- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
What Recent Evidence Is Telling Us About Alcohol and Cancer
Evidence shows alcohol increases estrogen, raising breast cancer risk, with pandemic-related consumption spikes among women.
The US Surgeon General’s report calling for warning labels linking alcohol with cancer risk may have generated headlines, but for researchers who study these mechanisms, this was hardly news (See Related Article). In December 2020, as alcohol use was rising around the globe during the COVID-19 pandemic, the National Cancer Institute (NCI) convened a workshop and public webinar of experts to evaluate existing evidence and identify gaps in what was known about the connections between alcohol and cancer.1 The group also discussed what can be done to better communicate alcohol’s mortality risks.
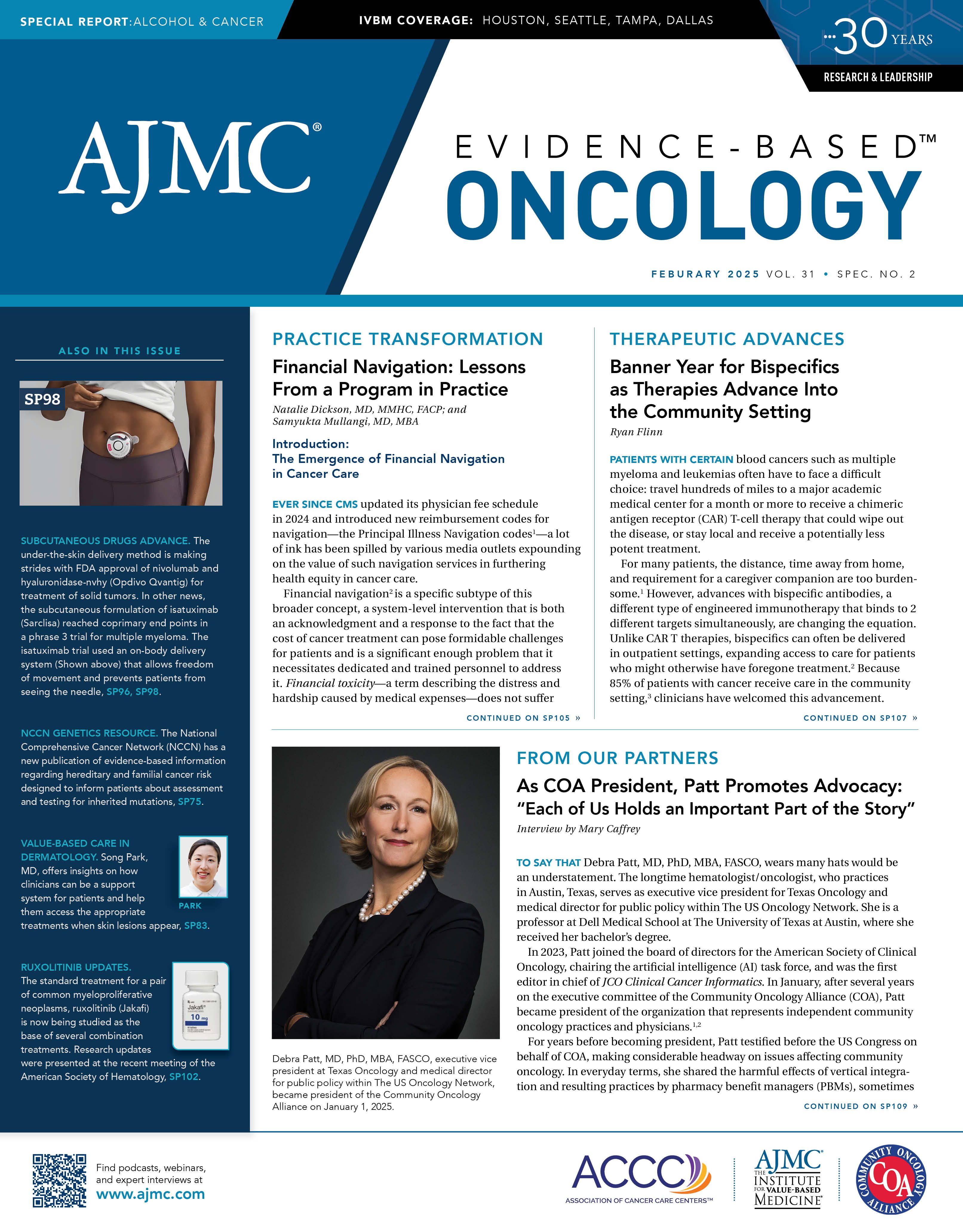
Noelle LoConte, MD | Image credit: University of Wisconsin

One of those experts was Noelle LoConte, MD, a hematologist and medical oncologist at the University of Wisconsin–Madison and lead author of a 2018 statement on alcohol and cancer for the American Society of Clinical Oncology.2 In 2023, LoConte was the senior author of a survey of Wisconsin patients with cancer, which found that increased alcohol consumption during the pandemic was associated with financial hardship and declining mental health.3
Given that evidence about alcohol and cancer has been accumulating for decades, Evidence-Based Oncology (EBO) asked LoConte: What has changed? Here are LoConte’s answers to questions from EBO, edited lightly for clarity:
EBO: What are the most important things we have learned about the mechanisms of how alcohol drives cancer risk? Is there new evidence that has come to light that moved us past a “tipping point” and toward a stronger public education effort?
