- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Impact of the COVID-19 Pandemic on Specialty Community Practices: An Oncology Perspective
The COVID-19 pandemic has impacted specialty practices generally and oncology practices especially have been resilient throughout the pandemic.
ABSTRACT
Objectives: Typically, a community-based specialty practice is prepared for a limited public health crisis that is driven by a natural disaster or a localized environment event. This article describes the unexpected impact that the coronavirus disease 2019 (COVID-19) pandemic has had on community-based specialty practices across the United States, especially oncology practices.
Study Design and Methods: We conducted an electronic national survey of community-based specialty practice administrators to determine the impact of COVID-19 on their practices and their ability to manage through a global pandemic. The 22-question survey focused on an initial observation period of March 15, 2020, to May 15, 2020, compared with a second period of May 16, 2020, to August 15, 2020.
Results: Oncology practices accounted for 46% of the 155 specialty practices that participated in the survey. Overall, 57% of respondents saw at least a 30% decline in total patient volume and/or financial impact during the initial observation period, compared with a 38% decline for the oncology practices. More than 70% of all practices experienced improvement after May 15, 2020, with at least 60% improving regardless of specialty. The initial decline was primarily driven by declines in new patient volume and procedures. Approximately 62% of practices anticipate a moderate-to-significant impact on patient outcomes over the next 12 months. The impact expected was slightly higher in retina and ophthalmology practices than oncology.
Conclusions: Although unexpectedly impacted in delivering care for their patients, specialty practices generally and oncology practices especially have been resilient by leveraging federal funds and adopting operational enhancements.
https://doi.org/10.37765/ajmc.2020.88569
INTRODUCTION
It is estimated that the coronavirus disease 2019 (COVID-19) pandemic generated at least $202.6 billion in losses for health care systems and hospitals during the first 4 months of the public health crisis.1 From the start of the pandemic to the end of April, there was a nearly 60% decline in ambulatory care.2 It is anticipated that the reduction in health care utilization will more than cover the incremental costs of testing for and treating COVID-19.3 However, such reductions in utilization, chiefly in preventive care in oncology, may have ripple effects, leading to delayed diagnosis, stage migration, and the potential for increased morbidity and mortality.4 This impact can vary by geography as well as differ based on the type of care. It was identified that breast cancer screenings had declined by as much as 86% by the end of April, followed by increased volume since then.3 An initial report in oncology demonstrated a nearly 40% drop in new patient visits for community oncology practices.5
However, it is not clearly understood how community-based care has been impacted across the various specialties—especially oncology. The implication for patient outcomes will need to be evaluated for the foreseeable future. To assist in putting the impact into perspective, we will share the results of a national survey to understand the impact and recovery of the initial wave of COVID-19 on specialty practices.
STUDY DESIGN AND METHODS
We conducted an electronic survey of specialty practices across the United States. These practices encompassed the following specialties: oncology; retina and ophthalmology (referred to as vision practices); rheumatology, gastroenterology, urology, and neurology (referred to as other large specialty practices); and other clinics such as orthopedics and acute care. The survey consisted of up to 22 questions that compared the impact of COVID-19 on key performance measures, the adoption of operational enhancements, and federal stimulus between the initial observation period of March 15, 2020, to May 15, 2020, and the next 90-day period of May 16, 2020, to August 15, 2020. The survey was conducted at the end of the second period over a 15-day period.
The survey was distributed to practice administrators of 1500 specialty practices geographically dispersed. This anonymous survey was conducted through the QuestionPro survey service and analyzed using descriptive statistics. Survey responses were compared with both electronic medical record and practice billing information to address any potential response biases.
RESULTS
A total of 155 specialty practices participated in the survey. Of these, 46% were oncology community practices. Vision and other large specialty practices represented 21% each. Approximately 74% of practices had 1 to 6 physicians. The majority were in suburban locations, with varied geographic distribution among the specialties. These differences are illustrated in Table 1.
