- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
ASCO 2020: AJMCtv Interviews
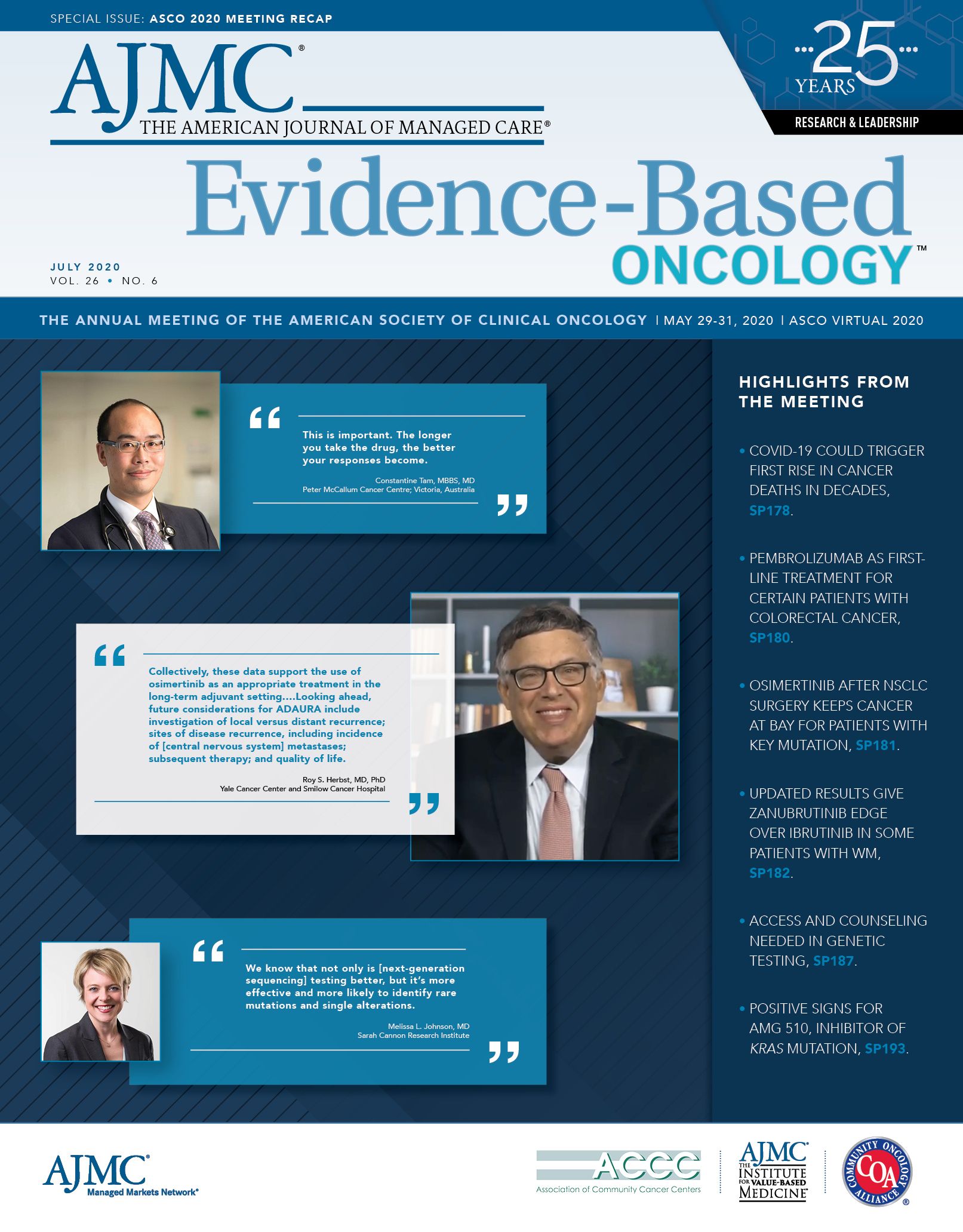
Interviews on presentations made during the 2020 Virtual meeting of the American Society of Clinical Oncology, featuring Drs Melissa L. Johnson, Constantine S. Tam, Adrian Kilcoyne, Sara L. Douglas, and Jeffrey Skolnick.
