- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Clinical Pathways: A Critical Component of Success in Episodes of Care
https://doi.org/10.37765/ajmc.2020.42551Author Information
Lili Brillstein, MPH, is a leading advocate for episodes of care/bundled payments, with a global reputation for successfully advancing and implementing value-based care models. She is a former director of specialty care value-based models for Horizon Blue Cross Blue Shield of New Jersey and built the largest, most progressive, and most collaborative episodes of care program for commercially insured patients in the country. In July 2019, Brillstein founded BCollaborative to provide strategic advisory services to boards and C-suite stakeholders across the healthcare industry that seek to craft strategy and engagement in specialty care value-based models. She works with providers, payers, pharma, start-ups, and others to help advance the move from fee-for-service to value-based care. She has served as an advisor to CMS and is a member of the advisory board to the US Women’s Health Alliance and the Quality Cancer Care Alliance.
Brian Currie has been designing, negotiating, and implementing reimbursement solutions for major healthcare systems in the New York, New York, region for more than 25 years. He is the former senior vice president of reimbursement performance and outcomes at Northwell Health, where he created a financial framework for the system’s first extensive regional network of freestanding surgical and urgent care centers. Previously, Currie was president and chief executive officer of Long Island Health Network, leading the first clinically integrated hospital network in the country; the network gained recognition for its clinical quality improvement and financial turnaround. Currie is presently a self-employed healthcare consultant in New York.The episodes of care model is a value-based model that incorporates all the care rendered to an individual patient over the course of treatment for a particular procedure, diagnosis, or healthcare event, across the full continuum of care. This construct gives clinicians and their interdisciplinary partners a framework to explicitly and consciously collaborate in treating individuals who are clinically similar and therefore would be expected to have clinically similar outcomes. It is a model that focuses on consistently achieving the best of those outcomes.
The goal of episodes of care (or bundled payments) is to create a comprehensive treatment model that places the individual patient at the center. The model encourages communication, collaboration, and coordination across all healthcare providers—with goals of reducing unnecessary care and related costs and standardizing and optimizing both.
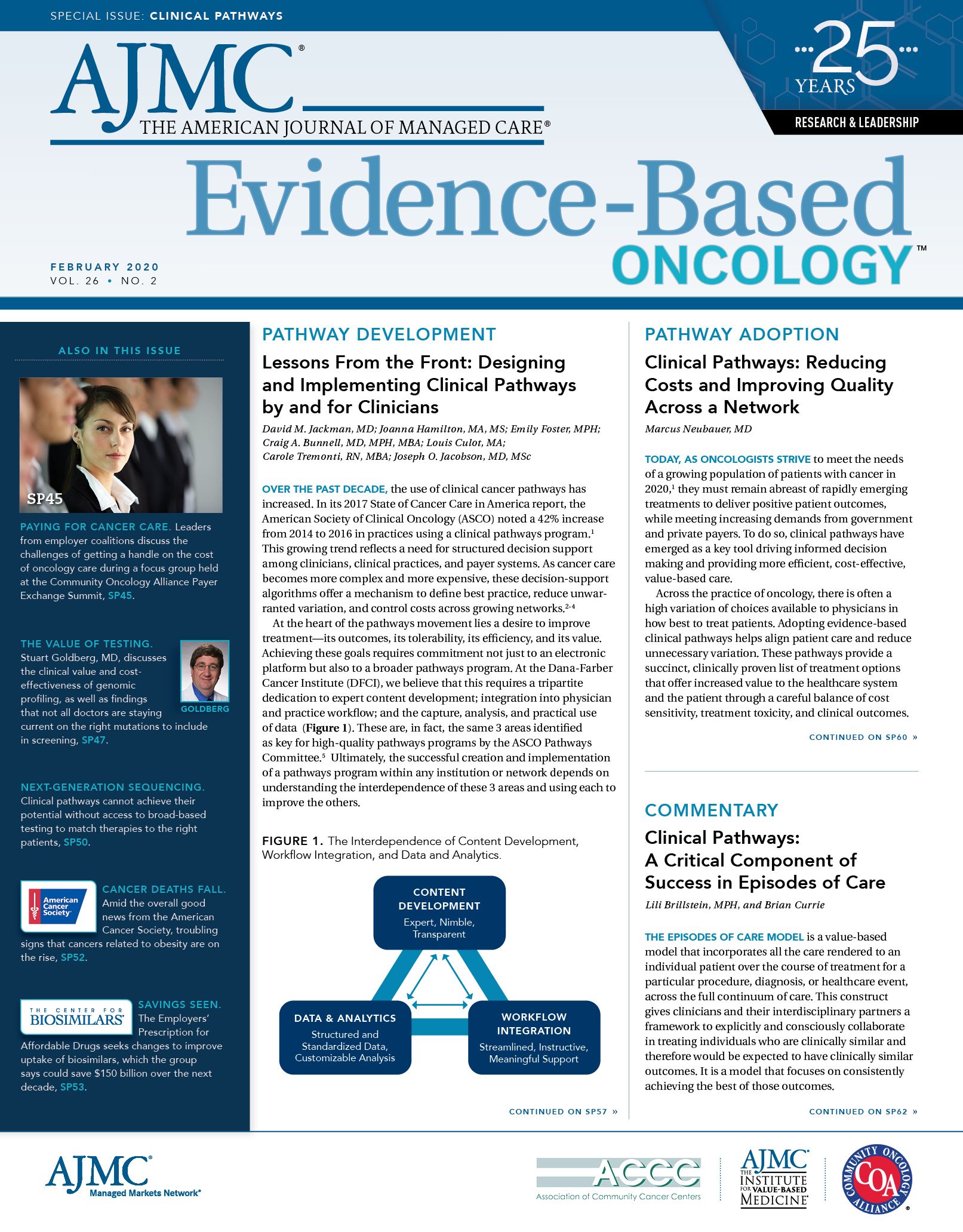
