- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
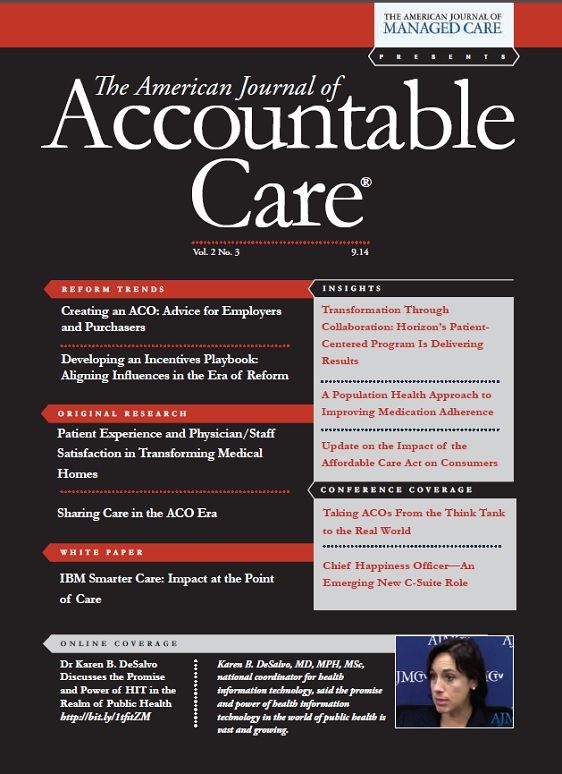
Chief Happiness Officer-An Emerging New C-Suite Role
Treating physicians as your most valued customers: embracing the role of chief happiness officer to drive physician engagement and change management.
I nodded politely in response to each person’s introduction at the dinner table, a lovely setting in one of Bangkok’s trendiest restaurants, while fighting off fatigue from the long flight and anticipated jet lag. Surrounding me was a group of 10 senior executives from the host organization, sponsoring its first-ever geriatrics conference, but honestly, I was mostly thinking about what exactly was in the dish that had just been placed before me. Then the gentleman to my right introduced himself, with a welcoming smile, as Chief Happiness Officer.
Excuse me…who? But here is the logic behind the title:
Expertise in physician engagement and change management is fast topping the desirable-traits list for physician executives involved in population health management. As the industry transforms from a transactional, fee-for-service reimbursement model to a total-cost-of-care, fee-for-value model, the job of the Chief Medical Officer increasingly involves engaging physicians in new care models. Changing a compensation model from purely volume-driven to one that includes quality and efficiency measures is difficult to implement, at best, and physician buy-in is critical for the model’s ultimate success. A key way to succeed in this space is to focus on the thoughtful utilization of selected power tactics.
Informal, or personal, power is widely accepted to be more potent than formal power derived from one’s position or title in an organization. When coupled with rational persuasion (the use of logical arguments and factual evidence, to which physicians are naturally inclined), the informal power tactic of exchange (an explicit or implicit quid-pro-quo) can be very potent. The implicit use of exchange in a population health management setting is essentially focusing on satisfying the wants or needs of the individual whose behavior you wish to influence. Thinking of himself as Chief Happiness Officer, the Chief Medical Officer—in this case, Dr Trin Charumilind, Bangkok Hospital—focuses on improving the work experience for his or her main customer, the physician, relying on the social contagion of happiness to spread to the nurses, receptionists, and other office or hospital staff, which, in turn, translates into positive experiences for patients.
Dr Trin’s introduction certainly brightened my own smile. It became the start of a very productive and informative evening that built the foundation for what I am sure will be a lasting professional relationship. Coupling tried-and-tested rational persuasion arguments with a sincere focus on delivering a tangible benefit to the physician may just be the catalyst for a virtuous cycle of exchange.
So the next time you are struggling with how to influence physician behavior, try envisioning yourself as Chief Happiness Officer!Author Affiliations: Jeffrey Farber, MD, MBA, FACP, vice president, Hospital Services Utilization, Mount Sinai Health System, chief medical officer, Mount Sinai Care, LLC .
Address correspondence to: Dr Jeffrey Farber, One Gustave L. Levy Place, Box 1100, New York, NY 10029. E-mail: Jeffrey.Farber@mountsinai.org
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More

