- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
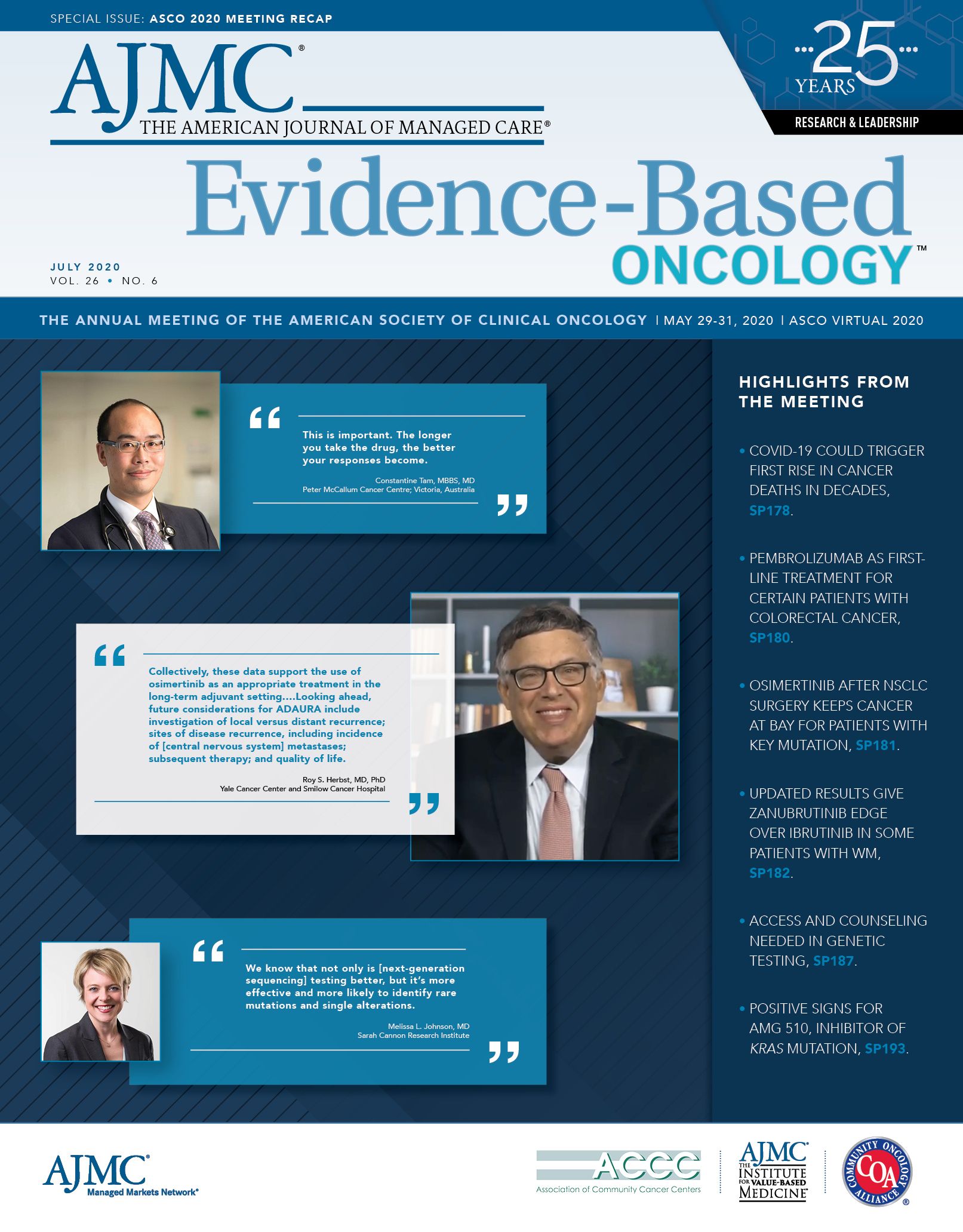
COVID-19 and Cancer: NCI's Sharpless Says COVID-19 Could Halt Streak of US Cancer Mortality Gains
The talk by Ned Sharpless, MD, director of the National Cancer Institute, preceded presentations on some of the earliest findings about the effects of COVID-19 on cancer: It appears that patients treated with chemotherapy for lung or thoracic cancer shortly before being diagnosed with COVID-19 face a higher risk of death, and so do patients with cancer who take the combination of hydroxychloroquine (HCQ) and azithromycin.
