- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Case Report: COVID-19 Risk in CLL Could Be Exacerbated by Hypogammaglobulinemia
The patient continued to test positive for COVID-19, but intravenous immunoglobulin eventually led to his recovery.
People with chronic lymphocytic leukemia (CLL) are at a higher risk of contracting COVID-19, but a new case report shows that some patients with CLL may experience particularly persistent, worsening cases of COVID-19 as a result of CLL-secondary hypogammaglobulinemia.
The report was published in Cureus.
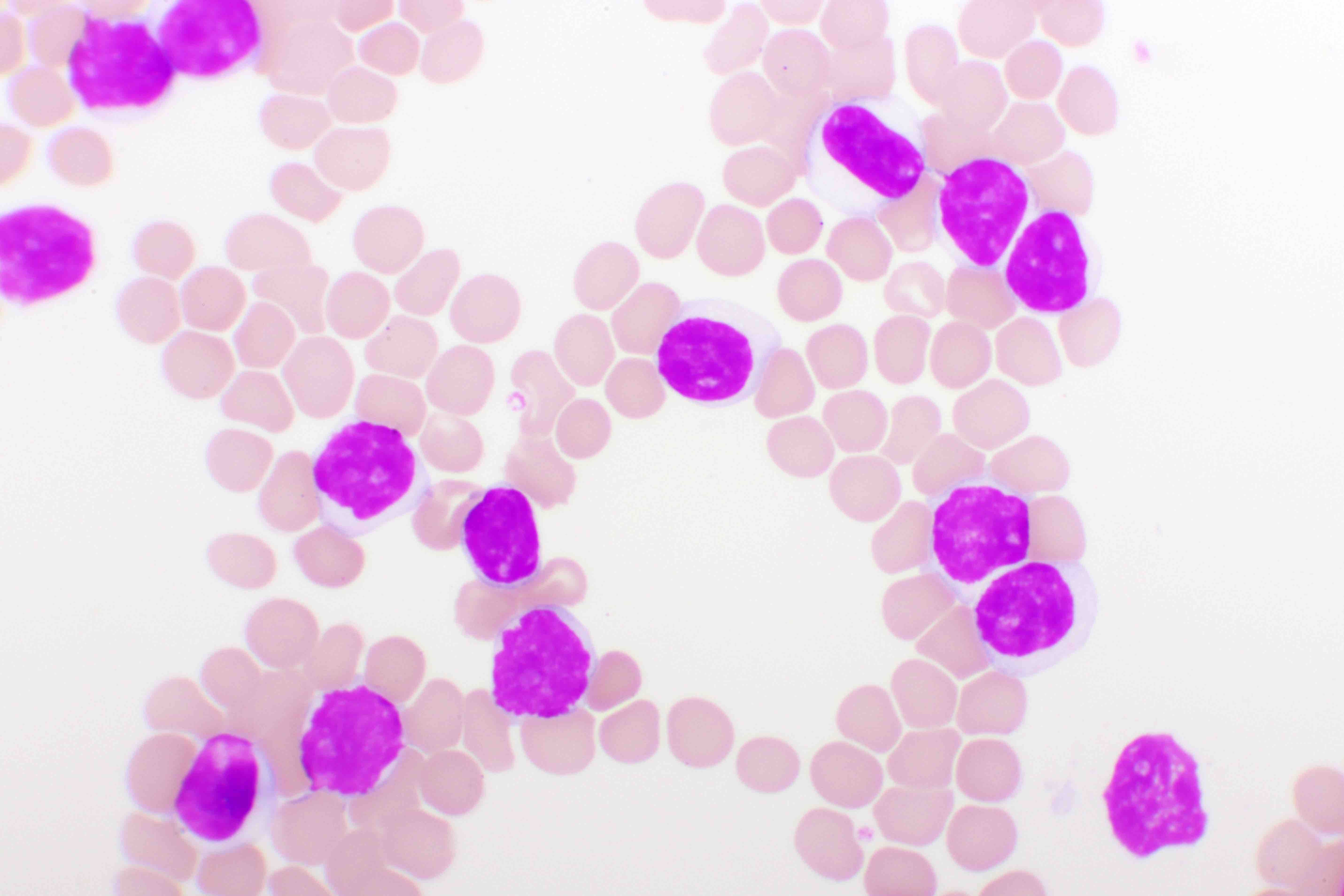
Chronic lymphocytic leukemia | Image Credit: © jarun011 - stock.adobe.com
The case involved a 77-year-old man who received a diagnosis of CLL 13 years ago and whose disease was classified as stage 3 according to the modified Rai clinical staging system. The patient was taking 6 cycles of venetoclax (Venclexta; AbbVie/Genentech) 300 mg daily maintenance.