LoConte: There is some newer evidence that, in my mind, has proven the “abstainer bias” as the cause of the J-shaped curve that, for some time, seemed to favor that 1 drink a day is healthier than not drinking [or drinking more]. The 2023 study4 I am referring to was able to control for people [who] abstained but previously drank vs those who never drank. The abstainers group likely drank enough for that to impact their current health. The never-drinkers, indeed, were the healthiest group.
EBO: We have heard more about increased alcohol use among women. What are the particular issues with how alcohol drives cancer risk in the body that are of special concern to women?
LoConte: The major concern here is breast cancer. Alcohol raises estrogen, which in turn raises the risk of breast cancer. The other issue is that alcohol use among women was shown to increase greatly during and after the pandemic,5,6 which, based on other stressful events that led to communities increasing their alcohol consumption, [such as] 9/11 or Hurricane Katrina, will likely be sustained use.
EBO: The 2020 NCI workshop1 addressed the challenges of communication on alcohol and cancer risk. What do you see as the chief barriers to building public awareness and acceptance that this risk merits action?
LoConte: It’s a nuanced message—it’s some cancers, not all cancers. Some moderate or intermittent use likely is OK. The way alcohol causes cancer is variable, depending on the cancer, etc. That makes pithy or quick messaging hard. The other barrier is that a lot of doctors drink. For example, we know that doctors who are obese are less likely to speak to their patients about obesity, and back in the day, doctors who smoked were less likely to address tobacco use with their patients. Lastly, the alcohol industry is a powerful industry that is opposed to this messaging about alcohol as a carcinogen.
References
1. Gapstur SM, Bandera EV, Jernigan DH, et al. Alcohol and cancer: existing knowledge and evidence gaps across the cancer continuum. Cancer Epidemiol Biomarkers Prev. 2022;31(1):5-10. doi:10.1158/1055-9965.EPI-21-0934
2. LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and cancer: a statement of the American Society of Clinical Oncology. J Clin Oncol. 2018;36(1):83-93. doi:10.1200/JCO.2017.76.1155
3. Lawler T, Anderson SW, Trentham-Dietz A, et al. Change in alcohol consumption during the Covid-19 pandemic and associations with mental health and financial hardship: results from a survey of Wisconsin patients with cancer. J Cancer Surviv. Published November 28, 2023. doi:10.1007/s11764-023-01502-1
4. Zhao J, Stockwell T, Naimi T, Churchill S, Clay J, Sherk A. Association between daily alcohol intake and risk of all-cause mortality: a systematic review and meta-analyses. JAMA Netw Open. 2023;6(3):e236185. doi:10.1001/jamanetworkopen.2023.6185
5. Hahm HC, Hsu KC, Hyun S, Kane K, Liu CH. Psychological distress and heavy alcohol consumption among US young women during the COVID-19 pandemic. Womens Health Issues. 2023;33(1):17-24. doi:10.1016/j.whi.2022.09.002
6. Moskatel LS, Slusky DJG. The impact of COVID-19 on alcohol sales and consumption in the United States: a retrospective, observational analysis. Alcohol. 2023;111:25-31. doi:10.1016/j.alcohol.2023.05.003