- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Considerations to Increase Rates of Breast Cancer Screening Across Populations
Authors from the Community Oncology Alliance and Avalere Health present data that show breast cancer screening rates recovered more slowly among some racial/ethnic groups following on the onset of the COVID-19 pandemic.
ABSTRACT
Objectives: COVID-19 has caused considerable drops in utilization of breast cancer screening services during the pandemic, especially among certain racial and ethnic groups. Members of the Community Oncology Alliance (COA)—including the COA president, South Carolina oncologist Kashyap Patel, MD—have reported increases in patients, particularly those of color, presenting with stage III and IV cancer at diagnosis. According to data released by the Biden administration, more than 9.5 million recommended cancer screenings had been missed in the United States as a result of the COVID-19 pandemic, as of February 2022. President Joe Biden and First Lady Jill Biden, EdD, aim to address this in the 2022 revitalized Cancer Moonshot Initiative. The findings made by COA as well as by Avalere also suggest that the pandemic has exacerbated existing health care disparities.
Methods: Using a multipayer database, we analyzed breast cancer screening rates for 2 periods—March 1 to September 30, 2019, and March 1 to September 30, 2020—among Medicare fee-for-service (FFS), managed Medicaid, and commercial insurance beneficiaries to understand the potential impact of the COVID-19 pandemic on adherence to the US Preventive Services Task Force breast cancer screening recommendations, which are currently undergoing review. Screening rates were evaluated across 5 racial/ethnic groups and by payer type.
Results: Mean monthly mammogram screening rates among eligible White Medicare FFS beneficiaries dropped to 0.6% in April 2020, but these screening rates recovered to 6.5% by June 2020. Screening rates for eligible Black Medicare FFS beneficiaries recovered on a pace slightly slower than that of White beneficiaries, but more rapidly than that of other groups. By comparison, American Indian/Alaska Native beneficiaries had a mean monthly screening rate of 0.5% in April 2020, which recovered to 3.1% in June 2020; these were below 2019 screening rates of 4.2% for April and 3.9% for June. Differences in screening rates by payer type were also observed. Patients with commercial insurance had higher screening rates compared with those covered by Medicare FFS and managed Medicaid.
Conclusions: Our principal finding shows that mean breast cancer screening rates decreased in April 2020 across all payers, but recovery to prepandemic screening levels has occurred more slowly among certain racial and ethnic minority groups. Differences in recovery rates by payer type highlight a strong relationship between income level and screening utilization.
https://doi.org/10.37765/ajmc.2022.88855
INTRODUCTION
Routine screenings for breast cancer have the potential to detect disease at its earliest stages, when it is most amenable to treatment.1 If screenings are delayed or missed, the risk of later-stage diagnoses and initial presentation of more complex disease increases.2 The US Preventive Services Task Force (USPSTF), an independent regulatory panel that provides evidence-based guidelines for clinical preventive services, has recommended screenings for 4 types of cancer—breast, colorectal, cervical, and lung—among people who satisfy established age criteria and/or have certain risk factors. Currently, mammograms are recommended once every 24 months for women aged 50 to 74 years. (USPSTF recommendations do not apply to women at high risk of breast cancer; in these cases, women are encouraged to consult with their primary care physician.)
USPSTF recommendations play a significant role in ensuring coverage for preventive services, such as cancer screenings. Under federal law, all private payers and Medicare are required to cover services that are given “A” or “B” recommendations from USPSTF.3 The only exception is the Medicaid market, where there is variability from state to state in how preventive services are covered.
