- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The MMRF: Understanding and Sharing the Genomic Landscape of Multiple Myeloma
The MMRF CureCloud Research Initiative, a novel direct-to-patient observational study developed by the Multiple Myeloma Research Foundation (MMRF), collects and aggregates de-identified genomic and clinical data from thousands of patients, providing each participant with a personalized genomic report based on their disease subtype, with the ultimate goal to individualize and optimize their treatment.
In the process, the initiative will create a data set that can inform treatment decisions for all patients with multiple myeloma (MM), according to Anne Quinn Young, MPH, brand president, MMRF. Gathering, aggregating, and sharing the data will lead to “democratization of care,” which is especially important in MM because it disproportionately affects underserved groups, Young said in an interview.
Precision Medicine and Multiple Myeloma
Precision medicine focuses on individualizing treatment by patient and disease state. It is personalized medicine,1 with a goal to protect each patient’s health by considering the factors that influence that individual. It is individualized specialized treatment.
Per the Precision Medicine Initiative, it is “an innovative approach that takes into account individual differences in people’s genes, environments, and lifestyles, giving medical professionals the resources they need to target the specific treatments of the illnesses we encounter.”2
The CDC calls these disease risks “unique,” noting that such an approach can “better predict, prevent, treat, and manage disease.” Methods of doing this include gathering a family disease history, using genomic sequencing, and screening for possible inheritable conditions, such as mutations (eg, BRCA1, BRCA2) or conditions (eg, Lynch syndrome) that predispose some to certain cancers.3
Overall, the process facilitates a more accurate forecast on the success of potential strategies for specialized care, which is in stark contrast to a more generalized approach,4 and when considering contributions from such digital health tools as wearable devices and remote monitoring, the American Medical Association highlights progress in disease prevention and treatment effectiveness.5
In MM—an extremely heterogeneous6 cancer of plasma cells, considered by many to be a chronic condition because it is incurable7-9—the accumulation of abnormal antibodies in the bone marrow interferes with healthy blood cell production, crowding them out and leading to bone pain, mental confusion, and leg weakness/numbness,10 among other symptoms, as well as low levels of several important blood components: white blood cells, red blood cells, and platelets.11
