- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Young People Disproportionately Represented in Increased Private Insurance Claims for Mental Health Diagnoses, 10-Year Study Finds
Children and young adults under 23 years of age were disproportionately represented in the increase in private insurance claim lines1 with mental health diagnoses from 2007 to 2017, according to a new white paper from FAIR Health, a national, independent, nonprofit organization dedicated to bringing transparency to healthcare costs and health insurance information.
At a time of widespread concern about evidence of a nationwide increase in behavioral health disorders, including both mental health and substance use disorders, FAIR Health drew on data from our database of over 28 billion private healthcare claim records—the largest in the country—to analyze behavioral health trends and patterns in the decade from 2007 to 2017. That period spans the time prior to and after the passage of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008, which required a plan’s coverage for behavioral health treatment to be at parity with its coverage for medical-surgical treatment.
Among our findings:
Claim lines with behavioral health diagnoses increased 108 percent as a percentage of all medical claim lines from 2007 to 2017 (Figure 1).
Figure 1. Claim Lines With Behavioral Health Diagnoses, by Mental Health, Substance Abuse and/or Dependence and Total Behavioral Health, as a Percentage of All Medical Claim Lines, 2007-2017.
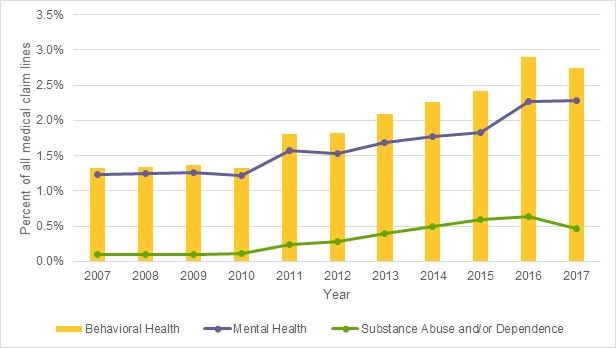
Source: FAIR Health
In keeping with other researchers’ findings that young people are bearing much of the burden of the increase in mental health disorders, FAIR Health found that the pediatric population (defined as ages 0-22, to include people of college age) was disproportionately represented in the increase in claim lines with mental health diagnoses in the period 2007-2017. For example, the pediatric share of claim lines for major depressive disorder increased from 15% to 23% during the study period (Figure 2).
Figure 2. Pediatric and Adult Distribution of Claim Lines with Major Depressive Disorder Diagnoses, 2007 and 2017.
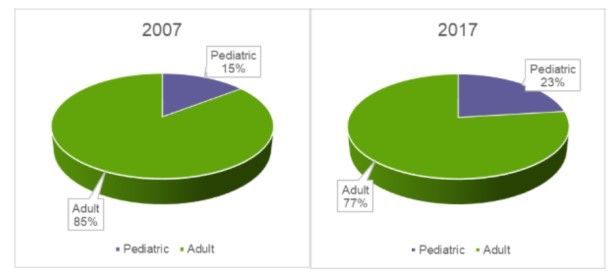
Source: FAIR Health
Claim lines for generalized anxiety disorder rose by greater percentages for individuals of college age (19-22) and high school age (14-18) than for any adult group. For adjustment disorders, claim lines for young adults (ages 19-30, including college-age individuals) increased 78%—more than for any other age group (Figure 3).
Figure 3. Claim Lines with Adjustment Disorder Diagnoses as a Percentage of All Medical Claim Lines by Age Group, 2007-2017.
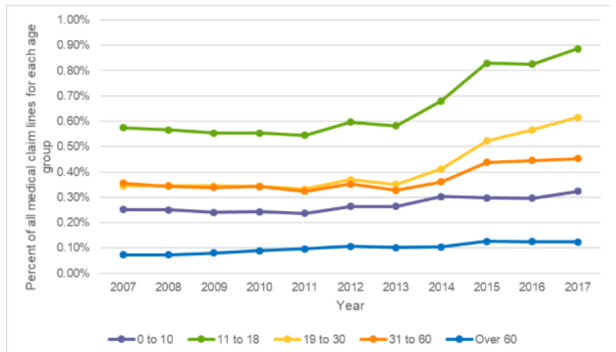
Source: FAIR Health
Opioid dependence claim lines increased 1180% overall from 2007 to 2017—but fell 50% from 2015 to 2017 (Figure 4).
Figure 4. Substance Use Disorders with the Greatest Increases in Claim Lines as a Percentage of All Medical Claim Lines from 2007 to 2017 Despite Decreases from 2015 to 2017: Opioid-Related Only.
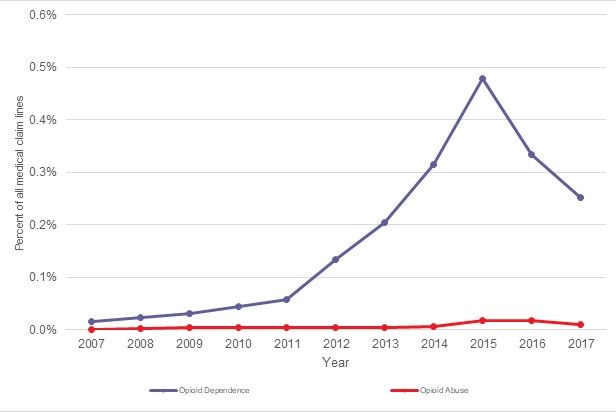
Source: FAIR Health
“Other stimulant dependence” (dependence on stimulants other than cocaine) was the substance use disorder with the greatest increase in claim lines from 2007 to 2017 (3490%), despite constituting a relatively small percentage of all medical claim lines.
From 2007 to 2017, claim lines associated with major depressive disorder and generalized anxiety disorder became more common by comparison to claim lines for all medical diagnoses in most parts of the country—except the South.
At a time of change in the nation’s behavioral health, we are pleased to use our unparalleled data repository to shed light on many aspects of both mental health and substance use disorders. Our study provides a strong foundation of key indicators of behavioral health services among the privately insured. We look forward to further studies that focus on the specific services rendered, the types of venues where patients seek care and the specialties of the healthcare professionals providing the services.
Notes
- A claim line is an individual service or procedure listed on an insurance claim.
Author Information
Robin Gelburd, JD, is the president of FAIR Health, a national, independent, nonprofit organization with the mission of bringing transparency to healthcare costs and health insurance information. FAIR Health possesses the nation’s largest collection of private healthcare claims data, which includes over 28 billion claim records contributed by payors and administrators who insure or process claims for private insurance plans covering more than 150 million individuals. Certified by the Centers for Medicare & Medicaid Services (CMS) as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D; FAIR Health houses data on Medicare Advantage enrollees in its private claims data repository. Ms. Gelburd is a nationally recognized expert on healthcare policy, data and transparency.