Tiragolumab Plus Atezolizumab Improves Objective Response in CITYSCAPE Trial
Blocking TIGIT, a T-cell immunoreceptor, benefi ts patients with non—small cell lung cancer in that it can restore their immune system’s antitumor response, leading to a greater objective response and progression-free survival, noted MELISSA L. JOHNSON, MD, associate director for lung cancer research at Sarah Cannon Research Institute and partner in Tennessee Oncology, in discussing the results of the CITYSCAPE trial.
At the American Society of Clinical Oncology (ASCO) meeting, you presented findings from CITYSCAPE. Can you provide some background on this trial, as well as its notable results?
CITYSCAPE is a randomized phase 2 trial. We enrolled 135 patients who were newly diagnosed with metastatic non—small cell lung cancer. They were negative for EGFR and ALK alterations, and their tumors expressed PD-L1 at least 1% or higher as tested using the Dako 22C3 assay. That assay could be done locally or centrally. Patients were randomized to receive tiragolumab, an anti-TIGIT antibody, plus atezolizumab, a PD-L1 antibody, versus placebo plus atezolizumab.
The primary end points were objective response rate and progression-free survival (PFS). The trial results showed that patients who received the combination of tiragolumab plus atezolizumab had improved objective response as well as PFS compared with patients who were treated with placebo plus atezolizumab.
What particular mechanism of action of the anti-TIGIT immunotherapy is important in the lung cancer space?
Understanding the Benefits of Zanubrutinib on Cardiac Effects
TIGIT is another inhibitory checkpoint. It works similarly to PD-L1. TIGIT is expressed on immune cells, T cells, and natural killer cells, and when it binds to its ligand, PVR, on tumor cells or antigen-presenting cells, it can blunt the immune response. In a similar way to blocking PD-1 or PD-L1, when you block TIGIT with the anti-TIGIT antibody, tiragolumab, you can restore the antitumor immune response and activate infl ammatory cells to fight the cancer.Compared with ibrutinib, the second-generation Bruton tyrosine kinase (BTK) inhibitor zanubrutinib appears to have more of a benefi t for patients in that it is associated with less atrial fi brillation and hypertension, and fewer other cardiac eff ects, explained CONSTANTINE S. TAM, MBBS, MD, clinical hematologist, Peter MacCallum Cancer Centre in Melbourne, Australia. He discussed fi ndings from the initial ASPEN study and updated results presented at ASCO.
What is it about the second-generation BTK inhibitors that might tend to cause less of these cardiac effects?
We think it’s how clean the targeting is. We don’t really know what causes hypertension and atrial fibrillation. We look at congenital BTK deficiency—humans born without BTK—and they don’t really get atrial fibrillation or hypertension. So, presumably, you can dispense with BTK and be okay from a vascular point of view. We think that ibrutinib causes some of these AEs because it’s not totally clean. So, it’s like TEC, and EGFR, and JAK3 and a whole group of other enzymes, which are structurally related to BTK.
Now, with either zanubrutinib or acalabrutinib, you get less off -target enzyme inhibition [than with ibrutinib]. And I don’t think anyone can actually put a finger on it and say, “This enzyme is causing it.” But we just know that the cleaner it is, the better the profile.
And it wasn’t just hypertension: Fibrillation and a whole multitude of other AEs, like muscle spasm, peripheral edema, pneumonitis, and pneumonia were reduced with zanubrutinib compared with ibrutinib. And I think a lot of the [cases of] sudden pneumonia were in fact pneumonitis, because there’s no real reason why there should be such a big diff erence in infective pneumonia.
Overall, the ability to stay on a drug longer seems to favor zanubrutinib. Is that a benefit of it over ibrutinib?
AstraZeneca's Kilcoyne Claims Paradigm Shift in Lung Cancer Treatment
Yes; the drug is easier to take. Fewer AEs, (adverse events) less dose reduction—people can stay on it for longer. Also, we actually examined the cumulative risk of atrial fi brillation and hypertension over time. You see that for zanubrutinib, essentially, most of the events happen in the fi rst 12 months and then it sort of plateaus. Conversely, with ibrutinib, we’ve seen an increasing cumulative pattern. This suggests that if you are going to take one of these drugs for, let’s say, 3 or 5 years, zanubrutinib may be a bit better because it has no cumulative effect on the vascular system, whereas ibrutinib appears to have one.ADRIAN KILCOYNE, MD, MBA, MPH, vice president of US Medical Affairs and Health Economics Outcomes Research for Oncology at AstraZeneca, discusses a paradigm shift in lung cancer treatment due to the overwhelming efficacy of a EGFR—tyrosine kinase inhibitor (TKI) treatment.