“When I started in myeloma almost a quarter of a century ago, what you have to realize is the treatment back then for patients was still this drug called melphalan, which was developed in the 1960s,” said Daniel Auclair, PhD, chief scientific officer at the MMRF, in an interview with Evidence-Based Oncology™.
The MMRF: From Drug Development to Data Generation
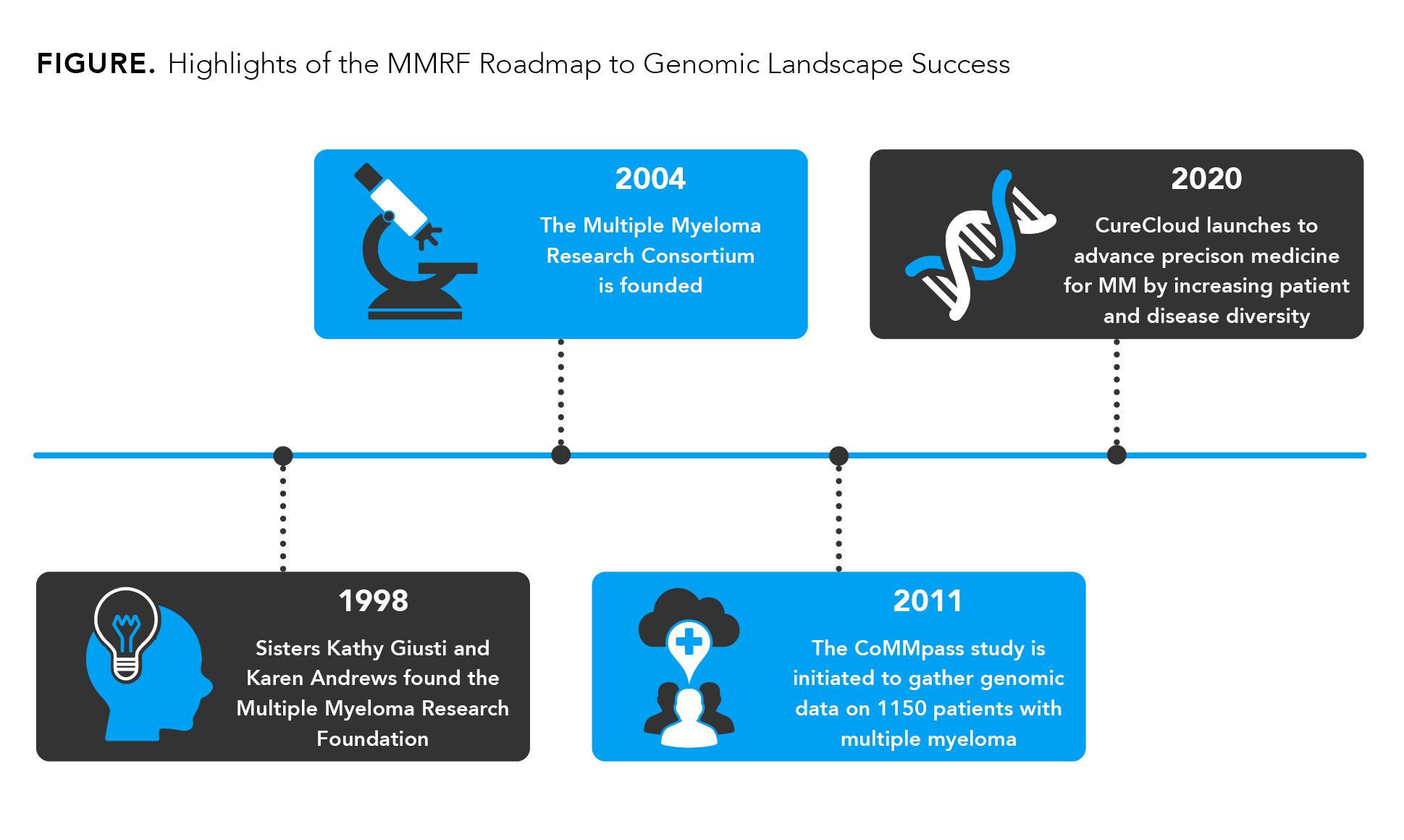
That quarter century ago was 1996, a full 2 years before Kathy Giusti and her twin sister Karen Andrews founded the MMRF, following Giusti’s 1996 MM diagnosis and, soon thereafter, frustration at the lack of effective treatments that could extend a patient’s life beyond the average 3 years between diagnosis and death.12 At first, the MMRF purely funded research grants, including those for novel immune approaches, Auclair stated, “but very early on we realized that in order to make a difference for our patients, we needed to do much more than that. We needed to not only fund some of the research but get intimately involved in the research itself.”
That goal first manifested as the Multiple Myeloma Research Consortium (MMRC), founded in 2004, which has since conducted 89 clinical trials. “Basically, most drugs approved in MM were tested through this clinical consortium,” Auclair said.
While the MMRC was getting off the ground, so, too, was what would become known as The Cancer Genome Atlas (TCGA) at the National Cancer Institute, under the direction of Eric S. Lander, PhD, AB, then at the Broad Institute in Massachusetts. Herculean efforts on the part of TCGA resulted in molecularly characterizing more than 20,000 samples for 33 cancer types over 12 years.13
Noting that 15% of Black individuals at higher risk for MM or with a first-degree relative with a blood cancer who were screened have been found to have a myeloma precursor condition,14 Auclair underscored the importance of early detection and that this could be as simple as a blood test to detect the antibody monoclonal immunoglobulin M protein, “a very beautiful biomarker,” he said, and one that is often used as an indicator of disease extent and possible progression.15 “But we just don’t do it,” he said.
MM was not among the 25 cancers the soon-to-be TCGA had determined to survey. This omission spurred the MMRF to genetically characterize the disease and come up with a long-awaited genomic blueprint by 2009 by incorporating data from several hundred patients who had newly diagnosed or relapsed disease. In total, 6 MM subtypes were identified through those efforts, as were never-before-seen genetic alterations, which helped fuel the MMRF’s efforts to get at the root causes of MM.
The MMRF has since expanded its efforts to defeat MM on several fronts, each of which has incorporated extensive patient data and follow-up, research, and clinical trial work.
