- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Evidence, Support, and Education Needed to Drive Precision Oncology, Accenture’s Bogdan Says
Accenture’s 2021 report, “The Future Is Now: How to Drive Precision Oncology Adoption," adds to the chorus calling for greater sharing of data and improved standardization, so that academic centers and community practices alike can continually improve data sets used worldwide.
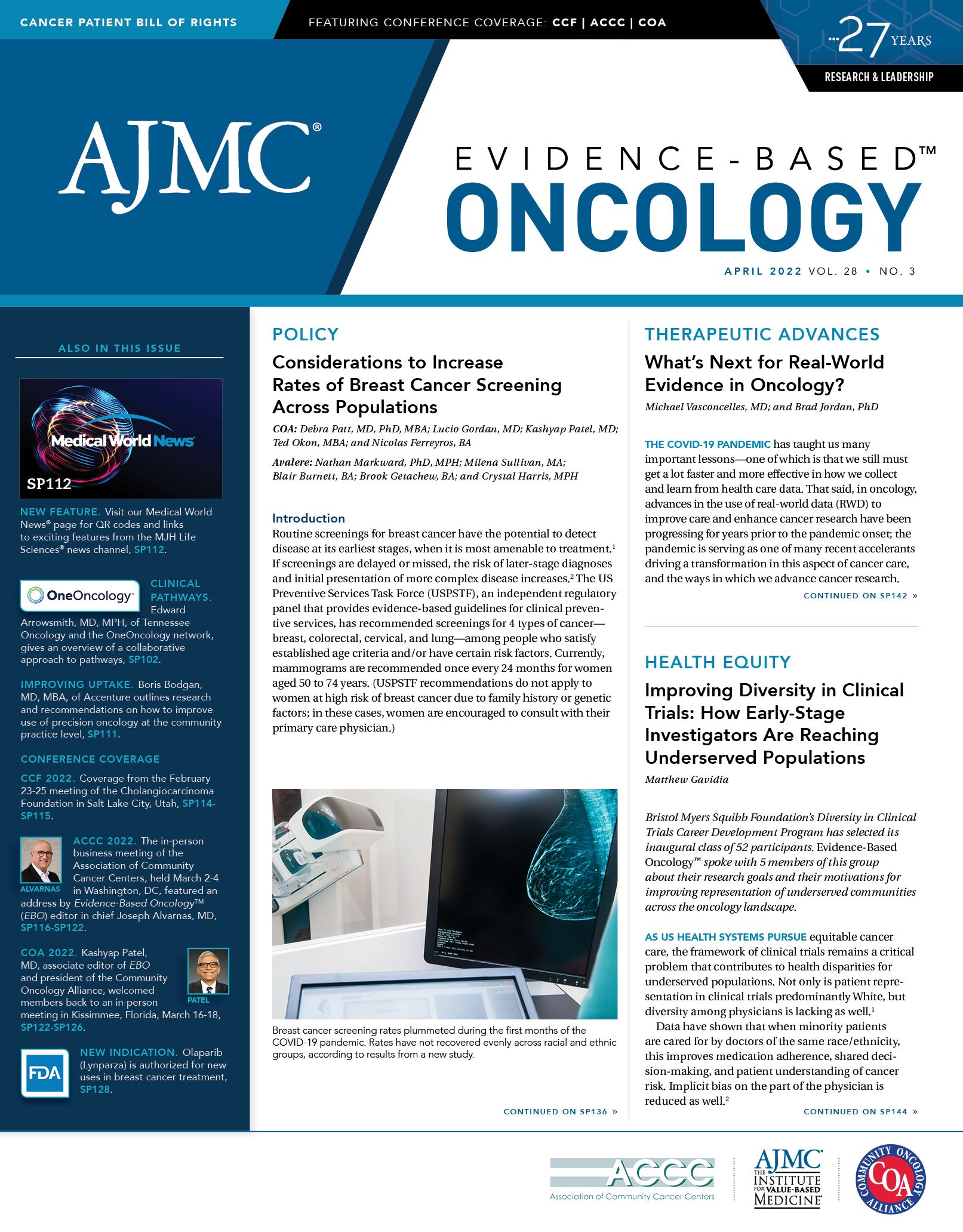
Improving uptake of precision medicine in community oncology practices will require a multistep process to arm physicians with both the right data and the right support, along with a rethinking of how education occurs, according to a global leader in medical technology.
Boris Bogdan, MD, MBA, managing director and global lead, Medical Practice and Center of Excellence for Precision Oncology, Accenture, discussed a survey of oncologists’ views—along with recommendations on how to bolster precision medicine—during an interview with Evidence-Based Oncology™.
