- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
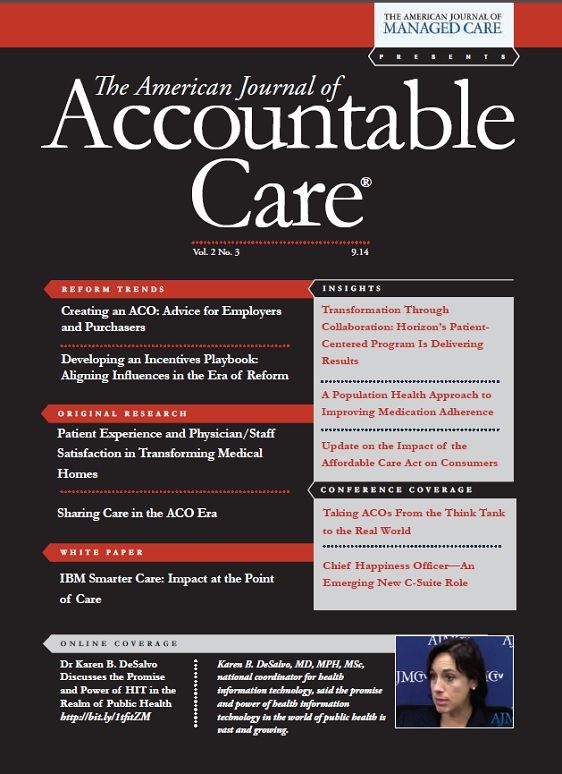
IBM Smarter Care: Impact at the Point of Care
IBM Smarter Care uncovers valuable insights into lifestyle choices, social determinants, and clinical factors enabling holistic and individualized care to optimize outcomes and lower costs.
Better Care at Lower Cost
In Europe, the rise in chronic disease in an aging population is consuming an ever-increasing share of healthcare resources. To stem the tide, one healthcare provider in southern Europe is piloting a new program for complex chronic disease management to support elderly patients with multiple chronic illnesses. The system will help nurses, primary care physicians, specialists, and social workers coordinate their efforts to provide holistic and individualized in-home support to individuals. The system’s objective is to improve adherence to care programs, quality of life, and satisfaction with the healthcare system, all while reducing costs.
Key to the program is creating a customized care plan for each individual. A 360-degree view of the clinical and functional information collected from the primary care physician, acute care practitioners, labs, and other departments informs the plan. This information was previously segregated in more than 20 different databases and many custom and commercial applications.
Introduction
Healthcare is in crisis. Globally, aging populations combined with a steady rise in the incidence of chronic diseases have led to healthcare spending that consumes an ever-increasing portion of the world economy.1 Solutions have been researched and debated for decades, and many health organizations are in the midst of transforming into more coordinated, efficient, and purposeful care delivery systems. But the healthcare industry cannot solve the world’s health problems alone.
Healthcare is not the only factor that plays a role in a person’s health status.2,3 Genetics, health-related behaviors, and social and environmental factors also contribute to the health of individuals and entire populations.3 Combating the escalating crisis in healthcare spending and making substantial improvements in the health and vitality of people around the world both require much broader coordinated efforts by many systems and stakeholders.
Smarter Care
Health and social care systems are interdependent; each critically affects the other. Yet, a complex matrix of public and private stakeholders dedicated to the health and well-being of individuals still operates largely within silos. They provide separate types of intervention, often with competing objectives and insufficient regard for the outcomes.
As the world grows more instrumented and interconnected, the volume and velocity of data available increases dramatically. As a result, new opportunities arise for observing, analyzing, and coordinating the connection between social determinants, clinical factors, and lifestyle choices. The ability to transcend these traditional boundaries and work toward the common goal of holistic and individual care is what we call Smarter Care.
Collaborative innovation is happening in pockets around the globe. We believe the world is now on the cusp of creating a “system of systems,” in which private and public stakeholders are coming together to coordinate resources at unprecedented levels. These stakeholders span industries, providers of social and community services, and governments large and small.
