- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
VBID and Medicare Advantage: Achieving Bipartisan Support
There has been increased bipartisan support around the expanded role of value-based insurance design.
This article was collaboratively written by A. Mark Fendrick, MD, director of the V-BID Center, and several V-BID Center staff.
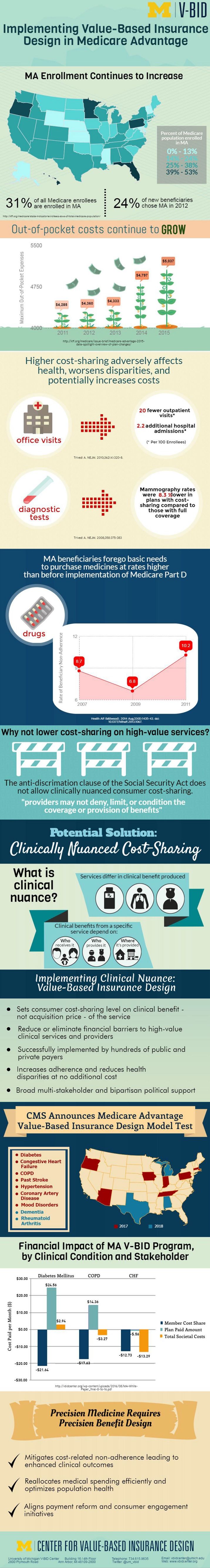
On Thursday, October 27, 2016, the Senate Finance Committee Chronic Care Working Group released a discussion draft outlining bipartisan proposals on how to improve the health outcomes of Medicare beneficiaries living with chronic conditions. One section recommended the expansion of the Medicare Advantage (MA) Value-Based Insurance Design (VBID) demonstration plans to all 50 states.
This increased bipartisan support and expanded role of VBID principles in public and private payers builds on H.R. 5652 “Access to Better Care Act of 2016.” This bipartisan bill provides high-deductible health plans the flexibility to provide coverage for services that manage chronic disease prior to meeting the plan deductible.
This support is based off a growing body of evidence demonstrating that increases in patient cost sharing lead to decreases in the use of both nonessential and essential care. Medicare beneficiaries, many of whom manage multiple chronic conditions, are particularly at risk. Due to misaligned incentives, Medicare beneficiaries receive too much low-value care and too little high-value care.
Applying clinically nuanced VBID strategies presents an enormous opportunity for the Medicare program—particularly MA plans. A review of the peer-reviewed literature reveals how increases in Medicare beneficiary cost-sharing are adversely affecting our most vulnerable beneficiaries, contributing to poor patient-centered outcomes, and, in some instances, increasing Medicare expenditures. Actuarial modeling of MA-VBID programs for diabetes, chronic obstructive pulmonary disease (COPD), and congestive heart failure (CHF) demonstrates that consumer out-of-pocket costs are reduced in all 3 conditions, plan costs increase slightly in the short term for certain conditions (diabetes and COPD), and plan savings result for CHF. From the societal perspective, the diabetes program was close to cost neutral; net savings resulted in the COPD and CHF programs.
VBID can encourage the utilization of high-value providers and services and limit the use of services that are of potentially low-value, thus helping MA plans improve health and quality, enhance consumer engagement, and reduce costs.
To learn more about how VBID can play a role in Medicare Advantage, view the infographic below, and visit the Medicare and MA initiative page.