Study results have highlighted the effect of the March 2020 public health emergency (PHE) in response to the COVID-19 pandemic on cancer screening rates4,5 and how the PHE widened health care disparities among racial and ethnic groups.6 In November 2020, we reported sharp declines in cancer care, including screenings, following the declaration of the PHE.7 In June 2021, data reported by the CDC showed an 87% drop in breast cancer screening rates in April 2020, compared with prepandemic rates.8
Disparities in screening rates predate the pandemic. A decade ago, data published prior to passage of the Affordable Care Act found disparities in access to high-quality mammography, with Black and Hispanic women without insurance less likely to have access.9 In 2017, Narayan et al found that income, education level, and access to insurance were predictors of screening rates.10
In May 2021, USPSTF published a Final Research Plan as part of the organization’s effort to update its breast cancer screening guidelines, devoting considerable attention to reassessing how health equity and social determinants of health (SDOH) contribute to discrepancies in breast cancer screening, diagnosis, treatment, and outcomes.11 The impact of the COVID-19 pandemic on utilization of breast cancer screenings and subsequent advanced-stage diagnoses for many patients highlights the need for revised breast cancer screening recommendations.
Although a report from a Massachusetts health system in review of 192,060 patients undergoing cancer screening found that cancer screenings returned to nearly prepandemic levels between June and September 2020,4 we sought to examine a multipayer data set to determine if the recovery in breast cancer screenings was felt evenly across ethnic and racial subgroups and if there were any differences in recovery rate based on insurance status. According to analyses from the US Census Bureau, beneficiaries with commercial health insurance are more likely to have higher incomes than those enrolled in Medicare fee-for-service (FFS) or managed Medicaid.12
DATA AND METHODS
The Community Oncology Alliance (COA) and Avalere Health conducted an evaluation to measure and compare adherence to USPSTF breast cancer screening guidelines prior to the COVID-19 pandemic (March 1 to September 30, 2019) and during the PHE (March 1 to September 30, 2020) across multiple payer populations and social risk factors (eg, race/ethnicity, income). The analysis utilized Inovalon’s MORE2 Registry, a multipayer database that captures the enrollment and claims data of more than 338 million Medicare FFS, Medicare Advantage, managed Medicaid, and commercial beneficiaries, and Acxiom’s InfoBase Geo database to link and integrate patient-specific SDOH information at the 5-digit zip code level.
RESULTS
Racial/ethnic disparities. Our results illustrate patterns of mammogram use among 5 racial/ethnic groups in the period from March 2020 to September 2020, covering the onset of the pandemic, the declaration of the PHE, and the period when screening rebounded after the initial decline. The illustrations compare this 6-month period with the corresponding period in 2019. Results are presented for 5 groups: White, Black/African American (hereafter, Black), Hispanic/Latino (hereafter, Hispanic), Asian/Native Hawaiian/Pacific Islander (hereafter, Asian), and American Indian/Alaskan Native. Data presented below show that mammogram utilization among 3 groups (Asian, Hispanic, and American Indian/Alaskan Native) was already lower in 2019 than utilization among White beneficiaries and, moreover, dropped even more precipitously at the start of the pandemic in 2020 (FIGURE 1).
In like manner, Figure 1 highlights how breast cancer screening utilization recovered more rapidly in White and Black subgroups during the period immediately following declaration of the PHE and prior to the emergence of the Delta and Omicron COVID-19 variants.
FIGURE 1.
