- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
AJMCtv® Interviews, February 2017
AJMCtv® interviews let you catch up with experts in healthcare. Topics include challenges with immuno-oncology, including the patient voice in treatment decisions, and why payers should cover genomic testing.
David Fabrizio Suggests Advantages of Genomic Profiling for Payers
Payers have been slow to adopt new technologies, but they are starting to be more proactive in seeking out genomic profiling companies, according to David Fabrizio, of Foundation Medicine, Inc. These molecular diagnostic tools make the healthcare process more efficient by performing a comprehensive test at the point of diagnosis.
What specific challenges does the molecular diagnostics industry face with respect to insurance coverage for their products?
There is a challenge associated with getting coverage for molecular diagnostics. For the most part, payers have been slow to adopt new technologies and really, they haven’t been incentivized to do so, up until recently. However, what we’re starting to see is that payers are being more proactive, certainly, in seeking out companies like Foundation Medicine that are building these comprehensive genomic profiling assays to understand what’s going on inside a patient’s tumor at the molecular level, and these are encouraging signs.
I think that they’re starting to understand the implication of using these molecular diagnostics up front at the very point of diagnosis, because it can remove a lot of the ambiguity associated with following that trail of breadcrumbs about understanding what is really contributing to a patient’s disease, and what is the best course of therapy. So rather than doing 1 test and getting 1 answer and then trying a treatment that doesn’t work and then trying another test, you do a comprehensive test like a FoundationOne test, for instance, up front, and it makes the healthcare process more efficient, and that’s a benefit to patients and payers.
Dr David L. Porter: Combining CAR-T Cells With Other Immunotherapies, the Next Logical Step
David L. Porter, MD, of the University of Pennsylvania Health System, explains why treating tumors with a combination of CAR-T cells and other immune-stimulating agents is a logical next step for investigators.
Can CAR-T cells be combined with other immunotherapies or targeted agents?
There is no doubt that CAR-T cells will ultimately be combined with other immunotherapies and other agents. There are years and years of precedent for combining different types of anticancer therapy. I do think there will be some cases where CAR-T cells are sufficient by themselves. We’ve seen that already in some of these B-cell malignancies and ALL [acute lymphoblastic leukemia] and some people with non-Hodgkin’s lymphoma or CLL [chronic lymphocytic leukemia].
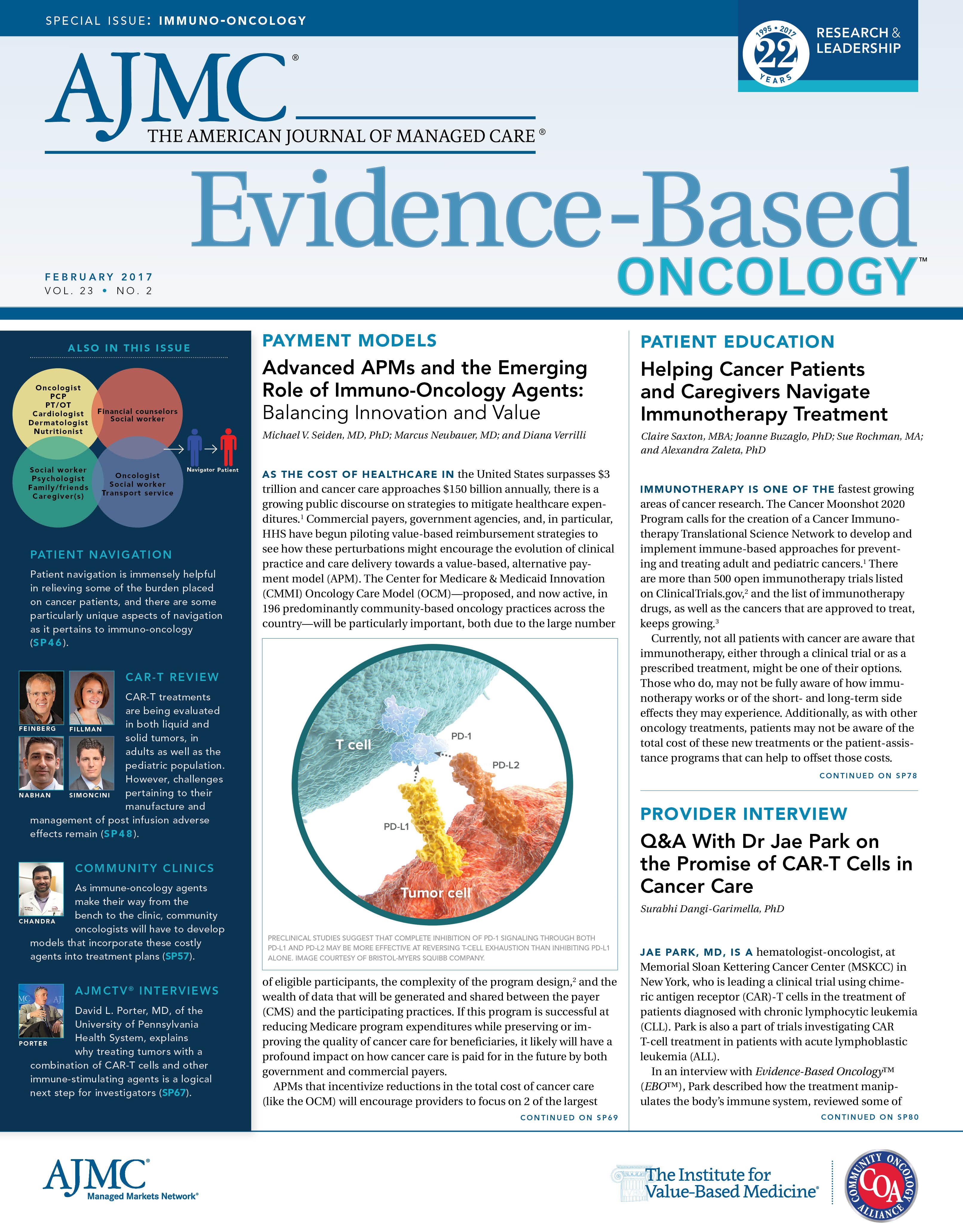
But, there will be situations where the CAR-T cells may not be effective by themselves, and there are some natural combinations one can start thinking of. For this to be effective, the T cell has to be active, so combining the CAR-T cells with immune-stimulating agents will be very, very logical: some of the checkpoint inhibitors, for instance.
