH requires agents from multiple drug manufacturers, tested alone or in combination after matching a patient’s mutation pattern. Doroshow expects the number of pharmaceutical partnerships and drugs to double by the end of 2017.
A report developed by the blue-ribbon panel of experts appointed by Biden had identified a lack of collaboration and the slow dissemination of discoveries and clinical data as some of the barriers to improving cancer delivery in the United States. Partnerships spearheaded by institutions like the NCI could help overcome some of them.
References
1. NCI formulary: a public-private partnership. National Cancer Institute website. https://nciformulary.cancer.gov/. Accessed January 18, 2017.
2. Dangi-Garimella S. Vice President Biden delivers Cancer Moonshot report to the nation. The American Journal of Managed Care™ website. http://www.ajmc.com/newsroom/vice-president-biden-delivers-cancer-moonshot-report-to-the-nation. Published October 17, 2016. Accessed January 18, 2017.
MYSTIC Trial, Evaluating Durvalumab as First-Line Treatment in NSCLC, Adds OS Endpoint
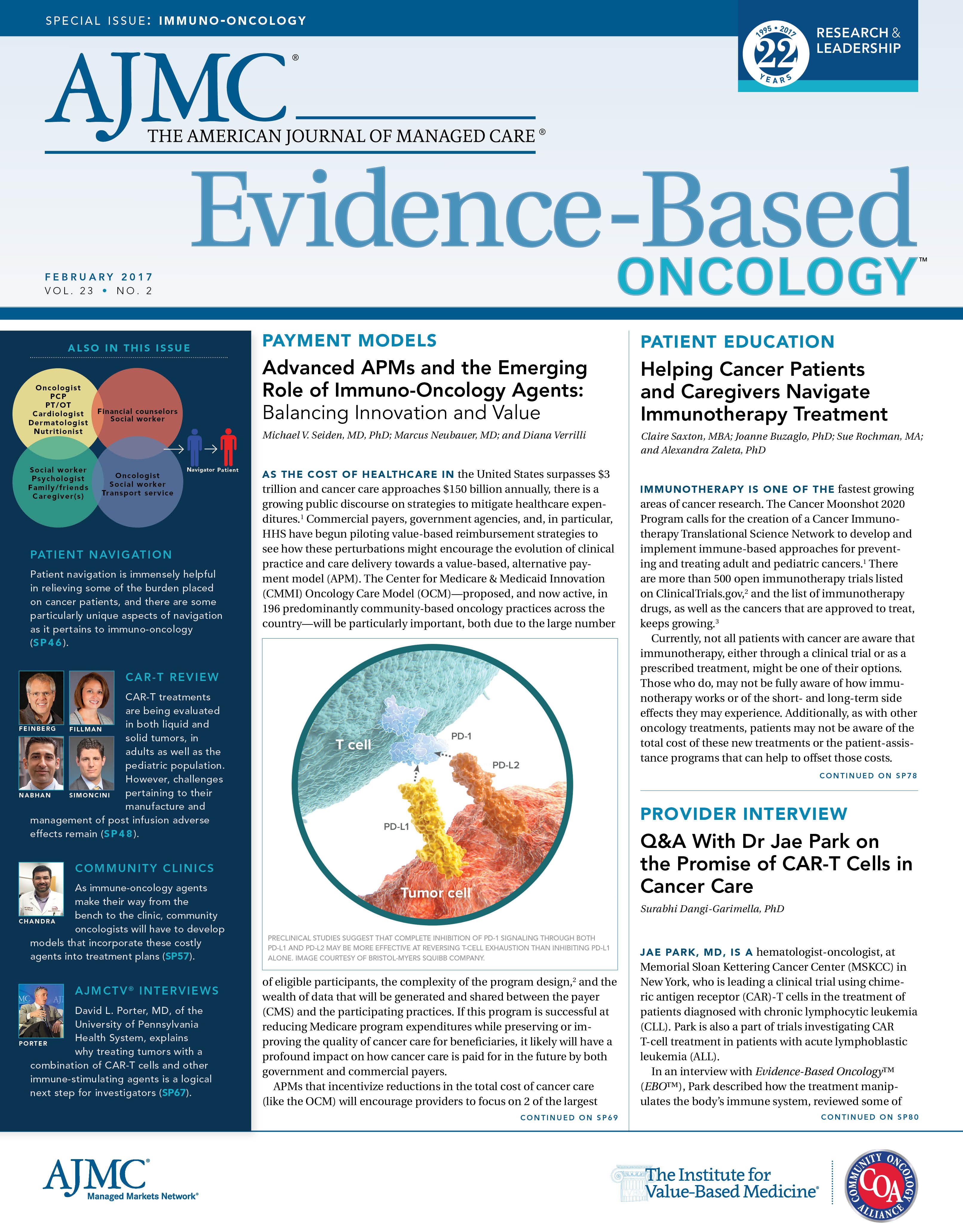
A phase 3 trial evaluating the effect of durvalumab, the programmed death ligand-1 (PD-L1) inhibitor, alone or in combination with tremelimumab, versus platinum-based chemotherapy has refined its endpoints to include overall survival (OS) and progression-free survival (PFS).
