- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Expanding the Role of NGS and Retesting in Early and Refractory NSCLC: Jonathan Thompson, MD, MS
Jonathan Thompson, MD, MS, emphasized that broader molecular testing in early-stage non–small cell lung cancer (NSCLC) is essential to guide perioperative treatment decisions, while selective retesting at progression can identify resistance mutations or new targets to optimize value-based care.
At a recent Institute for Value-Based Medicine® event, Jonathan Thompson, MD, MS, a hematology and medical oncology specialist and associate professor at Froedtert and the Medical College of Wisconsin in Milwaukee, emphasized that molecular testing in early-stage non–small cell lung cancer remains inconsistent, despite its importance for guiding perioperative treatment decisions. Next-generation sequencing (NGS) is often underutilized in patients initially considered for surgery, even though identifying actionable alterations—such as EGFR, ALK, or other fusions—should deprioritize immunotherapy, which offers limited benefit in these populations. Thompson noted that current guidelines narrowly recommend testing for EGFR and ALK in early disease, but broader NGS can uncover other drivers, such as ROS1 or MET fusions, that similarly influence treatment choices.
Thompson also addressed payer hesitancy around reimbursement for retesting as disease progresses and new targets emerge. In patients with actionable genomic alterations, repeat NGS at progression can identify resistance mutations such as EGFR C797S or MET amplification, which may open access to novel therapies. Conversely, for patients without driver mutations, repeat broad-panel NGS is less valuable, though biopsy and immunohistochemistry can guide use of antibody-drug conjugates targeting HER2 or MET in the refractory setting. Thompson concluded that expanding guideline-supported testing and aligning payer coverage with evolving molecular insights are critical for ensuring optimal, value-based care.
This is the second part of a 6-part interview series with Thompson.
This transcript was lightly edited; captions were auto-generated.
Transcript
What barriers limit molecular testing in early-stage disease, especially when positive markers may exclude patients from perioperative immunotherapy?
Early stage is a challenge in terms of making sure the biomarkers mentioned are being performed, especially the [NGS]. We see that it's not always routinely performed for patients who are day 1, 2, or 3, who are destined to potentially get surgery, but we do know that patients who either are going to receive neoadjuvant therapy before surgery, or even adjuvant therapy by itself after surgery, that the same principles apply for those patients as they do for our metastatic patients—that we need to know if they have an actionable genomic alteration. If they do, then we need to deprioritize immunotherapy-based treatment in the early stages, because they don't benefit the patient. Alternatively, if they don't have actionable genomic alterations, understanding the PD-L1 level helps us really appropriately select patients who may benefit more from incorporating immunotherapy into their perioperative treatment.