In 2011, the CoMMpass Study was initiated, which expanded upon the MMRC’s groundwork by gathering information on close to 1200 patients aged 27 to 93 years—846 from the United States, 172 from Italy, 93 from Spain, and 32 from Canada—from 76 worldwide sites and following up with them on a biannual basis for at least 8 years. With the data it gathered and interpreted through the study, the MMRF has been able to report on what regimens work in what line—from first through fourth—and to what degree, as well as for how long a patient was on a certain combination treatment.16
Patient data have also enabled the MMRF to double its innovative results seen with CoMMpass and identify an astounding 12 subtypes of MM via RNA sequencing. “These subtypes can be related back to DNA alterations, some of which are actionable, meaning there is a therapy available to target and treat that alteration,” the MMRF notes.16
In addition, the CoMMpass findings themselves have given rise to the MMRF’s newest study, MyDRUG (Myeloma - Developing Regimens Using Genomics), which is investigating regimens of drugs—proven effective and already approved to treat other cancers—that specifically target the genetic mutations in each MM subtype.16,17 This study aims to be effective on 2 fronts: hastening the treatment testing process and streamlining the matching of patient to effective regimen.17
“My father always said that there isn’t a coin so thin that it doesn’t have 2 sides to it. There’s the genomic blueprint of the cancer and then there’s how the immune system reacts to it, is influenced by, changes, and responds to treatment,” Auclair added. “When novel immune agents entered the field of myeloma in 2015, we were able to see long remissions; not only responses, but good response and remission. So that told us that immune approaches are the way of the future. That is why we’ve been investing more in this area.”
A Multipronged Approach
CureCloud is that “more,” and through this new initiative launched in July 2020,18 the MMRF is hoping to deploy its CoMMpass findings to the masses—thousands of patients far beyond the 1200 of CoMMpass—with next-generation sequencing (NGS) technology, starting with direct outreach to a potential 5000 patients that it hopes results in treatments for all of them.19
Thinking outside the box through CureCloud—yet building on knowledge gained through CoMMpass—the MMRF is using a multipronged approach to advance precision medicine for patients by consolidating all of the information in one place that they can access with their physicians to inform treatment decisions. For patients, this involves enabling consent online (smartphones can be used), including the release of their medical record, which brings a phlebotomist to their home for a liquid biopsy blood draw, which in turn leads to a personalized genomic report containing information on their variation of MM along with clinical trials focused on their subtype. Clinicians approve each patient’s free liquid biopsy orders and review the personalized genomic report with them to determine the optimal course of action, adding to their MM treatment knowledge with each new participant in CureCloud19,20 and by making that data available to all patients and doctors.
Genetic sequencing of those blood samples comes next, through the use of an NGS assay that looks at the 70 most relevant genes in MM, Auclair said, by capturing the DNA that MM cells release into the blood through apoptosis. Molecular pathologists look over these sequencing reports and approve the findings before passing them on to the treating clinicians and the patients, the latter of whom receive a report they can more readily understand.
“We felt very strongly that for all the patients have given, for all their altruism, we wanted to give something actionable back,” Young said in an interview with Evidence-Based Oncology™. “The exciting technology allowed us to work toward democratization of care, which is especially important in a disease like multiple myeloma, which disproportionately affects traditionally underserved populations.”
For example, Black Americans receive a diagnosis of MM at twice the rate of White Americans and are younger when they receive that diagnosis,21-23 and per 100,000 individuals, non-Hispanic Whites have been shown to have a higher incidence rate than Asian and Hispanics outpace Whites.21 In addition, older Americans tend to shoulder a disproportionate burden of MM diagnoses, with the median age of diagnosis ranging from late 60s to early 70s.22,24-26
Figure. Highlights of the MMRF Roadmap to Genomic Landscape Success
Bringing Greater Diversity to Enrollment
Speaking to how CureCloud aims to balance patient diversity and disease diversity, Young told of how past MMRF work keeps paying it forward. Those working on CureCloud have consulted with the MMRC and CoMMpass sites that have found success at enrolling diverse patient populations in their studies for help in devising plans to ensure at least 20% of CureCloud patients are Black.
“We asked them, ‘How can you help us make sure that we do the same with CureCloud, that 20% of the 5000 patients are Black?’—because 20% of myeloma patients are Black,” she said. “We’re also working with health systems,” she noted, one of which is Ochsner, for whom over 40% of their patients with myeloma are Black.
