- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Road to Parenthood After Cancer
Young adult cancer survivors face an uncertain path to parenthood-here is one story.
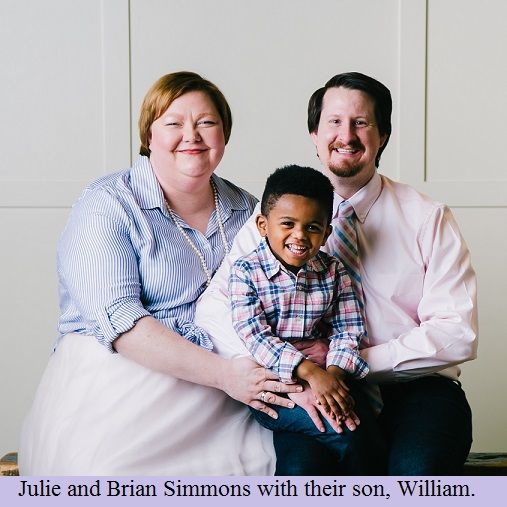
This article has been co-authored by Brian and Julie Simmons, Samfund grant recipients.
The path to parenthood after cancer in young adulthood is different for everyone. But what all young adults have in common is
uncertainty
(whether cancer treatment will affect fertility, and/or whether they can preserve fertility before treatments),
higher
cost
(in vitro fertilization, adoption, surrogacy, and any other way to start a family that doesn’t involve the traditional route carries astronomical costs that are rarely covered by insurance), and a general
lack of guidance
(unfortunately, conversations about family building rarely occur for myriad reasons).
There is a lack of consensus o
n how to treat adolescent and young adult (AYAs) with cancer. Unfortunately, although fertility preservation and family building remain 2 of the issues that are most universal to this age group, they are still not commonly or adequately addressed. Ultimately, it is our hope that sharing stories like Brian and Julie's (below), mine, and others, will raise awareness that,
- This is a common challenge among AYAs
- It is equally important for AYAs to ask questions and for providers to address the issue proactively
- With open communication and sufficient information and guidance, AYAs can feel empowered and hopeful about becoming parents after cancer
Julie and Brian are a Georgia couple who received a Samfund grant to fund their adoption homestudy. They write here about their experience as a couple that faced uncertainty on their way to parenthood due to cancer:
“Can I hold you?” That’s how our toddler frequently greets us in the morning as he sleepily wanders into our bedroom. No matter how the morning is going, when an adorable 3 year-old asks for morning cuddles, the answer is a resounding “YES!” This is especially true when parenthood came after much tribulation.
When we married, we envisioned a future filled with our children’s laughter. There was no question for us—parenthood was part of the ideal. Unfortunately, biology had a different idea. Two years before our wedding, Julie was diagnosed with ovarian cancer. While all cancer diagnoses come with a certain level of fear and dread, reproductive cancers are uniquely hard for a young adult because of the uncertain impact they will have on future fertility and the fact that it’s a topic many don't discuss.
At only 23 years old, our ability to fulfill a lifelong goal of parenthood was in question.
When Julie met with her doctors, fertility wasn’t on her mind. It seemingly wasn’t on her doctors’, either: the first doctor didn’t mention any fertility issues, despite the loss of 1 ovary. The second doctor was the first to say the word “cancer” but didn’t mention fertility. It was only after Julie asked was the topic introduced. The response: “It will depend on the chemo, but we can never know for sure.” The third doctor answered simply: “We don’t know." But what options do you have?
Do you delay treatment and risk the cancer spreading? Do you attempt some sort of preservation in the short window you
might
have? What if you can’t afford it? There are so many unknowns, but all of them are shadowed by CANCER. So, you dive into treatment.
Julie is one of the fortunate cancer survivors. Thanks to treatment by fantastic medical professionals, she survived. However, survival often comes at a price—for Julie, part of that price was impaired fertility. We were cautiously optimistic when we married, hoping for a miracle but expecting a fight. We went through a battery of tests, still to be told that there was no way to know if the chemo had damaged the eggs, or if Julie could even ovulate. They best we heard was that we should try, that it
might
happen.
For years we endured costly, unsuccessful fertility treatments in our attempt to fight against biology. We watched as family and close friends had their first, second, and then third children. In early 2010 we opted for one last-ditch effort before we were to move across the country for graduate school. Painful treatments, daily invasive ultrasounds, signs of hope, devastating losses, and “educated guesses” became routine for us. We had tried everything we could afford, and we were unsuccessful, and broke.
We would need a small nest egg to even think of starting the adoption process. Getting the required home study cost more than we had on hand, so we figured we’d finish school, work for a while until the money was saved, and then start the process of adoption. Then, in late 2011, we felt like we needed to try—that we needed to open the door, fully expecting that we would wait years before a child came to us. With a leap of faith, we submitted a grant request to The Samfund
, a foundation that provides financial assistance to young adult cancer survivors, to cover the cost of an adoption home study. In late 2011 we were notified that our application h
ad been approved. Receiving a Samfund grant forever changed our lives.
Throughout 2012 we worked with an adoption agency to complete the home study and application process. We knew that the process was complicated but we couldn’t anticipate how invasive it would feel. It was like having every nook and cranny of our entire lives laid out before us, and then inviting a panel of strangers to come in and judge us, based on some arbitrary guidelines. There were times we felt like giving up, moments where Julie questioned how this could be worse than chemo, hours of utter despa
ir, thinking it was a fool’s errand and we should grieve the loss and try to move on.
In early 2013 we joined the list of other potential parents waiting to be selected by a birth parent. The agency we used had a sliding scale for fees—the only way we could afford an adoption. The average wait for a placement is more than 3 years, so we settled in for the long haul, but in under a year, our adoption caseworker informed us a birth mother wanted to meet us.
Just 18 days after meeting the birth mother, our son was born. There are not adequate names for the emotions we felt that day. We were sure this beautiful child was meant to be ours. Every day since has been a range of unnamable emotions. One thing is certain, it has always felt right.
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