The patient explained that, despite being fully vaccinated, he had been diagnosed with COVID-19 4 months ago, and since that time he had experienced shortness of breath that got progressively worse. He was treated with antivirals and steroids, but continued to test positive for COVID-19. Two months prior to the visit documented in the case report, he had started requiring oxygen to walk.
“Shortness of breath was associated with a productive cough, and the patient could not walk a few steps without rest,” the authors wrote.
The patient had stable vital signs, and a chest examination showed fine bilateral crackles without lower limb edema or jugular venous distension, according to the authors.
“Initial labs showed normal complete blood count, complete metabolic panel, and brain natriuretic peptide,” they wrote. “Procalcitonin was negative, but C-reactive protein (CRP) was 11 mg/L (normal range: 0-0.8 mg/L).”
A respiratory panel came back negative, with the exception of COVID-19.
The patient was given a CT scan, which showed he had scattered peripheral ground-glass infiltrates that were worse than in previous scans 3 and 4 months prior.
“The patient was again started on [intravenous] steroids and molnupiravir (Lagevrio; Merck) with no improvement in his symptoms over the next few days, so immunoglobulin levels were ordered and showed IgA was 13 mg/dL (normal value: 61-437 mg/dL), IgG 109 mg/dL (normal value: 603-1613 mg/dL), and IgM 15 mg/dL (normal value: 15-143 mg/dL),” the authors reported.
Based on those results, the patient was started on intravenous immunoglobulin (IVIG), which led to immediate improvement following the first dose, they wrote.
After 2 weeks, the patient was no longer requiring oxygen and he reported that shortness of breath was no longer an issue. Additionally, the patient achieved a negative COVID-19 test despite not holding rituximab (Rituxan; Genentech/Biogen) or venetoclax during his treatment.
The authors explained that the patient’s CLL likely affected the course of his COVID-19.
“CLL patients, in particular, have a high risk for a poor outcome from COVID-19 infection, and this can be attributed to co-existing low immunoglobulin levels caused by CLL itself or the treatment regimens which include rituximab,” they noted.
The authors noted that one study found up to 6.6% of patients taking rituximab may develop chronic hypogammaglobulinemia as a result of anti-CD20 medication.
The investigators said they were unable to find in the medical literature a similar case in which a patient continuously tested positive for COVID-19 and had worsening symptoms after being treated with standard therapies. However, they said physicians should keep hypogammaglobulinemia in mind in cases of patients with CLL and COVID-19.
“In conclusion, the use of IVIG, long considered only an ancillary therapy in individuals with CLL on long-term/continuous therapies, must be carefully taken into consideration by physicians who manage these patients with COVID-19 infections, given the longer life expectancy,” they wrote.
Reference
Haddad A, Al-Maharmeh Q, Kloub MN, Ali EA, Shaaban H. Long-lasting SARS-CoV-2 infection with post-COVID-19 chronic interstitial pneumonia in a patient with chronic lymphocytic leukemia treated successfully with intravenous immunoglobulin. Cureus. 2024;16(1):e51890. doi:10.7759/cureus.51890