TABLE 1. Practice Attributes of National Survey Respondents
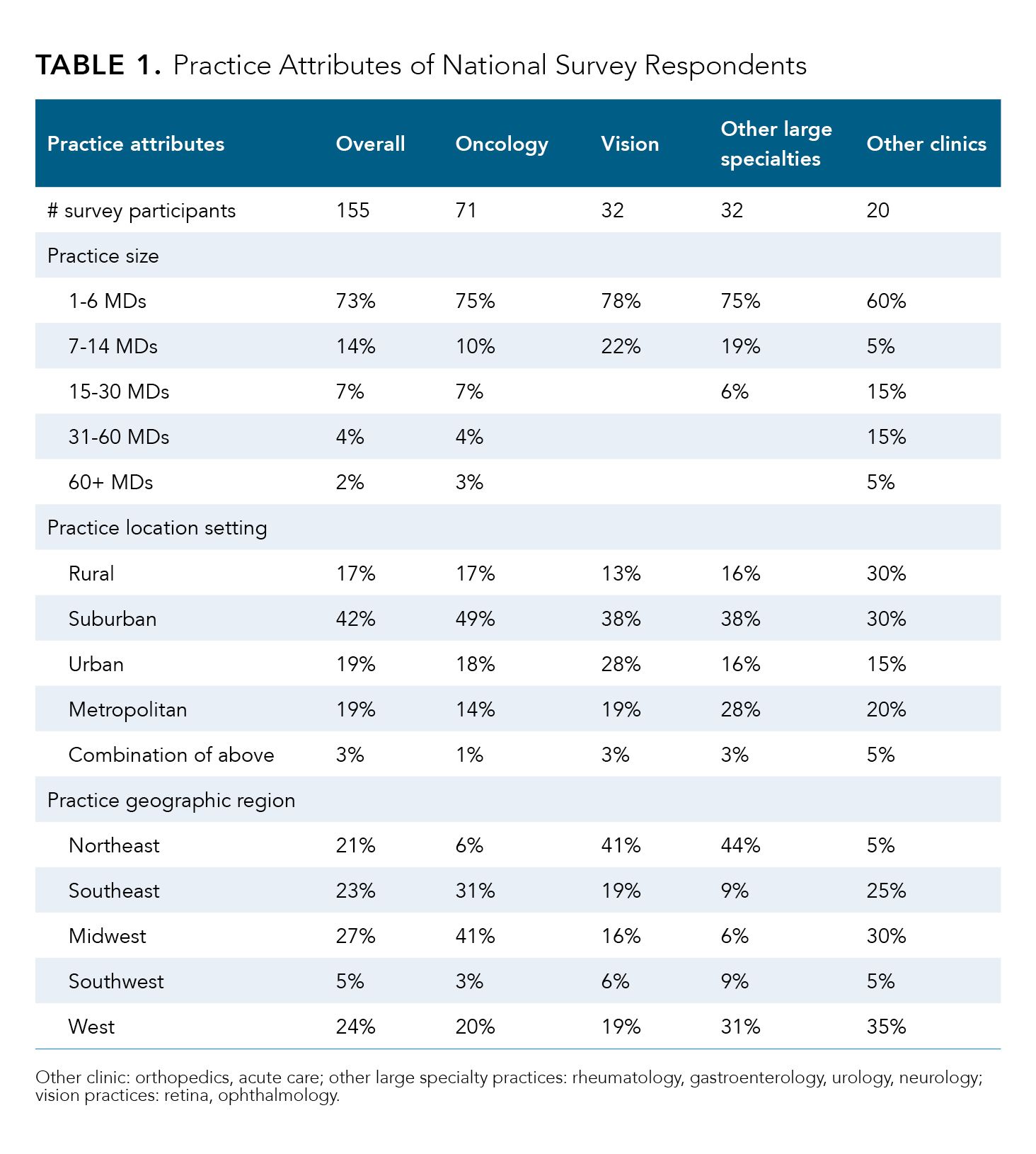
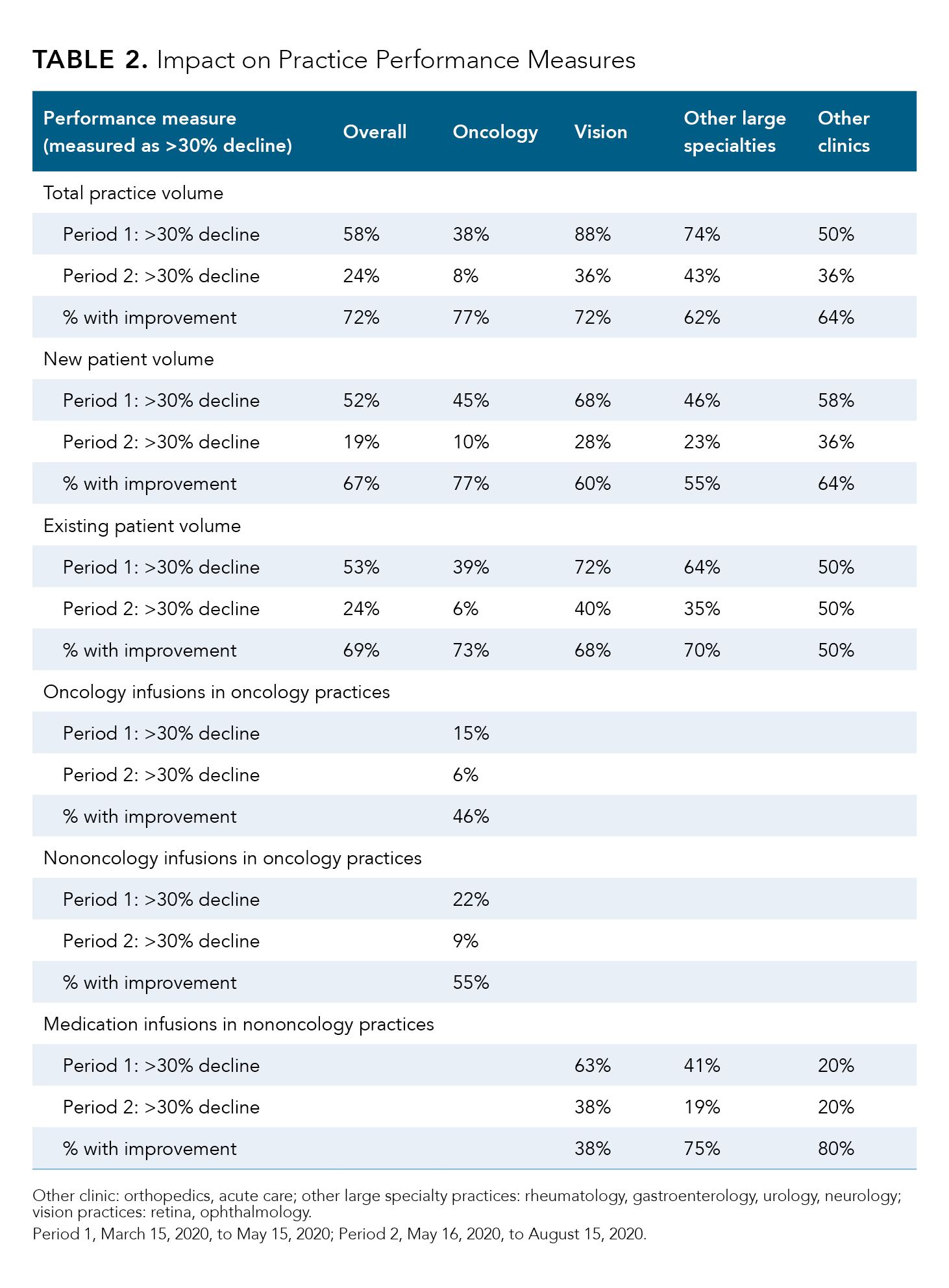
Overall, more than 50% of specialty practices experienced at least a 30% decline in total patient volume within the initial 60-day period, while approximately 38% of oncology practices saw similar declines as displayed in Table 2. More than 70% of practices have seen improvements in patient volume since the middle of May. One of the primary drivers in the initial decline between March 15 and May 15 was the decline in new patient visits; more than 50% of practices had a decline of greater than 30%. Similar declines were seen in 43% of oncology practices. Oncology practices observed the greatest level of rebound with 77% having improvements in the second observation period. Although the other specialty segments saw patient volumes increase, the majority were starting from a more significant deficit. The declines of more than 30% in existing patient encounters were seen in 39% and 72% of oncology and vision practices, respectively. In the second observation period, approximately 69% of practices had experienced some level of improvement, with at least 45% of oncology practices returning to normal patient volumes within the second period.