The randomized, multi-center, open-label MYSTIC trial was designed to test whether durvalumab can be used as front-line treatment in patients with locally advanced or metastatic non—small cell lung cancer (NSCLC) who express wild-type epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK), and PD-L1. The original primary outcome measure was PFS at 3 years, while secondary outcome measures included health-related quality of life, pharmacokinetics of the drugs, and immunogenicity of the biologicals durvalumab and tremelimumab.
In a press release, AstraZeneca, which is developing the drug, said that the decision to include OS as an endpoint “is based on recent internal and external data, including durvalumab’s strong efficacy as monotherapy presented at recent medical meetings, as well as significant opportunities in the competitive landscape.” This update will extend OS data collection to 2018, while PFS data and several interim analyses for OS are expected in mid-2017.
The company is simultaneously testing durvalumab as monotherapy (PEARL trial) or in combination with tremelimumab (NEPTUNE trial) against standard-of-care platinum-based chemotherapy in patients with EGFR and ALK wild-type advanced or metastatic NSCLC. “The MYSTIC trial amendments, the NEPTUNE trial expansion, and initiation of the new PEARL trial are all designed to enhance our options in first-line NSCLC for immuno-oncology (IO—as monotherapy or combination with another IO agent. We continue to follow the science through both internal and external sources for the benefit of patients and look forward to sharing our first pivotal data in mid-2017,” Sean Bohen, MD, PhD, executive vice president, Global Medicines Development, and chief medical officer at AstraZeneca, said in the press release.
Durvalumab is a PD-L1 inhibitor that received a breakthrough designation for use in bladder cancer in early 2016. By interacting with both, the programmed death-1 receptor and CD80 on T cells, it boosts the immune system’s tumor-detecting capacity. AstraZeneca is also evaluating this antibody in head and neck cancer, liver cancer, and blood cancer.
Reference
AstraZeneca expands 1st-line lung cancer immuno-oncology programme opportunities [press release]. London, UK: AstraZeneca; January 17, 2017. https://www.astrazeneca.com/media-centre/press-releases/2017/astrazeneca-expands-1st-line-lung-cancer-immuno-oncology-programme-opportunities-17012017.html. Accessed January 17, 2017.
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
Empowering Children and Parents Through Technology: Opportunities, Challenges, and Future Directions
January 15th 2026Digital health platforms improve pediatric care by offering customized, interactive tools for children and parents. They enhance education, support, and engagement while tackling challenges related to access, usability, and privacy.
Read More
Insights Into Patient Portal Engagement Leveraging Observational Electronic Health Data
January 12th 2026This analysis of more than 250,000 adults at least 50 years old with chronic conditions showed lower portal use among older, non–English-speaking, and Black patients, underscoring digital health equity gaps.
Read More
Subjective and Objective Impacts of Ambulatory AI Scribes
January 8th 2026Although the vast majority of physicians using an artificial intelligence (AI) scribe perceived a reduction in documentation time, those with the most actual time savings had higher relative baseline levels of documentation time.
Read More
Telehealth Intervention by Pharmacists Collaboratively Enhances Hypertension Management and Outcomes
January 7th 2026Patient interaction and enhanced support with clinical pharmacists significantly improved pass rates for a measure of controlling blood pressure compared with usual care.
Read More