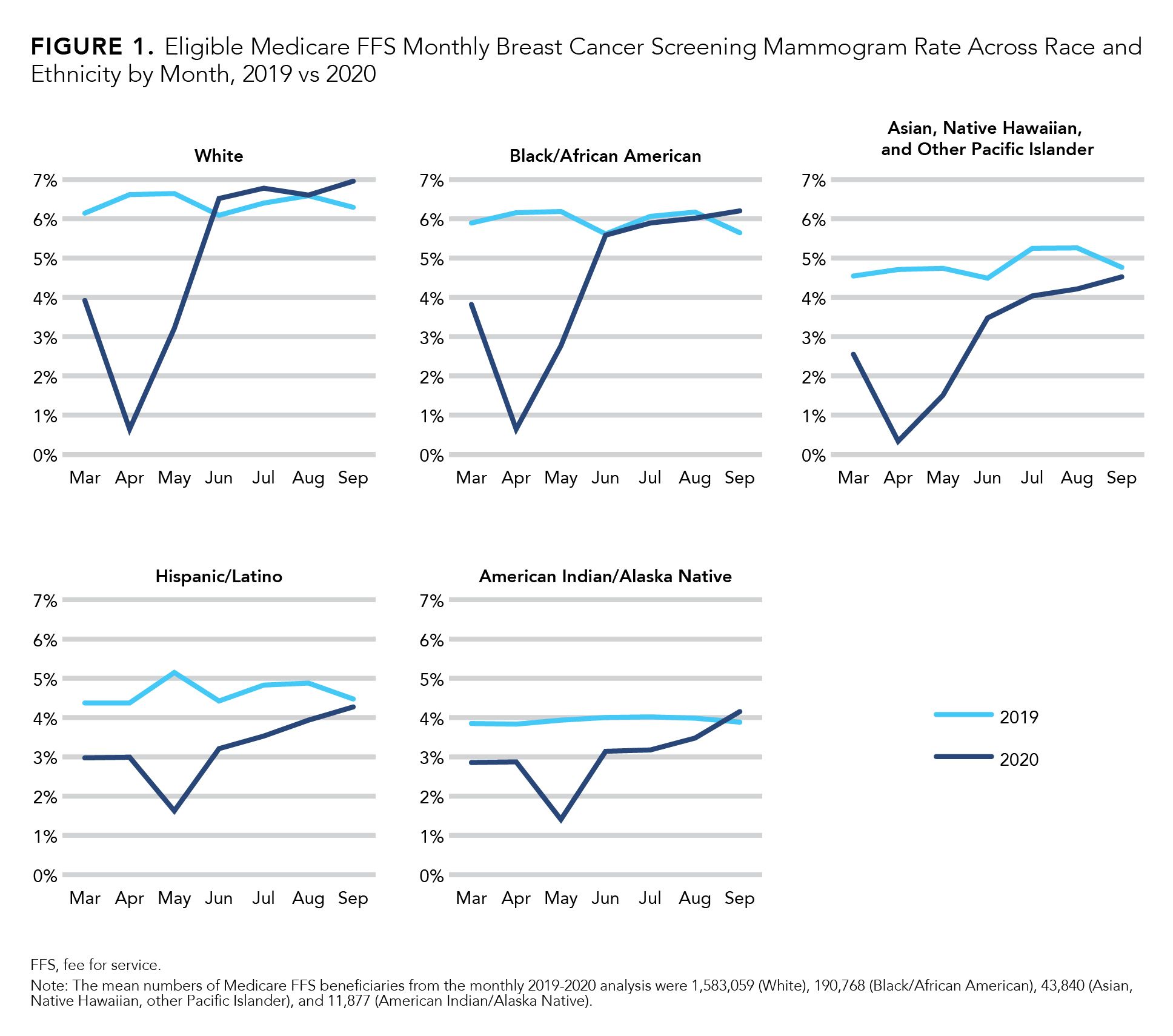
Meanwhile, the analysis found that the Asian, Hispanic, and American Indian/Alaskan Native groups did not experience a rebound in screening rates until September 2020, and eligible Asian and Hispanic Medicare beneficiaries’ screening rates did not fully recover during the same period. This observation aligns with findings published in the Journal of Clinical Imaging that showed higher mammogram cancellation rates among non-White patients.13
The trend in monthly screening across race and ethnicity categories was also observed in the screening utilization patterns over a 24-month period—a critical shift as USPSTF guidelines on breast cancer screening for women aged 50 to 74 years recommends screening every 2 years.
Disparities by payer type. Screening rate disparities were also observed across payers (FIGURE 2). Data on prepandemic screening rates showed that managed Medicaid beneficiaries had the lowest screening rates, compared with individuals covered by commercial and Medicare FFS policies. Furthermore, Figure 2 underscores that adherence to the USPSTF 24-month breast cancer screening guidelines is consistently lower for managed Medicaid beneficiaries, demonstrating the need to better understand the downstream implications of delayed screening across these subpopulations. Indeed, USPSTF recommendations for screening do not dictate Medicaid coverage in the same way they do for commercial and Medicare FFS patients, and screening utilization in this population remains low.