The majority of oncology practices had less than a 30% decline in oncology drug infusions (79%) and nononcology drug infusions (67%) during the initial period. Increases in drug infusions were experienced in at least 46% of oncology practices during the second period. Approximately 57% of other specialty practices had less than 30% declines in medication infusions during the initial period with improvements observed in 66% of these practices. Increases in medical and diagnostic procedure volume was observed in 68% and 73% of vision and other large specialty practices, respectively. Less than 20% of practices with in-office dispensing capabilities saw significant declines of more than 30%. Of those, 50% of the other large specialty practices continued to be impacted compared with 3% of oncology practices.
Only 42 participating practices conducted clinical trials. Of these, a reduction of more than 30% of new patient enrollment occurred in 26% of practices, and 12% of practices saw a similar reduction in scheduled patient trial encounters. Oncology practices were the least impacted from new patient enrollment. Trial enrollment had still only improved for 35% through mid-August.
TABLE 2. Impact on Practice Performance Measures
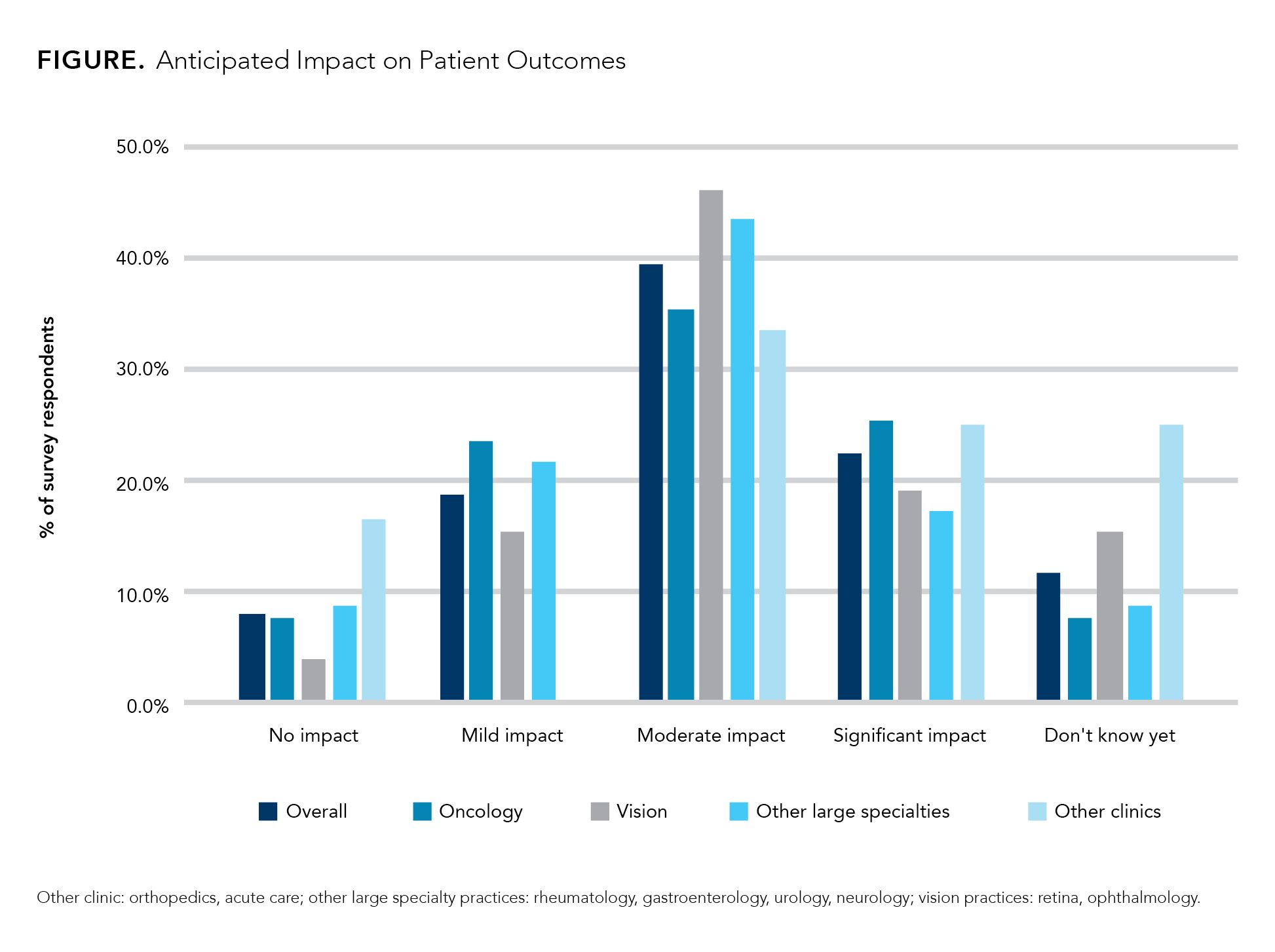
Delays in diagnosis and treatment can have substantial impact on patient outcomes. Based on the participating practices, approximately 62% of respondents feel there will be a moderate-to-significant impact on patient outcomes over the next 12 months. This was consistent across all specialty segments as demonstrated in the Figure.
