- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Experts Advise Caution on Reresections for Low-Grade Sarcomas
Investigators explored the utility of unplanned resections, also called reresection, among patients who have soft tissue sarcomas.
Experts have issued caution when considering reresection among individuals who have soft tissue sarcomas (STS), noting that for patients with diagnosed low-grade lesions, a subsequent resection may be unnecessary.1
Also called an unplanned resection, or Whoops procedure—so termed because a removed mass initially thought to be benign is ultimately diagnosed as a sarcoma2—the current team of investigators sought to make inroads against the ongoing debate surrounding reresections: Do they help to reduce local recurrence (LR) and improve overall survival (OS)? The authors highlighted that these types of resections often results in an incidental R1 resection, meaning margins are not clear and there is residual tumor.3
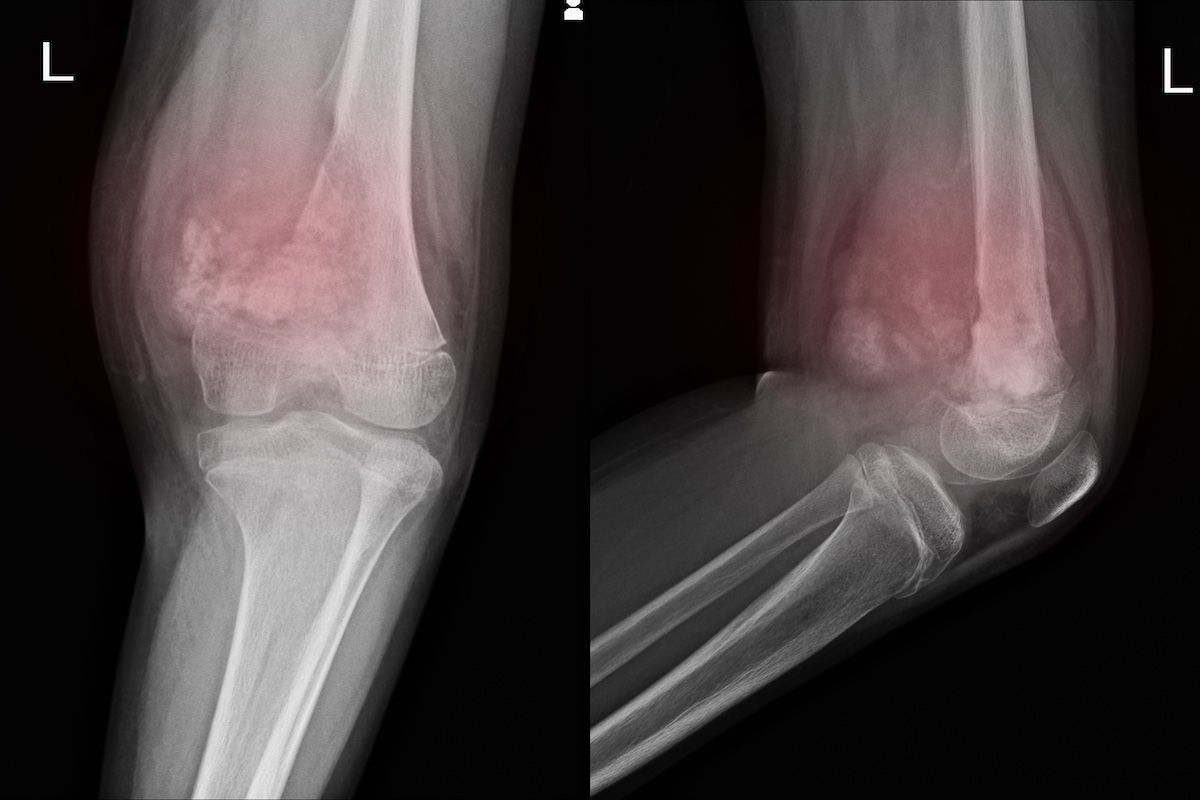
In both patient group in this analysis, the most common diagnosis in 28% of each group was undifferentiated pleomorphic sarcoma | Image Credit: RichmanPhoto-stock.adobe.com
“One of the major problems in resolving this quandary is the absence of high-quality randomized studies,” the present study authors wrote.1 “Consequently, a control group comparing the results of re-excision to a more conservative approach is missing in most of the studies.”