Smarter Care in Action: 3 Examples
1. The Camden New Jersey Coalition of Healthcare Providers uses big data to pinpoint “hot spots,” or places with a high density of people with complex medical, social, and behavioral needs. The coalition analyzed medical records from 3 major hospitals in Camden from 2002 to 2011. It found that just 1% of the city's patients generated 30% of emergency department expenses, and 90% of emergency department costs were generated by 20% of patients. By providing and coordinating the medical care and social services of the highest-need patients, the coalition has been able, in some cases, to reduce the cost of their care by almost half.4
2. Another hot spot that exemplifies the collaboration that is possible in a receptive community is on the west side of Saskatoon, Saskatchewan, Canada. It has the highest rate of new HIV cases in Canada; higher than average rates of diabetes, depression, addiction, sexually transmitted diseases, and hepatitis C; and an exceptionally high rate of infant mortality. So to meet the needs of the community, launched Station 20 West, a $20-million project that combines affordable housing; a library; medical offices, including a clinic run by medical students that welcomes patients after hours and on Saturdays; and a grocery store with an intentional focus on healthy food.5
3. The Castlefields Health Centre in Cheshire county, England, is taking an integrated approach to health and social care for the elderly. A district nurse works with a social worker to identify and provide supportive care in a program that, has reduced hospital admissions of patients 65 years and older by 14%. This program has also significantly lowered the average length of stay for those elderly patients who cannot avoid hospitalization.6
Data-Driven Insights
Data today can be acquired from novel and diverse sources, which helps pinpoint opportunities in a population to transform care for the individuals with the greatest needs. Being able to capture, manage, and use all forms of data from all relevant sources are what enable new types of personalized insights and care that can make a significant difference.
Health and social care leaders are working to improve wellness in their communities and to operate with greater financial efficiency. Health insurer WellPoint has pioneered the use of cognitive computing systems to encourage use of evidence-based practices in its provider network. Memorial Sloan Kettering Cancer Center and IBM are co-developing cognitive capabilities so that oncologists everywhere will be able to make better informed treatment decisions with their patients. Developmental Services Ontario, a network of agencies that helps adults with developmental disabilities, relies on more sustainable, community-based support and individualized care plans to improve the health and well-being of individuals.
These organizations and other innovators are focusing on entire populations as well as on the individual, to understand each person’s context. They are using new and existing data sources and analytic innovations to uncover valuable insights into lifestyle choices, social determinants, and clinical factors. With these insights, they are able to create a more holistic view of individuals and their unique requirements; they can also provide more coordinated, efficient care and advanced care management with a deeper level of engagement that can improve outcomes and lower costs.
Creating Communities of Care
Health and social care systems are being recast through new business and financial models with new partnerships and relationships. For example, governments are focusing on achieving better outcomes and lowering costs in both social programs and healthcare. Employers are offering incentives, education, and health benefits programs to help employees make healthier lifestyle choices and improve their overall wellness.
• Intervention. Identifying and influencing populations and recognizing intervention opportunities.
• Knowledge. Driving evidence-based and standardized care planning.
• Collaboration. Assessing and engaging individuals and stakeholders for the creation of individualized care plans.
• Coordination. Delivering care and monitoring progress based on clinical and social requirements.
• Learning. Applying new insights from interactions and outcomes to enable continuous transformation.
Such efforts must be aligned to create stronger communities of care that share common priorities. Based on experience with a vast number of client engagements in care industries, IBM has identified a common set of drivers of quality care that enable more successful outcomes for individuals and stakeholders worldwide. They include:
No matter where care originates, communities of care must be able to identify the interdependencies between health and outcomes, and between surrounding social care systems and community support structures. And, they must exploit all care-related data to uncover clinical and social insights that can be woven into all aspects of care, even when the data is from multiple disconnected sources.
The Continuum of Care
With context-based insights from social and clinical analysis, care professionals can segment populations by risk profiles (Figure), inform care approaches for individuals, and proactively manage finite care resources faster and more efficiently. The result is improved outcomes. Identifying specific risk factors for individuals can guide better decision-making at every stage along the continuum of care. Such insights allow for:
• Preventive measures, such as vaccination programs or wellness promotions, and early intervention initiatives.
• Routine screenings that can predict disease onset.
• Education and incentives that encourage healthy lifestyle choices to help control risks.
Smarter Care can help organizations in care-related industries improve health and wellness outcomes for their constituents, while strengthening their own financial performance. Enabled by new technologies, organizations in systems of care are crossing boundaries to share and advance common goals centered on the individual. Taking a holistic approach makes it possible to deliver efficient, integrated services, and individualized care that can improve outcomes, lower costs, and drive wellness and community vitality.
Smarter Care Enables Organizations to:
• Synthesize knowledge and analyze large, complex care-related data sets to identify those at risk.
• Manage information that spans multiple stakeholders, including wellness, health, and social care organizations.
• Deliver proactive, individualized care that eliminates unnecessary and preventable inpatient hospital admissions and readmissions.
• Highlight the most effective evidence-based care protocols for greater economic value and reduced waste.
• Collaborate over boundaries, including organizational, bureaucratic, and technological, to enable individual and population health.
• Provide coordinated care to individuals as citizens, patients, and consumers.
Keeping PACE
Singapore’s population of 5.5 million is among the fastest aging in the world today. In August 2011, a 3-year demonstration project called the Singapura Programme for All Inclusive Care of Elders (SingaPACE) launched to evaluate the impact of integrated home- and community-based care intervention on older adults. Its goal is to help them avoid hospitalization and improve quality of life. A collaboration of the Tsao Foundation, Singapore General Hospital, and Alexandra Hospital, the program provides comprehensive medical, nursing, health, nutrition, and social programs for the frail elderly in Bukit Merah, including a day healthcare center and home care services. Transportation to and from the day healthcare center is provided.