FIGURE. Anticipated Impact on Patient Outcomes
The adoption of telemedicine for care delivery was a significant advancement. Approximately 72% of practices implemented telehealth services within the first 30 days of the pandemic. However, more than 60% of vision practices did not use these services due to their inability to conduct the appropriate patient assessments through this technology. Other than in vision practices, telemedicine was primarily used for follow-up visits due to similar challenges. Seventy-eight percent of practices were using secure, Health Insurance Portability and Accountability Act-compliant telemedicine platforms.
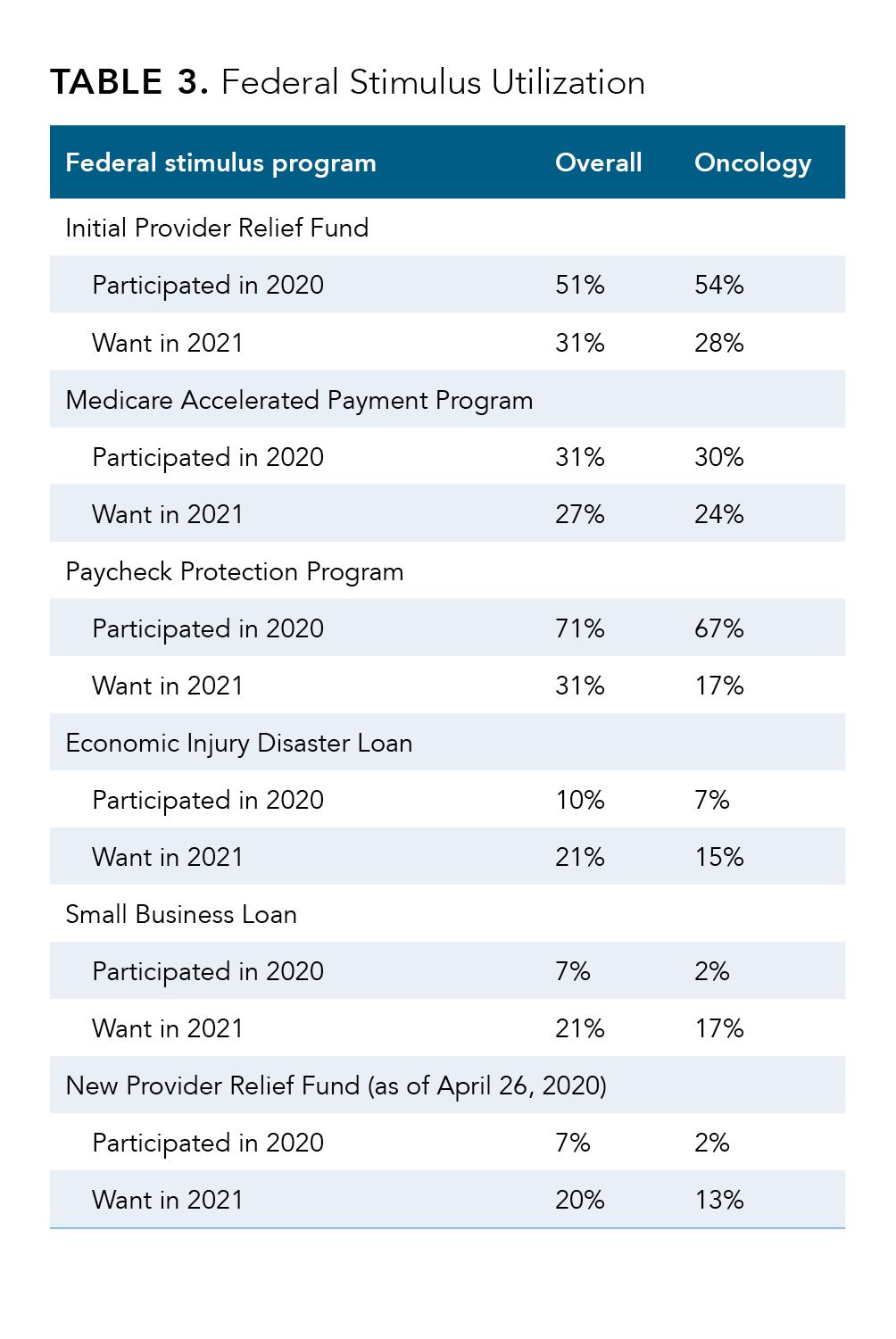
At least 70% of responding practices (Table 3) were able to use federal stimulus relief; the most common was the Paycheck Protection Program. This included 67% of oncology practices. The initial Provider Relief Fund program, the next most frequently used program, was used by 51% of all practices and 54% of oncology practices. Approximately 59% of oncology practices are still not sure that the federal stimulus programs will be enough to cover unexpected operational expenses for another 6 to 9 months. Only 28% of all practices felt it would be sufficient to cover these expenses through the next wave of the pandemic.
TABLE 3. Federal Stimulus Utilization
More than 80% of each specialty practice segment has adopted necessary COVID-19 testing and return-to-work protocols. However, 30% felt that their practices were not prepared to address the Families First Coronavirus Response Act requirements.
Overall, the highest ranked activity practice desired to have in place in 2021 was the forgiveness of all Paycheck Protection Program payments. However, oncology and other large specialty practices felt that telehealth at reasonable reimbursement was the most important, followed closely by Part B drug sequestration relief for oncology practices.
DISCUSSION
Based on the results of this national survey, we have seen how resilient our community-based specialty practices are. Although all were challenged with the initial onslaught of the COVID-19 constraints, they collectively identified ways to modify their operational approaches. The government took steps to allow for broader use of telemedicine, which most specialty practices adopted within the first 30 days of the pandemic. However, not all specialties were able to leverage telemedicine to the same level of operations due to the complexity of new patient assessments and some types of follow-up visits, especially in patients with retinal disorders and cancer. It is estimated that one-third of older adults are still not ready to use telemedicine,6 which has continued implications for oncology and vision-based specialties.