They published their findings in a recent issue of Cancers (Basel) of their investigation into 185 patients who had an unplanned resection at LMU University Hospital in Munich, Germany. Among these patients, 156 underwent a subsequent re-excision (Group A; mean age, 57 [range, 13-93] years; 50.6%, female patients) and 29 did not or received conservative treatment (Group B; mean age, 60 [range, 31-85] years; 48.3%, female patients). The outcomes of interest were LR, LR-free survival, and OS as seen via R0 resection. Radiotherapy or chemotherapy were also administered when clinically indicated.
Among the 156 patients who underwent a subsequent re-excision, the most common diagnosis was undifferentiated pleomorphic sarcoma (UPS; 28%), followed by myxofibrosarcoma (17%), leiomyosarcoma (12%), and liposarcoma (10%). UPS was also the most common diagnosis among the 29 patients who did not undergo a subsequent re-excision (28%), but followed by liposarcoma (24%) and malignant peripheral nerve sheath tumor (10%).
Tumor depth was more extensive in the smaller patient group; 97% of these patients had tumors with a subfascial location vs 64% of the patients who underwent re-resection. On the other hand, tumors were more often superficial in the reresection cohort, at 36% vs 3%.
Grade 3 lesions were seen in 39% of each patient group, grade 2 lesions in 35% each, and grade 1 lesions in 15 each. The authors highlighted that the among the patients treated conservatively, tumor size was significantly larger (P < .0001), and among the patients who underwent reresection, their initial incomplete resections necessitated a subsequent wide reresection or neoadjuvant radiotherapy. In the conservative group, 9 received just adjuvant radiotherapy; 5, just chemotherapy; and 14, radiotherapy and chemotherapy.
Median follow-ups were 40 months in Group A and 43 months in Group B. Eight percent and 14%, respectively, showed signs of LR during the study’s observation period, which the study authors said was statistically insignificant; residual disease was seen in 10.8% and 3.2% of these patients, respectively. OS and LR-free survival did not differ between the groups, and receipt of radiotherapy was shown to not affect patient survival outcomes.
Subsequent metastatic disease was seen in 15% of Group A and 10% of Group B. Of these 27 patients (24 in Group A and 3 in Group B), 16% of Group A and 24% of Group B died during the study’s observation period.
“In [our] opinion, it is imperative to engage in a comprehensive discussion with the patient regarding these findings. A re-resection procedure, if uncomplicated, holds promise to improve the OS and lower the risk of LR,” the study authors concluded. “However, in cases where the anatomic location (ie, pelvis, spine) poses difficulties, this potentially compromises limb function due to mutilating surgical procedures. A routine re-resection should be avoided if no gross residual disease is observed.”
The authors note that it is safe to proceed with re-resection in most cases, but that for low-grade lesions, considering the extent of the surgery and risk of complications, a more conservative approach may be necessary.
Limitations on application of these findings to a wider patient population include that the study was retrospective, the nonresected patient group was small, and study inclusion criteria encompassed sarcomas and all of its subcategories.
References
1. Fromm J, Klein A, Mentrup F, et al. Unplanned resections of soft tissue sarcomas-necessity of re-resection? Cancers (Basel). 2024;16(10):1851. doi:10.3390/cancers16101851
2. Williams AK. The ‘whoops’ procedure. Presented at: COA 2017; April 27-28, 2017; Kissimmee, FL. https://coa.org/2017/presentations/Saturday/12WilliamsAmy.pdf
3. Hermanek P, Wittekind C. The pathologist and the residual tumor (R) classification. Pathol Res Pract. 1994;190(2):115-123. doi:10.1016/S0344-0338(11)80700-4