• Hospital admissions because of accident or emergency
• Admission for acute care
• First admission to residential nursing care
• Patient satisfaction
• Caregiver burden
The 3-year study will measure the following variables for individuals in the program against standard care for elders who are eligible for but decline nursing home placement:
Results from the study will be published on clinicaltrials.gov.7
Conclusion
• Governments
• Social program agencies
• Medical practitioners
• Hospitals and other healthcare providers
• Insurers
• Employers
• Life sciences companies
• Makers of medical devices and diagnostics
• An increasing number of other individuals, groups, and organizations
Improving the way health and social care systems work is not an abstract aspiration but an increasingly urgent imperative. Around the globe, businesses, governments, agencies, and others can work better together to create communities of care. Taking a Smarter Care approach facilitates the implementation of new business and financial models for the global care industry. These models focus on the critical interdependency between:
IBM helps these stakeholders collaborate to uncover valuable insights into social determinants, lifestyle choices, and clinical factors. These insights can be applied to developing a holistic approach to individual and community care.
Why IBM?
Leading, innovative organizations are redefining the value they bring to their markets, partners, and stakeholders, and technology is enabling their transformation. Data-driven insights and comprehensive population analysis are enabling smarter individual care plans that are coordinated between health and social care systems. These technological advances can lead to improved individual outcomes and population health, all of which are critical factors in economic and social progress.
The demographic challenges of the 21st century demand that businesses, governments, cities, and communities articulate a vision, use fact-based decision making, and act with purpose to improve the health and well-being of individuals. For more than 100 years, IBM has been helping healthcare and public sector organizations achieve their goals. IBM has the experience to engage and convene leaders and foster collaboration that crosses all boundaries, all in an effort to meet tomorrow’s challenges through relentless innovation. IBM has deep expertise in managing and integrating complex systems, and IBM specialists have broad subject matter experience in life sciences, bioinformatics, social care, and healthcare. By bringing these together, IBM is enabling a foundation for transforming 21st-century care systems. IBM has completed more than 3000 transformation initiatives, ranging from small hospitals to national healthcare projects, and holds more than 500 patents in analytics and more than 600 in healthcare. IBM has worked with social program agencies in 70 countries and has solutions for social program management and health and social care coordination that were designed by health and social care professionals. IBM supports collaboration between the clinical and social worlds. And, IBM Watson cognitive computing capabilities, hypothesis generation, and evidence-based learning can support medical professionals in decision making.
For more information
To learn more about Smarter Care, contact your IBM representative or IBM Business Partner, or go to ibm.com/smarterplanet/us/en/smarter_care/overview/. © Copyright IBM Corporation 20141. Including 33 of the 34 member countries of the Organization for Economic Cooperation and Development. OECD (2012), OECD Health Data: Health expenditure and financing, OECD Health Statistics. Accessed October 30, 2012. http://www.oecd-ilibrary.org/social-issues-migration-health/total-expenditure-on-health_20758480-table1.
2. McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21(2):78-93. University of Wisconsin Population Health Institute, Madison, WI. County Health Rankings website. 2011. http://www.countyhealthrankings.org/our-approach.
3. Franks P, Clancy C, Gold M. Health insurance and mortality. evidence from a national cohort. JAMA. 270(6):737-741.
4. Expanding “hot spotting” to new communities—what we're learning about coordinating health care for high-utilizers. Robert Wood Johnson Foundation, 2012. http://www.rwjf.org/en/research-publications/find-rwjf-research/2012/01/expanding--hot-spotting--to-new-communities.html.
5. Goldman B. Hot spots: Camden, NJ and Saskatoon, SK, White Coat, Black Art website. Updated November 30, 2012. http://www.cbc.ca/whitecoat/episode/2012/11/30/hot-spots-from-camden-nj-to-saskatoon-sk/ and Burke P, Benefits of Station 20 West. Saskatoon Media Group website. Updated April 8, 2013. http://www.saskatoonhomepage.ca/benefits-of-station-20-west/itemid_21.
6. Lyon D, Miller J, Pine K. The Castlefields integrated care model: the evidence summarised. Journal of Integrated Care. 2006;14(1):7-12. http://www.emeraldinsight-.com/journals.htm?articleid=1934229&show=abstract.
7. Evaluation of the Singapura Program of All Inclusive Care for the Elderly (SingaPACE) Demonstration Project, ClinicalTrials.gov Identifier: NCT01568801. http://clinicaltrials.gov/show/NCT01568801.GVW03048-USEN-01.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