New patient visits, both from a conduct and referral perspective, have had significant impact on specialty practices. Some reports have published declines of up to 47% in patient visits for oncology practices by the beginning of April, with 20% improvement by early May.2 Recently analyzed information of 104 oncology practices who utilize InfoDive showed that oncology practices had seen an average decline of 30% in new patients by end of April and have rebounded back to 6% below the rates in February. New patient visits declined by 44.6% and 68.0% in April for urology and vision practices, respectively, compared with February. And, those practices have come back to within 6.3% and 12.3% of their pre–COVID-19 new patient volumes.7
This situation translated into an average decline in reimbursement of 17.1%, with the most significantly impacted practices being those that conduct surgical and medical procedures, including orthopedic, urology, and vision practices. Approximately 35% of oncology practices observed declines in reimbursement within the first period, while 37% were still dealing with declines in August compared with pre–COVID-19 reimbursement rates. These declines can be attributed to the delays in cancer screening and diagnostic procedures that result in new patient referrals. Weekly visits to oncologists are approximately 2% below prepandemic levels, compared with improvements of 4% for ophthalmology and urology.8
CONCLUSIONS
The impact on specialty practices is widely varied based on the type of services provided. Those specialties that are primarily delivering medical care along with drug administrations were less impacted initially; however, they continue to be challenged with the delays in newly diagnosed patients. Those practices whose services are primarily associated with surgical or medical procedures were able to rebound quickly once state and local restrictions were removed. Although at least 70% of surveyed practices reported utilization of federal stimulus packages, only about 30% felt some form of these options should be available in 2021. Some considerations should be made for these variations in service delivery. Importantly, the majority of community-oncology based practices maintained the best possible access to patient care, implementing and using telehealth services more frequently than institutional health systems did. However, hospital systems were extremely involved in the actual care of acutely ill patients with COVID-19. Regardless, the majority of community practices were able to remain open and to provide some level of service, unlike those within the hospital and health system settings.4 Continued focus of key activities should be strongly considered to strengthen oncology practices throughout the pandemic, including but not limited to elimination of sequester to part B drugs; securing telehealth reimbursement at reasonable levels; continued government financial assistance with personal protective equipment costs; and reducing barriers to screening procedures for prevention of cancer by payers, such as elimination of co-pays or suspension of prior authorization processes that delay care.
Author Information
Lucio N. Gordan, MD, is the president and managing physician of Florida Cancer Specialists and Research Institute. Contact: lgordan@flcancer.com
Susan Weidner, MS, is the senior vice president, analytics, for IntrinsiQ Specialty Solutions, Inc.
References
1. Hospitals and health systems face unprecedented financial pressures due to COVID-19. American Hospital Association. May 2020. Accessed November 1, 2020. https://www.aha.org/guidesreports/2020-05-05-hospitals-and-health-systems-face-unprecedented-financial-pressures-due
2. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges. To the Point (blog). Commonwealth Fund. May 19, 2020. Accessed November 1, 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits
3. White paper: the up and down impact of the pandemic on health care costs. Willis Towers Watson. September 29, 2020. Accessed November 1, 2020. https://www.willistowerswatson.com/en-US/Insights/2020/09/the-up-and-down-impact-of-the-pandemic-on-health-care-costs
4. Patt D, Gordan L, Diaz M, et al. The impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. Published online October 21, 2020. doi:10.1200/CCI.20.00134
5. Ong MBH. Real-world evidence: COVID-19 vs. community oncology: Flatiron’s data provides first damage assessment. The Cancer Letter. May 1, 2020. Accessed November 1, 2020. https://cancerletter.com/articles/20200501_1/
6. Admin_NH. Telemedicine for seniors: helping patients get the most out of their visits. swyMed™ Newsletter. October 23, 2020. Accessed November 1, 2020. http://swymed.com/telemedicine-for-seniors-getmost-visits/
7. InfoDive COVID impact analysis. IntrinsiQ Specialty Solutions. October 13, 2020. Accessed November 1, 2020.
8. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. To the Point (blog). Commonwealth Fund. October 15, 2020. Accessed November 1, 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits