- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
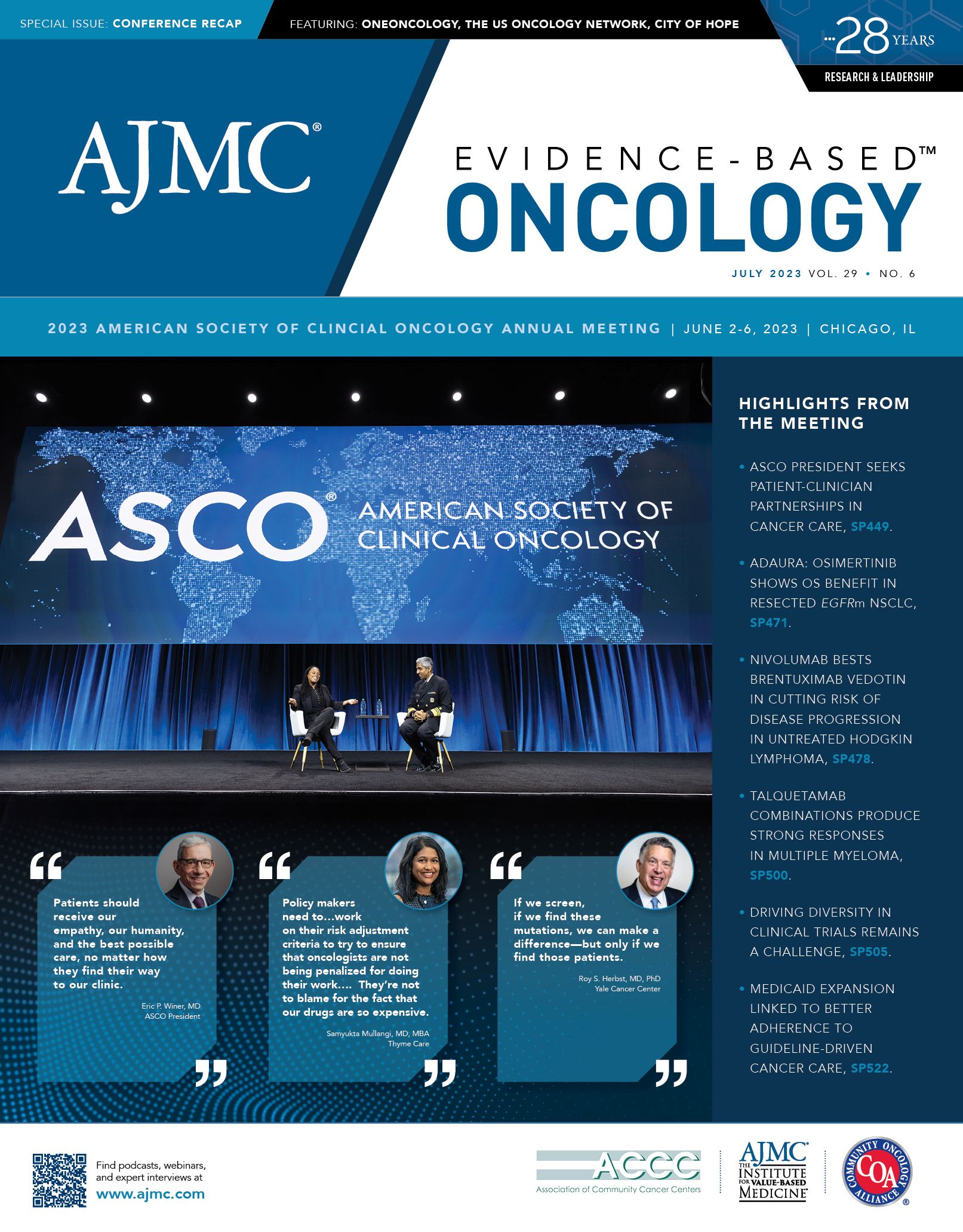
ASCO 2023: Opening Session
Coverage of addresses by ASCO President Eric P. Winer, MD, and National Cancer Institute Director Monica M. Bertagnolli, MD, who is a former ASCO president.
Citing His Own Story, ASCO President Eric P. Winer, MD, Calls for Patient-Clinician Partnerships in Cancer Care
When Eric P. Winer, MD, president of the American Society of Clinical Oncology (ASCO), made patient-clinician partnerships the centerpiece of the 59th annual ASCO meeting in Chicago, he did so from a lifetime of being both the one offering care and the one needing it.
Most of the oncology world will be familiar with Winer’s 35-year career,
Winer

which began when he was chief resident at Yale School of Medicine. His work took him to Duke University School of Medicine and then to Harvard Medical School, where he was a professor of medicine, and Dana-Farber Cancer Institute, where he held the Thompson Chair in Breast Cancer Research and served both as chief clinical development officer and senior vice president for medical affairs.
In February, Winer returned to Yale, where he is the director of Yale Cancer Center and physician-in-chief of Smilow Cancer Network.1
But Winer’s story starts as the patient who has battled chronic conditions since childhood and who brings that perspective to his daily work and his presidential theme, “Partnering with Patients: the Cornerstone of Clinical Care and Research.”
“The theme promotes the preeminence of the relationship between the patient and the oncology clinician, which should be neither hierarchical nor unidirectional,” Winer said. “I believe we must form these partnerships, if we want to provide the very best cancer care and encourage our patients to participate in clinical trials.”
Winer, like his maternal grandfather and 2 great-uncles, was born with hemophilia before effective treatments were available, and he spent much of his childhood hospitalized or in physicians’ offices. “My parents sought out doctors who would partner with them, and quickly moved on to a new physician if their voices were not heard,” he said. “After all, they were the experts in what I was going through.”
Factor VIII concentrates to treat hemophilia became available when Winer was a teenager, dramatically changing his life for the better. “In most ways, I suddenly became a normal kid,” he said.
Years later, those life-altering injections resulted in Winer contracting both HIV and hepatitis C. In 1985, before he had even been diagnosed with either disease, he learned a vivid lesson in medical stigmatization during a visit to the dentist for a root canal.
“As I was lying back in the dental chair, he (the dentist) entered and with barely a greeting asked me to leave the office,” Winer recalled. “He claimed the staff had refused to treat me because of the risk that they thought I posed. I was abruptly denied the access to care that I needed.”
Summarizing the lessons he has learned over a lifetime as a patient and an oncologist, Winer began with the importance of the relationship between doctor and a very ill patient. A healthy patient with no problems may have no relationship with their doctor, but “in the setting of serious illness, those relationships are essential,” Winer said.
He encouraged oncologists to empathize with patients who feel stigmatized by their diagnosis. “Should an individual with lung cancer who has been addicted to tobacco and probably tried to quit repeatedly be treated any differently from a nonsmoker with lung cancer?” he asked rhetorically. “Patients should receive our empathy, our humanity, and the best possible care, no matter how they find their way to our clinic.”
Winer’s own experiences have underscored the importance of research to further medical care in oncology.
“We owe it to our patients to step firmly on the scientific accelerator,” he said. “Basic, translational, clinical, and population-based research have led to life-altering progress and will ultimately allow us to eliminate death and suffering from cancer, assuming we can deliver the best care to everyone. Now, more than ever before, we need to reach out to our own patients, to the patient community at large, and to the general public to understand what we need to prioritize to make their lives better.”
Reflecting on the challenges faced by ASCO and the annual meeting during the past 3 years of the pandemic, Winer applauded the resilience of the organization.
“This year, the total attendance is almost 43,000, and 36,000 of you, or more, are here in Chicago with us,” Winer said. “Almost 7000 abstracts were submitted, which broke the previous high set before the pandemic by 7%. Clearly, the world of cancer investigation is thriving and evolving.”
Reference
Eric P. Winer, MD. Yale Cancer Center. Accessed June 11, 2023. https://www.yalecancercenter.org/profile/eric-winer/
NCI’s Monica M. Bertagnolli, MD: No Excuses to Not Share Data to Reduce Cancer Deaths
Monica M. Bertagnolli, MD, director of the National Cancer Institute (NCI) and nominee to be director of the National Institutes of Health, outlined the challenges to achieving the goals of the National Cancer Plan in her speech accepting the 2023 Allen Lichter Visionary Leader Award at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago.1
Bertagnolli

Bertagnolli, a past president of ASCO, surgeon at Brigham and Women’s Hospital, and member of the Gastrointestinal Cancer Treatment and Sarcoma Centers at Dana-Farber Cancer Institute, was herself diagnosed with breast cancer last year.2 “After getting my own cancer diagnosis last November, I am grateful to be a cancer survivor myself,” she said, praising the nearly half-million women who have volunteered to participate in randomized clinical trials since 1971.
“I am the direct beneficiary of their contributions. And for this, I am profoundly grateful,’’ Bertagnolli said.
The overarching goal of the Cancer Moonshot relaunch announced by President Biden in 2022 is to reduce cancer mortality by half by 2047.3 Achieving that goal will require accelerating the current 2.3% annual decline in cancer death rates to a 2.7% annual decline.
“This might seem relatively easy given the favorable trajectory that we’ve seen in mortality in recent years,” Bertagnolli said. “You all know that it most certainly is not. It will take committed, collective action from all of us, including societal changes much beyond the biomedical community.”
Bertagnolli detailed the 8 goals of the National Cancer Plan that must be achieved to meet the larger goal of cutting cancer deaths by half over the next 2 decades, beginning with preventing cancer in the first place. She noted much of that can be achieved by individuals eschewing cigarettes and embracing a generally healthier lifestyle, but it does not end there.
“We need a fundamental understanding of what drives early carcinogenesis and more accurate management of heritable and environmental risk factors and many more prevention-focused clinical trials,” Bertagnolli said.
Noting that “cancer is a gradual process,” Bertagnolli said cancers that are not prevented must be detected early, and ideally before the disease disrupts the patient’s life. “We must address it before it causes trouble. But we also can’t overreact so that our treatments are worse than the disease,” she said, calling for a better fundamental understanding of cancer biology, new diagnostics, and more clinical trials.
Eliminating inequities in the health care system will be key to reducing cancer mortality. “I don’t believe there is anything more tragic than seeing great harm come to people, not because we don’t have ways to help, but because lifesaving options are just not available to them,” Bertagnolli said.
Many important insights in how to improve oncology care are almost certainly waiting to be encountered in existing data sources but remain undiscovered because of various barriers stemming from both legitimate protections of patient confidentiality and the sheer volume of data. “How much knowledge do we still have locked away in clinical trials’ databases, electronic health records, and in research laboratories?” Bertagnolli asked.
“We no longer have excuses for not sharing data, because technology exists that can allow us to honor the wishes of our patients for data use and to combine, analyze, and visualize data from many different sources. What we still lack is a commitment to this goal.”
Bertagnolli, who has regularly been the first woman appointed to her many leadership posts in the course of her career, stressed the need to “optimize the workforce” that is researching and treating cancer.
“We need to nurture a cancer care and research workforce that is diverse, reflects the communities served, and meets the needs of all people with cancer and those at risk for cancer,” she said.
Less than 10% of cancer patients participate in clinical trials, and increasing that participation will be crucial to improving treatment and reducing death rates, Bertagnolli said, working through a long list of initiatives underway at NCI.
“Every person with cancer or at risk for cancer should have an opportunity, if they wish to do so, to participate in research or otherwise contribute to the collective knowledge base, and barriers to their participation must be eliminated,” she said.
“I am also convinced by my own experience that if we just honor the wishes of people whose data we need in all of these matters, we will make tremendous progress.”
References
1. Tallent A. ASCO honors Dr. Monica M. Bertagnolli for leadership and innovations in cancer care. ASCO Connection. May 16, 2023. Accessed June 12, 2023. https://bit.ly/43VlTox
2. President Biden announces intent to nominate Dr. Monica Bertagnolli as director of the National Institutes of Health. News release. The White House; May 15, 2023. Accessed June 12, 2023. https://bit.ly/3J9Ed5z
3. About the Cancer Moonshot. National Cancer Institute. September 11, 2022. Accessed June 12, 2013. https://bit.ly/46bltwm