A lot of excitement was generated by the news that ADAURA would be unblinded due to the overwhelmingly efficacy of the EGFR-TKI treatment. Can we expect the results to be paradigm shifting?
Absolutely. As you’re aware, we’ve had some great results with osimertinib (Tagrisso) already in the metastatic setting. So, we feel there’s great promise in bringing it earlier into the disease paradigm. When we look at the ADAURA study, this is very much earlier in the longer-term curative setting; it’s in the early stages, stage IB to IIIA, meaning these are the resectable populations. What we’ve been able to demonstrate is compelling.
When any study is stopped 2 years early, that has to be done for a very good reason. As you can imagine, these data are compelling in terms of the disease-free survival benefi t we’re seeing, but they are important in a number of ways. One, the data are telling us that if you hit cancer early, well, you can have very compelling results in lung cancer. This may drive people to want to identify disease earlier, which is really important, too. The second thing is that while all these patients had surgery, not all of them had adjuvant chemotherapy. Half did, half didn’t, and regardless of that you’re seeing signifi cant benefit. So, in my
view, there will be a paradigm shift. I think you’ll see [osimertinib] will become standard of care.
Three is the question: Do you also need to give chemotherapy? And again, we don’t have enough data; we have to wait for referrals, [more] data, etc. But I think those 3 areas will see very significant changes in clinical care.
Osimertinib is already approved in the United States for the frontline setting in metastatic non—small cell lung cancer. What can we expect to see in the adjuvant setting after ASCO?
So after ASCO—and I think I’ve touched on some of the things already said—in the frontline metastatic setting, which is late-stage, disease stage IV, we have seen great results with Tagrisso. It really has become the standard of care for all intents and purpos es.…At AstraZeneca, we’re very much committed to really eliminating cancer as a cause of death, and we do understand the best chance of achieving that is to treat early, [by] identifying the right patients early. This is what ADAURA is allowing us to do: treat patients early. Now if we think about the stage IBs, those are pretty early lung cancers, and right through to stage III—that’s a broad group of patients. But if you look at those groups individually, we’re seeing benefi ts in each group. So, this is incredibly compelling for
Video Conference Interventions Are an Invaluable Resource for Those Who Choose to Participate
physicians now to be able to treat their very early lung cancers, which would probably have a good chance of cure with just resection. Still, a huge proportion of these [surgical] patients will relapse. So, for me, this is going to be a huge change in clinical care.Being part of a multidisciplinary team of oncologists, health care providers, caregivers, and patients benefits all members—not least the patients themselves—and telehealth-based interventions can help to foster these relationships. However, we should understand when patients do not want to involve their families in their care, noted SARA L. DOUGLAS, PHD, RN, the Gertrude Perkins Oliva Professor in Oncology Nursing and associate dean for research at the Frances Payne Bolton School of Nursing at Case Western Reserve University in Cleveland, Ohio.
The theme for this year’s virtual meeting was “Unite and Conquer: Accelerating Progress Together.” How does your poster on video conference interventions for distance caregivers of patients with cancer reflect this theme?
That’s such an interesting question. To be honest, I didn’t even know that was the theme of this year’s conference. So, it’s a very appropriate question. My answer, as I thought about it, is that I really think this study represented all of the good and the positive that come when all the members of the team unite for the benefit of the patient. In this research study, we had to rely on the oncologist and health care providers to participate and be involved, as well as the patient, the local caregiver, and the distance caregiver. By all of us sort of working together in conjunction with the researchers, we were able to test an intervention that’s not only going to help the distance caregiver but will potentially help patients as well.
Did you find that people were eager to participate, or were they reticent?