Clinical pathways are the clinical processes and protocols that are designed to guide treatment decision making and ensure that all practitioners care for the individual patient in the most clinically appropriate manner. They are scientifically based best practice standards—that is, the therapeutic interventions with the highest likelihood of achieving the best outcome for the patient. When effectively developed and adhered to, these clinical protocols can help create success within the episodes of care construct and other value-based models.
Employing clinical pathways within a value-based model construct allows clinicians to standardize care to address the variations in care and costs of care among clinically similar individuals; these variations often lead to suboptimal experiences and outcomes and unnecessary costs. Clinical pathways are most often developed by teams of clinicians in the same specialty using big data—years of objective clinical outcomes results on specific diseases—to agree upon the best methods of treating patients with these diseases, while leaving room for individual patient variation.
Pathways alone, however, are insufficient to transform the healthcare industry and create the most efficient treatment models to address a wide spectrum of diseases. It is absolutely critical to identify and understand the variations in care and costs of care to inform and develop the most effective tools. It is healthcare payers, governmental and private, who have the required data and necessary analytical tools to effectively understand those prevailing variations in care.
Truly transforming care requires a close, trusted partnership between payers and providers—it requires an understanding of all the care required for the patient, not just the care rendered by one particular practitioner at a time, as is the focus in the traditional and often frail fee-for-service (FFS) reimbursement model. It requires a commitment to creating and adhering to evidence-based guidelines, as well as a regular review and refinement of those interdisciplinary guidelines, to ensure consistently optimal outcomes.
The FFS model unintentionally creates treatment silos, which do not allow coordination of care between, for example, a primary care physician, an oncologist, a cardiologist, an obstetrician/gynecologist, or another specialty practitioner caring for the same patient with the same condition or multiple chronic conditions. Clearly, this cannot be the path to a future of holistic disease management and treatment. A vexing challenge, however, is that only health plans are the custodians of much of the data that can help provide insights into individual patients’ longitudinal experiences and care. Access to that data has historically been limited, at times inaccurate, and often difficult to discern for providers.