There are also clinical trials currently ongoing, combining CAR-T cells with medications like ibrutinib. Ibrutinib’s a very common therapy for CLL and some B-cell malignancies, and there is now good laboratory data [showing] that ibrutinib may make the CAR-T cells more effective at killing their target, at killing CLL cells for instance. And there’s data in the laboratory that it may make the CLL cells better targets for the T cells to kill them. It’s another natural combination that, I think, investigators are thinking of testing.
And there are a number of other agents that one can think of to try and activate the T cells when perhaps the body’s natural defenses are designed to keep the T cells from becoming activated, or the cancer’s defenses are designed to keep the T cells from getting into the tumor or from being activated. So, I think, there are a lot of possibilities, and we will see these trials being done over the next few years, combining CAR-T cells with other agents, as well.
Debra Madden on Unrealistic Expectations for Immuno-Oncology Treatments
Many patients have learned about the advances in immunotherapy treatments for cancer, but the media may not fully portray all the complexities and potential harms of these agents, according to Debra L. Madden, cancer research advocate and patient representative. Madden mentioned that biomarker research could help determine which patients are most likely to benefit from immuno-oncology.
What is the current level of knowledge most cancer patients have regarding immunotherapy risks?
If they’re interested in information about cancer treatments, they will have noticed that there’s all sorts of announcements about immunotherapy overall, and what an important advance it is, and how it’s the most exciting breakthrough that we have seen in cancer treatment in decades. And for some patients, that’s true.
But, again, I worry sometimes about how important and complex medical topics are presented in the popular media, because there’s not always discussion about some of the adverse effects, and some of the potential harms, as well as the potential benefits. However, a couple areas aren’t mentioned as much in the popular media. And that’s the fact that, yes, there are some patients who have done extremely well with traditionally very difficult-to-treat cancers and advanced cancers. However, unfortunately, that’s the minority of patients. Most patients do not have a response to these immuno-oncologic agents. One of the most important research questions that we have, at this point, is determining what biomarkers can we look at that will indicate who are these patients who are most likely to respond, so we can have more patients ultimately benefit.
Dr Carrie Stricker Discusses the Importance of the Patient Voice in Oncology Treatment Decisions
Oncologists must recognize the importance of the patient voice when making treatment decisions so that the treatment plan can be adapted to each patient’s goals and desires, said Carrie Stricker, PhD, RN, AOCN, chief clinical officer and co-founder of Carevive Systems.