FIGURE 2.
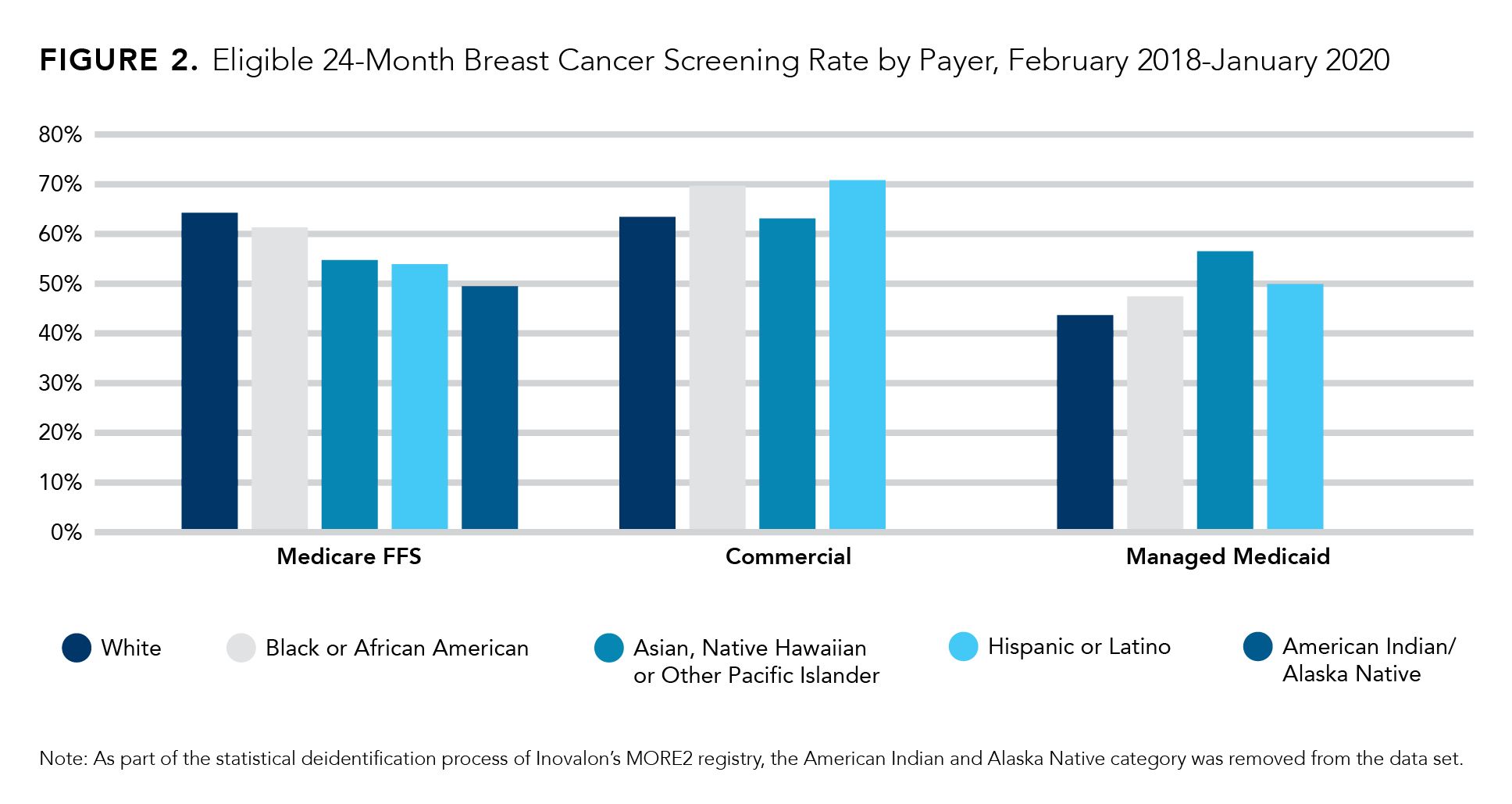
Avalere’s review also identified a strong relationship between rates of screening and median household income, regardless of race and ethnicity, consistent with earlier findings.14 Specifically, screening rates increased as a function of median household income, dividing patients into approximately 3 income groups: less than $40,000, $40,000 to $75,000, and $75,000 and above. The relationship was observed in both the commercial and managed Medicaid markets, although the relationship between increased screening utilization and higher income level was more prominent in the commercial segment.