In response to the FFS models’ failure to deliver high-quality care at the most efficient and affordable cost, the alternative, “managed care,” was originally touted as a rigorous, private sector—based approach that could achieve both optimal patient outcomes and more consistent care, as well as help address healthcare costs that were steadily rising to unaffordable levels.
Unfortunately, in practice, the standard FFS model of managed care has in many cases simply devolved into a “Mother may I” activity, in which clinicians must seek permission in advance each time they want to provide an isolated service to an individual patient. The inherent constraints of this model have left health plans intensely involved in the process of approving each isolated aspect of caring for patients, rather than creating networks and clinical models that support providers in making the most effective treatment decisions and collaborating to provide optimal, long-term care for its members. In this environment, health plans have increasingly become managers of increments of quality of care rather than overseers of patient outcomes and experiences and have been only marginally successful in providing support for providers in their role of defining the processes that will lead to the best patient outcomes, both clinically and financially.
The focus in FFS is on each singular, independent service rendered by individual practitioners. Care is often disjointed, with little to no communication among various healthcare providers treating the individual, and individuals are often left to navigate the complex labyrinth of healthcare services on their own. This all has led to unnecessary care, unsustainable costs, and suboptimal outcomes.
The FFS, managed care model of approving increments of treatment has been especially problematic for individuals with chronic and comorbid conditions, as their successful treatment and recovery often depend upon coordinated care among a variety of practitioners.
Episodes of care models provide an opportunity to transcend that dynamic—to use health plans’ own proprietary data to enable them to focus on overall patient outcomes and provide information to providers/clinicians to help them make decisions that create the best outcomes for patients at the most cost-effective price. These models respect the providers as the clinicians in charge of patient care and the health plans as oversight guardians of their members by providing support for those clinicians, as well as tools that ensure that providers and patients can see where unnecessary or unnecessarily costly care is being rendered. Using episodes of care models, the focus of the health plans becomes patient outcomes rather than increments of care. The focus of providers is on the process (that is, clinical decisions) to achieve the best outcomes tied to evidence-based best practices. Clinical pathways are critical tools that providers can use to standardize and achieve those best outcomes.
Episodes of care models have begun to take shape among clinicians caring for individuals with oncologic diagnoses. Evidence-based treatment protocols are widely disseminated and adopted by cross-specialty groups of providers who agree to closely collaborate in their treatment methodologies and evaluate outcomes within the construct of episode of care models. In many cases, surgical, chemotherapeutic, and radiation oncologists not only agree on which specific combinations of treatment are appropriate for an individual patient, based on the type and severity of the disease and its progression, but also adhere to specific time frames regarding the provision of each component of care and the seamless transition of care between and among collaborating providers. Perhaps most importantly for some of these conditions, both the evidence-based protocols and episodes of care models are rapidly being adapted in response to the burgeoning field of targeted biologics and personalized immunologic medicine, which will only exacerbate the need for a combination of evidence-based treatments within the construct of overall value-based treatment models.
Most clinicians believe they are taking the best care of their patients, and of course that is their intent; however, many have no idea that there may be significant variations between the care they deliver and that advocated by experts in their field using the most comprehensive, up-to-date, scientific evidence available. Health plans have the data that can clearly and reliably demonstrate to providers that these variations often can be easily addressed to improve outcomes, patient experience, and overall cost of care.
Physicians are often concerned that engaging in a value-based care model will reduce their ability to make decisions about their patients and about potentially losing their livelihood. If designed collaboratively and reviewed and refined regularly and with utmost respect for the roles of each partner, value-based models should support providers’ decision-making ability and provide additional revenue to those whose outcomes and costs are optimized. These models should also prepare providers to adapt to the rapidly changing advances in clinical treatment of various diseases with the data necessary to manage the soaring costs of such treatment. A value-based partnership model, incorporating evidence-based clinical pathways, would seem to be the only successful path forward to achieve optimal patient outcomes, as well as reduce and eliminate unnecessary costs and burdens to patients and health plans. 
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More