All of the physicians were very interested in participating. This is one of the few intervention studies I’ve done where people didn’t, you know, run and hide when they saw me coming, you know? They were very interested and engaged, as were other members of the health care team. Our refusal rate for participation was about 20%, which is less than what we usually see….It was interesting that sometimes the distance caregiver didn’t want to participate. Then again, sometimes, the patient didn’t want them to participate.
Experimental Glioblastoma Therapy Has Promise in Treatment-Resistant Cancers
[I couldn’t help but notice something] when I would be involved in talking to a patient about whether or not they were interested in the study, and then in asking if they’d give us permission to reach out to their distance caregiver. I recognized that sometimes our family members are distant for a reason. Not all families want to be together, want to share information, etc. And so I think—although some of the health care providers were very surprised at times—when a patient did not want their extended family involved, it’s very understandable. Each family unit is diff erent, and so we did have some patients and some distance caregivers who were not interested in participating.An experimental glioblastoma therapy with promising 12-month results may also have potential with other treatment-resistant cancers, according to JEFFREY SKOLNICK, MD, vice president of clinical development, Inovio Pharmaceuticals, Inc. Inovio’s experimental therapy, INO-5401, in combination with PD-1 checkpoint inhibitor cemiplimab, has shown promising results in glioblastoma.
Inovio’s experimental therapy, INO-5401, in combination with PD-1 checkpoint inhibitor cemiplimab, has shown promising results in glioblastoma. When can we expect to learn about 18-month findings?
We’re really excited about our 18-month overall survival (OS) data. As we’ve just released the OS data at 12 months, we anticipate that by the end of this year, certainly fall or winter, we will have all of the data for our 18-month OS. That’s really exciting to us.
If the 18-month findings are as exciting as the 12-month findings, then what will the next steps be?
We’re very excited to move on to a more pivotal study, for which we’ll be speaking with our potential partners. With this study, we’re collaborating with Regeneron and [its] cemiplimab, the PD-1 inhibitor that we are utilizing. We hope to continue those conversations with our collaborator, and we will move to designing a larger study and one that potentially will bring benefit to more patients.
Is there the potential for the combination of Inovio’s experimental therapy, INO-5401, and immunotherapy to work in other treatment-resistant cancers the way you’ve shown it can work in glioblastoma?
It’s key that INO-5401 is made up of 3 diff erent DNA plasmids, which make up the 5401 DNA medicine. These 3 plasmids are proteins that are often overexpressed in human tumors. It is true that specifi cally for glioblastoma, these particular proteins are important. For example, human telomerase is often—if not almost always—overexpressed in glioblastoma. But the same can be said for 2 other proteins: WT1, or Wilms’ tumor 1, protein, as well as for prostate-specific antigen. And so together, we really do have a program that has the opportunity to be studied in many other human cancers.
Final thoughts?
First, thank you very much for allowing me to share my excitement about Inovio’s therapies. I think that Inovio’s DNA medicines really have the opportunity to change the way we are treating not only patients with cancer, but patients with precancerous conditions, potentially infectious diseases, as well. And we’re really excited about the immunology and safety [data,] but most important, the efficacy data that we are seeing from our programs.
HEDIS Glycemic Goal Achieved Using Control-IQ Technology
December 22nd 2025A greater proportion of patients with type 1 diabetes who used automated insulin delivery systems vs multiple daily injections achieved the Healthcare Effectiveness Data and Information Set (HEDIS) glycemic measure.
Read More
Linking Data to Determine Risk for 30-Day Readmissions in Dementia
December 22nd 2025This study found that certain characteristics in linked electronic health record data across episodes of care can help identify patients with Alzheimer disease and related dementias at high risk of 30-day readmissions.
Read More
Performance of 2-Stage Health-Related Social Needs Screening Using Area-Level Measures
December 19th 2025Limiting health-related social needs screening to lower-income areas would reduce screening burdens; however, this study found a 2-stage screening approach based on geography to be suboptimal.
Read More
Impact of Medicaid Institution for Mental Diseases Exclusion on Serious Mental Illness Outcomes
December 17th 2025Medicaid’s Institution for Mental Diseases (IMD) rule bars federal funding for psychiatric facilities with more than 16 beds, but findings indicate that state waivers allowing treatment of serious mental illness in IMDs do not increase overall psychiatric hospitalizations.
Read More