DISCUSSION
Given these findings, addressing screening inequities related to race, ethnicity, and income should be a top priority for patients and providers. First and foremost, USPSTF screening recommendations provide a pathway to coverage for many preventive services without cost sharing in the commercial and Medicare markets.
In addition, current recommendations for cancer screenings do not systematically address disparities in care, namely that adherence to preventive service recommendations is lower among certain racial and ethnic minority groups, illustrating historical inequities in provision of services and outcomes that disproportionately affect minority populations.15 Timely screening is only one part of ensuring prompt diagnosis to improve equity in outcomes across subpopulations with increased social risk factors. Essential follow-up tests and procedures may not be covered by insurance, further delaying timely diagnosis and treatment of disease.
The disruption to cancer screening delivery during the COVID-19 pandemic will have a long-term impact on cancer care. Providers predict later-stage diagnoses and significantly worse outcomes.16 As the president of COA, South Carolina oncologist Kashyap Patel, MD, told The Washington Post, “COVID-19 put cancer and health care disparities on steroids.”17
USPSTF recommendations allow for coverage of preventive screening services receiving an “A” or “B” grade from the Task Force without cost sharing. Beyond USPSTF recommendations, there are a broader set of cancer prevention services that play an important role in the timely diagnosis of cancer. Coverage of these services among public and private plans, as well as value-based insurance design arrangements, is paramount in addressing delays in diagnosis, treatment, and care.
Limitations
This study had several limitations. When analyzing the impact of SDOH factors, mean screening rates were based on a patient’s 5-digit zip code. For example, trends by median household income were based on the 5-digit zip code of the patient and not the individual patient’s income. Furthermore, USPSTF screening guidelines offer minimum coverage of screening services for preventive care, in comparison with other breast cancer screening organization guidelines such as those of the American Cancer Society and the National Comprehensive Cancer Network. Other forms of screening and preventive services for early detection of breast cancer are cited and included in guidelines across multiple other compendia, but for the purpose of this assessment, we only reviewed screening adherence rates in comparison with USPSTF guidelines.
There were also differences in the mean number of beneficiaries included across insurance types (ie, Medicare FFS, commercial, and managed Medicaid) and time frames (ie, monthly profile analysis and 24-month profile analysis). For Medicare FFS, a 20% random sample of all Medicare FFS enrollees was used. For commercial and managed Medicaid beneficiaries, a convenient sample of those enrollees was used. There were limitations in insights into beneficiaries who switched payers outside of the sample used. In addition, there were limitations in race/ethnicity data; this information was sourced from payers, where either race or ethnicity is known. Information on biracial and multiracial beneficiaries is typically not known.
CONCLUSIONS
Given that USPSTF is currently in the Final Research Plan stage of updating draft recommendations for breast cancer screening, a final recommendation statement is imminent. Access to high-value preventive services can improve the speed of cancer diagnosis as well as increase adherence to recommended follow-up procedures and treatments for these patients. A broader set of stakeholders and targeted care delivery and communications can help close these gaps in care. Notably, the Cancer Moonshot initiative intends to leverage stakeholders such as government partners, business community, and nonprofit sectors to address inequities in screening, diagnostics, and treatment across race, gender, socioeconomic status, and other SDOH risk factors. To the extent to which some of these disparities disproportionally impact breast cancer outcomes for different populations, policies that reverse these trends, to target high-risk populations for screenings and to incorporate broader payment and delivery innovation for cancer care, may be warranted.