Months of deferred screenings or delayed treatments due to coronavirus disease 2019 (COVID-19) could reverse the US streak in improved cancer mortality that has lasted more than 25 years, said Norman E. “Ned” Sharpless, MD, director of the National Cancer Institute (NCI), during the American Society of Clinical Oncology (ASCO) 2020 Annual Meeting, presented in a virtual format due to the pandemic.
Sharpless, who served briefly as acting FDA commissioner in 2019, opened the virtual session on “Cancer and COVID-19” with a sober assessment of COVID-19’s effects on both clinical care and cancer research.
His talk preceded presentations on some of the earliest findings about the effects of COVID-19 on cancer: It appears that patients treated with chemotherapy for lung or thoracic cancer shortly before being diagnosed with COVID-19 face a higher risk of death, and so do patients with cancer who take the combination of hydroxychloroquine (HCQ) and azithromycin.
The separate data sets help shape an emerging picture of what patients with cancer face under COVID-19: They are more likely to be older or have underlying health problems, which are known to make the virus more deadly.
And, as explained by Jeremy L. Warner, MD, MS, an associate professor of medicine at Vanderbilt University Medical Center, patients may be immunosuppressed, from the treatment or the disease itself, and have more frequent contact with the health care system than people without cancer.
Deferred Care Will Come at a Price
The decision to preserve hospital and clinical capacity was “necessary and important” as COVID-19 peaked this spring, Sharpless said, “But all this deferred care—it’s going to have costs for patients with cancer,” he noted. “It may mean more cancer suff ering outcomes for our patients. What we don’t know yet is the scale of these bad outcomes.”
Each year, Sharpless said, NCI works with the American Cancer Society and others to publish an annual report on the state of cancer, and the declining mortality rates have become an annual “shot in the arm” for cancer researchers. “My fear is that diminished cancer care will produce a negative impact on these cancer statistics of relevance to the public health. And we expect to see these trends play out over several years,” he said. “We cannot escape this reality.”
Research is taking a hit, too, as patient accruals in NCI trials have fallen off pace, and Sharpless said he had heard similar reports about industry-sponsored trials. What has fi lled the gap somewhat, he said, are aggressive efforts to start trials to understand COVID-19’s eff ect on patients with cancer. He highlighted 2 groups presenting results during the ASCO meeting, as well as registries set up by ASCO and the American Society of Hematology.
On May 21, 2020, NCI launched the COVID-19 in Cancer Patients Study1 that will enroll 2000 patients with cancer who are diagnosed with COVID-19. “We aim to conduct the study at more than 1000 sites,” Sharpless said. “We need to know as much about the impact of COVID-19 on cancer patients in Montana as we do
about those in New York.”
He asked, rhetorically, “What have you learned about the impact of the virus on patients across racial and ethnic groups?” Sharpless pointed out that the NCI effort “is not a registry” but a trial approved by an institutional review board; investigators will seek patient consent to collect samples, analyze biomarkers, and develop germline sequencing of patients.
Patients who participate will be required to have regular health care visits, during which the facility will collect blood samples and copies of routine imaging scans for up to 2 years. “It’s important to note that participation in this study will not require additional visits to the hospital or other facilities,” Sharpless said. “Much of the data will be collected electronically and some of the tests will be part of the patient’s routine care.”