What is the importance of including patient voices when providing decision support to clinicians?
The attention to the patient voice at time of treatment decision making, in clinical decision making, is thankfully increasing by leaps and bounds. I’ll highlight for a moment—I am a volunteer for the American Society of Clinical Oncology (ASCO)—I’ll highlight for a moment ASCO’s value framework as one of the proliferating models for helping to ensure that clinicians can make evidence-based and very person-centered decisions at the point of care. And one of the 3 major factors that are included in that value framework is the patient’s voice and the patient’s preferences.
If we don’t ask a patient what their goals are, what’s valuable to them, and reflect that into our decision making, we could have a patient who really wants to have as their primary goal adequate quality of life and survival to make a significant wedding or other family event without their hair, or with enough functional status intact to be present physically and emotionally for that event, we could end up giving them a highly toxic regimen that they would not want had they known that that would be the outcome for them.
So, it’s absolutely crucial, and studies have shown, again and again, that we must get also at the patient’s understanding of what the goals of that treatment is for them. Some studies have shown that more than half of patients may think treatment is curative when, in fact, it’s intended to control, perhaps for long periods of time, but control and not cure disease. And we know from many case examples, analyses, and studies that patients say they would have made very different decisions had they known that information and had an opportunity to have an active voice in that treatment decision making and have it adapted to their preferences and goals and concerns.
Jonathan Hirsch on Making Data Usable for Oncologists at the Point of Care
Oncology care is often spread out across multiple facilities and providers, so health information technology (IT) innovators use software to integrate data from these many locations and deliver it to the point of care, according to Jonathan Hirsch, founder and president of Syapse.
How can health IT be used to transform oncology care?
Oncology is an incredibly complex domain, and it involves many different providers who may be at different practices, different health systems. It involves not just the medical professionals, but it also involves supportive care, like care coordinators, navigators, et cetera. And with oncology, you have this interesting dynamic where the care is highly longitudinal, it’s spread out across multiple facilities, and having access to the right information at the right point in time is truly the way to make progress in the fight against cancer.
So that’s really the job of software. It’s to bring all the information together and make it usable for the provider of oncology care to help that patient. When we think about how we use software to appropriately direct care and help in the fight against cancer, it’s really bringing the right information to the right person at the right point in time, but also having robust outcomes tracking capability so that the providers are not operating in isolation. You want to help the providers learn from the experiences of every other cancer case and every other provider facility.
One of the things that we’ve done to achieve this vision is we’ve partnered with a number of leading health systems, Intermountain, Stanford, and Providence Health & Services, to launch the Oncology Precision Network. This is an effort to use software and large data sets to really fight cancer by bringing the aggregate data and learnings from that network to the point of care, and this wouldn’t be possible without a robust software platform.
Dr Sean Khozin Discusses How FDA Regulatory Process Helps Advance Precision Oncology
FDA’s regulatory science activities are working to advance the field of precision oncology, in part by using predictive analyses to identify patients that may be good candidates for certain therapies, according to Sean Khozin, MD, MPH, senior medical officer at the FDA.
How does the FDA encourage advances in precision oncology?
If we look at the definition of precision oncology, as we all know, we can best describe it as delivering the right drug to the right patient at the right dose. If you look at FDA’s approval mechanism, you’ll notice that the policies and procedures that have been put into place, in fact, are based on that very precise definition of precision medicine.
So, in essence, when we review a marketing application, when we analyze the data, and do labeling negotiations, we ensure that the data support the indication, the population of patients who are supposed to be treated, at the right dose. So, that system has already been built into the approval process and the mechanism at the FDA.
Now, precision is a moving target and it’s driven by science. And it’s a very rapidly evolving field in oncology. Obviously, drugs are getting more targeted and more precise. So one of the ways, and one of the primary ways, that the FDA has been contributing to the advancement of the field is through its regulatory science activity. What we have been doing more, especially more in recent years, is looking at our own internal data and doing our own analyses, aggregated analyses on primary research to be able to identify, for example, populations of patients who may have certain characteristics that may make them a good candidate for certain types of therapies. We’re doing predictive analytics.
So, that’s become part of the regulatory science process where we are doing primary research using our own data, and also in collaboration with outside entities to contribute in a very proactive fashion to the advancement of the field of precision oncology.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More