Author Information
For the Community Oncology Alliance (COA): Patt, of Texas Oncology, member of the executive committee; Gordan, of Florida Cancer Specialists and Research Institute, member of the board of directors; Patel, of Carolina Blood and Cancer Care Associates, president; Okon, executive director; and Ferreyros, managing director of policy, advocacy, and communications. For Avalere Health:Markward, principal research scientist; Sullivan, principal; Burnett, manager/consultant; Getachew, senior associate; and Harris, senior policy associate.
References
- NCI Staff. For cancer screening, COVID-19 pandemic creates obstacles, opportunities. National Cancer Institute Cancer Currents blog. March 10, 2021. Accessed February 19, 2022. https://www.cancer.gov/news-events/cancer-currents-blog/2021/cancer-screening-decreases-coronavirus-pandemic
- Cavallo J. How delays in screening and early cancer diagnosis amid the COVID-19 pandemic may result in increased cancer mortality. The ASCO Post. September 10, 2020. Accessed February 14, 2022. https://www.ascopost.com/issues/september-10-2020/how-delays-in-screening-and-early-cancer-diagnosis-amid-the-covid-19-pandemic-may-result-in-increased-cancer-mortality/
- Patient Protection and Affordable Care Act, P.L.111-148, 42 USC§300gg–13. Coverage of preventive health services (2010).
- Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh Q-D. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. 2021;7(3):458-460. doi:10.1001/jamaoncol.2020.7600
- London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020;4:657-665. doi:10.1200/CCI.20.00068
- Wang QQ, Berger NA, Xu R. Analysis of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. 2021;7(2):220-227. doi:10.1001/jamaoncol.2020.6178
- Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059-1071. doi:10.1200/CCI.20.00134
- Sharp declines in breast and cervical cancer screening. News release. CDC; June 30, 2021. Accessed February 19, 2022. https://www.cdc.gov/media/releases/2021/p0630-cancer-screenings.html
- Rauscher GH, Allgood KL, Whitman S, Conant E. Disparities in screening mammography services by race/ethnicity and health insurance. J Women’s Health (Larchmt). 2012;21(2):154-160. doi:10.1089/jwh.2010.2415
- Narayan A, Fischer A, Zhang Z, Woods R, Morris E, Harvey S. Nationwide cross-sectional adherence to mammography screening guidelines: national Behavioral Risk Factor Surveillance System survey results. Breast Cancer Res Treat. 2017;164(3):719-725. doi: 10.1007/s10549-017-4286-5
- Final research plan – breast cancer: screening. US Preventive Services Task Force. May 6, 2021. Accessed February 19, 2022. https://www.uspreventiveservicestaskforce.org/uspstf/document/final-research-plan/breast-cancer-screening1
- Keisler-Starkey K, Bunch LN. Health insurance coverage in the United States: 2020. report number P60-274. US Census Bureau. September 14, 2021. Accessed February 23, 2022. https://www.census.gov/library/publications/2021/demo/p60-274.html
- Amornsiripanitch N, Chikarmane SA, Bay CP, Giess CS. Patients’ characteristics related to screening mammography cancellation and rescheduling rates during the COVID-19 pandemic. Clin Imaging. 2021;80:205-210. doi:10.1016/j.clinimag.2021.07.009
- Kim E, Moy L, Gao Y, Austen Hartwell C, Babb JS, Heller SL. City patterns of screening mammography uptake and disparity across the United States. Radiology. 2019;293(1):151-157. doi:10.1148/radio.2019190647
- Nonzee NJ, Ragas DM, Luu TH, et al. Delays in cancer care among low-income minorities despite access. J Women’s Health (Larchmt). 2015;24(6):506-514. doi:10.1089/jwh.2014.4998
- Nierengarten MB. ASTRO survey details effects of COVID-19 on radiation oncology. Cancer. 2021;127(16):2827. doi:10.1002/cncr.33786
- McGinley L. Covid and cancer: a dangerous combination, especially for people of color. The Washington Post. October 11, 2021. Accessed February 19, 2022. https://www.washingtonpost.com/health/2021/10/11/covid-cancer-delayed-diagnosis/