Results From TERAVOLT
Prior smoking history or lung damage are among the characteristics that put patients with thoracic cancer at particular risk from COVID-19, according to insights gleaned from 400 patients’ records in the Thoracic cancERs international coVid 19 cOLlaboraTion (TERAVOLT) registry.2 Thoracic cancers include lung
tumors, mesothelioma, carcinoid tumors, and thymic neoplasms.
According to the researchers, use of chemotherapy within 3 months of a COVID-19 diagnosis turned out to have a particularly strong association with early death: a 64% increased risk of dying from the virus. The effect of chemotherapy was seen whether or not patients also had other therapies, such asœimmunotherapy,œwhich showed up as a potential risk factor in an earlier study.3
Of the 400 patients, 144 died: 79.4% (n = 112) from COVID-19, 10.6% (n = 15) from cancer, and the rest from other causes. Treatments with anticoagulants and corticosteroids were also linked to increased death risk, adding to existing concerns about the use of corticosteroids for patients with chronic disease. More data will be needed to draw any fi rm conclusions about the use of anticoagulants.
Lead author Leora Horn, MD, MSc, commented on the speed with which the research eff ort has taken shape. “In less than a week, we had a study enrolling patients,” said Horn, who is the Ingram Associate Professor of Cancer Research and the director of the thoracic oncology program at Vanderbilt University Medical Center. “We have seen clinical trials being funded, approved, and enrolling patients within weeks, when it can often take months or years to get approval for a trial.”
Cancer and the Cocktail
Cancer patients with COVID-19 who were treated with both HCQ and azithromycin were 3 times more likely to die during the 30 days after they were diagnosed with COVID-19, according to fi ndings4 presented by Warner, lead author of the study from the COVID-19 and Cancer Consortium, which launched its registry March 15.
Warner cautioned that the association is of “uncertain validity” and may stem from residual confounding. “For example,” he said, “patients receiving this combination were more likely to have severe disease or more likely to be hospitalized.”
The researchers also reported that neither drug was associated with an added mortality risk when taken alone.
After some statistical adjustments, the researchers found that patients with worsening cancer were 5 times more likely to have died within 30 days of their COVID-19 diagnosis than patients in remission or with no evidence of disease.
Of the 928 people with cancer and COVID-19 who were included in the study, 121 (13%) died within 30 days of their COVID-19 diagnosis, according to fi ndings that Warner presented. The written abstract, submitted earlier to meet ASCO deadlines, had slightly diff erent numbers: 1108 cases and 106 deaths, or 10.4% of the total cases.
In their analysis of the cases and deaths, the researchers found that factors associated with a 30-day mortality risk including worsening, progressing, or active cancer; older age; male sex; and being a former smoker.
Only 3 of the 121 deaths that Warner discussed in his video presentation were of people with no comorbidities. Of the 466 who were hospitalized, 106 died.References
1. NCI COVID-19 in Cancer Patients Study (NCCAPS). National Cancer Institute. May 21, 2020. Accessed May 30, 2020. https://www.cancer.
gov/research/keyinitiatives/covid19/coronavirusresearchinitiatives/nccaps
2. Horn L, Whisenant JG, Torri V, et al. Thoracic Cancers International COVID19 Collaboration (TERAVOLT): impact of type of cancer therapy and COVID therapy on survival. J Clin Oncol. 2020;38(18 suppl; abstr LBA111). doi:10.1200/JCO.2020.38.18_suppl.LBA111
3. Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARSCoV2: a multicenter study during the COVID19 outbreak.’Cancer Discov. 2020;10(6):783791. doi:10.1158/21598290.CD200422
4. Warner JL, Rubinstein S, Grivas P, et al. Clinical impact of COVID19 on patients with cancer: data from the COVID19 and Cancer Consortium (CCC19). J Clin Oncol. 2020;38(18 suppl; abstr LBA110). doi:10.1200/JCO.2020.38.18_suppl.LBA110
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More