The results and recommendations were included in Accenture’s 2021 report, “The Future Is Now: How to Drive Precision Oncology Adoption.”1 The report adds to the chorus calling for greater sharing of data and improved standardization, so that academic centers and community practices alike can continually improve data sets used worldwide. Accenture’s findings align with the discussion held with global experts in real-world evidence (RWE) during a symposium at the American Society of Hematology 63rd Annual Meeting & Exposition in December 2021.2
Precision oncology is considered the future of cancer care: The Accenture report cites a 2019 study estimating that up to 50% of patients could benefit from this approach.3 And yet, Accenture’s engagement of 130 oncologists in the United States and Europe found that 29% reported the practice of matching a treatment to a particular patient was not widely adopted in their daily work.1
Accenture has set out to hear directly from oncologists—especially those in community practice—about what it would take to achieve broader uptake of precision oncology, Bogdan said. This mission, he explained, “is to really understand what is it that they need in their everyday practice to be more successful.”
According to the report:
- 85% of respondents ranked outcomes and longitudinal data as the most critical data source to share.
- 20% or less of oncologists today do not routinely participate in molecular tumor boards or use clinical decision support tools.
- 66% of oncologists believe clinical practice is changing rapidly and will require them to master new skill sets.
“We’ve seen a significant difference between what somebody in a community practice needs vs somebody in academic medical center,” noted Bogdan, who is based on Basel, Switzerland. But both have needs in common: The groups of oncologists all have the desire to discuss specific therapies with colleagues.
The intersection between these two, he said, is the “sweet spot,” where the right type of data and decision support can make a difference. Technology can give community oncologists the same level of feedback and guidance that can be found within an academic center, where tumor boards allow for deep exchanges.
Accenture’s report outlines a 3-step process:
1. Arming oncologists with the right evidence;
2. Offering clinical decision support to address uncertainties; and
3. Education that offers a “comprehensive foundational understanding of precision oncology.”
Giving oncologists at every level the right access to data, and the ability to discuss specific cases, is needed to take geography out of the equation in delivering quality care, Bodgan said. Already, some oncologists recommend genomic testing for every patient, although that is not the norm today.
And yet, Bodgan continued, even patients can gain access to testing, oncologists still have questions. What might be the right analytical diagnostic tools? What is the right biomarker?” Accenture’s engagement has shown the need for an educational component, with opportunities for peer-to-peer discussions on the best approach. The former practice of just picking up the phone and calling someone is insufficient, given the amount of information a community oncologist must absorb.
Moving from the era of “medicine by anecdote” to true evidence-based practice requires what Bodgan described as a middle step. If data sharing becomes uniform and widespread, the possibility exists for “medicine by crowdsourcing,” in that clinical opinion will still matter, but there will be strength in numbers and data behind it.
A community oncologist, Bodgan said, still appreciates the chance for a personal connection. “They appreciate having that quick break in the day to have chat and an exchange,” he said. This is especially true if access to a tumor board is limited or unavailable. Developing support tools that can create these opportunities would be valuable, based on Accenture’s findings, he said. A key will be to bring standardization to the data sharing process, which Bodgan said will take effort given the lack of uniformity in Europe alone.
Achieving data standardization will be a huge, expensive undertaking, Bodgan acknowledged, and the roles for academia, community oncology, payers, pharmaceutical companies, and the government are still being defined. But standardization and open source data sharing must happen.
“The quality of care 10 years from now shouldn’t be decided by whether you are living somewhere close to somebody who’s excellent,” Bodgan emphasized. “Rather, we must have a system in place, so that any place that you’re going to see an oncologist, they are enabled to make great decisions.
“We need to come to a point where we recognize that we cannot practice oncology in the future without the right data,” Bodgan said. “And when we talk about data, these are not hospital-specific data. These are data across systems—community and academic medical centers—all sharing to benefit the patient. That is where I hope we are going to get.”
References
1. Dupuy F, Ohnmacht F. The future is now: how to drive precision oncology adoption. Accenture Life Sciences. April 23, 2021. Accessed March 20, 2022. https://www.accenture.com/us-en/insights/life-sciences/precision-oncology
2. Caffrey M. ASH 2021 recap: real-world evidence. Am J Manag Care. 2022;28(SP1):SP47-SP48.
3. Sicklick JK, Kato S, Okamura R, et al. Molecular profiling of cancer patients enables personalized combination therapy: the I-PREDICT study. Nat Med. 2019;25(5):744-750. doi:10.1038/s41591-019-0407-5
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