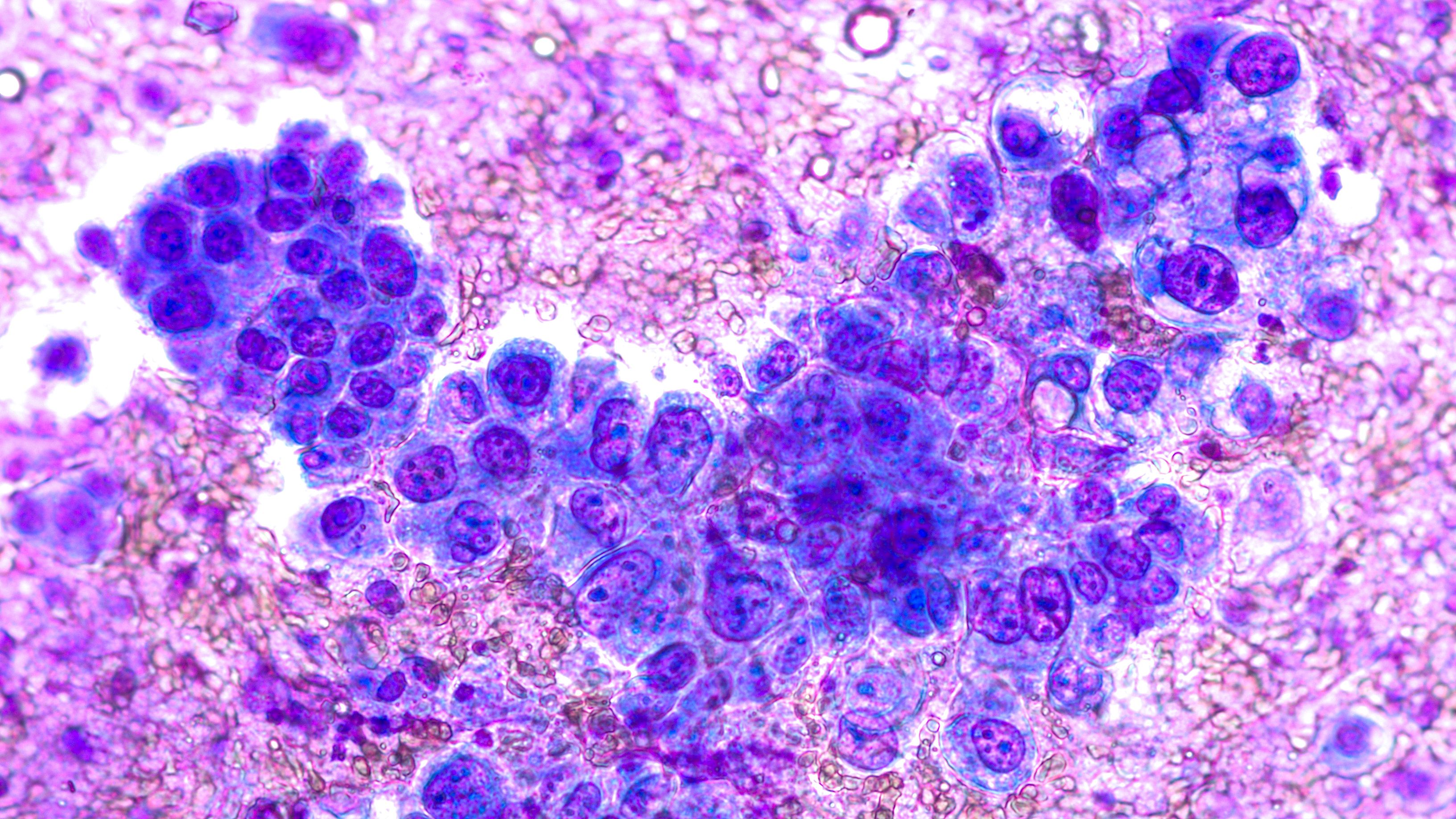
Phogomicrograph of fine needle aspiration cytology of a lung nodule showing non–small cell lung cancer. Image Credit: © David A Litman
Currently, one of the main barriers is some of this molecular testing isn't performed. Some of our guidelines are relatively narrow, meaning a lot of guideline-making organizations only recommend performing EGFR and ALK analysis for early-stage patients, because that's where our FDA approval exists in early stages for EGFR and ALK. However, we also know that other patients with actionable genomic alterations, like the ROS1-MET fusion, these patients similarly don't benefit from immunotherapy-based treatment, just like EGFR and ALK patients don't. Even though it's not in the guidelines right now, we still should be performing [NGS] on these patients to really capture the full breadth of mutation that may inform decision-making.
How can we overcome payer reluctance to reimburse for retesting as new targets and same-class therapies emerge?
Retesting in terms of performing [NGS] on patients who have already had it or reperforming it at the time of progression, I would say, is controversial. There are some patients where it's clearly a benefit, especially patients with our actionable genomic alterations, particularly EGFR—there we know that on progression after EGFR [tyrosine kinase inhibitor], that we certainly do detect genomic alteration if we perform NGS. Things like MET amplification, things like EGFR C797S mutations—detecting these mutations on NGS at the time of progression does potentially open up novel therapies that can get the patient back into disease control, and you wouldn't know about those options unless you repeat the genomic testing.
On the other hand, for patients without actionable genomic alterations, repeating a full NGS panel at the time of progression probably holds less value. It's unlikely to find new mutations that you could act on. There may be a better use of resources to not perform NGS on patients without genomic alteration or actionable genomic alterations. Now we do have increasing access to things like antibody drug conjugates for patients in the relapse/refractory treatment setting. There, we do know that we need to perform immunohistochemistry to detect whether they're potentially eligible for some of these antibody drug conjugate that target things like HER2 or MET. The scenario where I could see performing repeat biopsies or repeat biomarker testing for those without a driver mutation is exactly in that scenario where somebody has progression and we do a biopsy to see if now they have MET overexpression or HER2 overexpression on immunohistochemistry.