The outreach doesn’t stop there, however. In fact, it is constantly evolving, and the MMRF continues to evaluate its efforts by looking at the data that come in to see where refinement is needed—to uncover goals that are not being met and to come up with new strategies to ensure they are.
Young also shone a spotlight on 4 of the sites that are MMRC participants—Winship Cancer Institute at Emory University/Medical Center in Atlanta, Georgia; Icahn School of Medicine at Mount Sinai in New York City; Karmanos Cancer Center at Wayne State University in Detroit, Michigan; and Siteman Cancer Center at Washington University in St. Louis—noting their good relationships with their surrounding communities foster collaboration.
“CureCloud helped us better understand where we were falling short in reaching patients directly,” she emphasized. “That made us decide to supplement the marketing we were already doing to our patient database with consulting with those sites that have already been successful at patient engagement with more diverse or underserved communities.”
“We have drugs approved in MM that have not been extensively tested in certain populations. Some drugs that were approved in myeloma didn’t even have 1% of African American participants in the registrational studies,” Auclair added. “We’ve learned that we need to reach them where they are, because direct-to-patient contact doesn’t always work for underserved communities.”
Especially if patients aren’t able to be seen at some of the biggest centers, where sequencing is more common, the report they get from CureCloud could open up treatment options “they didn’t know about before,” Young continued.
“There are different ways to do research, there are different ways to do science, and efforts direct to patients, like CureCloud, using a lot of technology, a lot of telemedicine, are truly the future for our patients,” Auclair said.
Even with the extensive knowledge that has been gained through the MMRC, CoMMpass, and now CureCloud—along with the treasure trove of genomic data gained—there are still gaps in the precision space for MM because of the heterogeneous nature of this chronic disease. A cure remains out of reach, at least for now.
Although the trials the MMRF has conducted though the MMRC and its partners have led to an average overall survival of 5 to 7 years following an MM diagnosis for approximately 75% of patients, with transplant and standard-of-care treatment—and to a median overall survival of 9 to 10 years in 25% of patients—the majority do not reach the 3-year mark after treatment initiation because of disease relapse while on treatment, the MMRF experts said. Three areas in this regard that continue to benefit from the ongoing research conducted by the MMRC are early-stage disease, prevention of upfront/high-risk disease, and relapsed/refractory disease.
“We’re addressing each of these groups with potentially transformative agents,” Young pointed out. “We’re not here to do trials that are just for publication; we are here to make a difference in those populations, to extend progression-free survival and, ultimately, extend survival.”
A Resource for All Cancers
When asked if they are already thinking beyond CureCloud, not just for MM but for how the MMRF’s efforts could expand to push progress in other hematological disorders, Auclair and Young emphasized how the MMRF’s collective efforts aim to open a path to precision medicine, not just for all blood cancers but for all cancers in clinical immune genomic precision medicine.
Ultimately, a cure will only come from this kind of precision medicine approach, they said, with the next frontier in MM being to intercept the disease early—so patients don’t have to face worse outcomes from an advanced-stage diagnosis—by combining real-world data collection and 21st-century technology, by translating research efforts to the clinic, and by making a difference with actionable information from the patients themselves.
“The best way, ultimately, to defeat the disease, to stop cancer, will be to identify it early, identify the individuals early, and for those at higher risk, follow them very closely,” Young and Auclair underscored. “We need to intercept the disease.”
References
1. Precision medicine. National Cancer Institute. Accessed August 5, 2021. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/precision-medicine
2. The Precision Medicine Initiative. The White House. Accessed August 5, 2021. https://obamawhitehouse.archives.gov/precision-medicine
3. CDC. Precision health: improving health for each of us and all of us. Accessed August 5, 2021. https://www.cdc.gov/genomics/about/precision_med.htm
4. What is precision medicine? MedlinePlus. Updated September 22, 2020. Accessed August 10, 2021. https://medlineplus.gov/genetics/understanding/precisionmedicine/definition/
5. Precision medicine. American Medical Association. Accessed August 10, 2021. https://www.ama-assn.org/delivering-care/precision-medicine/precision-medicine
6. Rasche L, Kortüm KM, Raab MS, Weinhold N. The impact of tumor heterogeneity on diagnostics and novel therapeutic strategies in multiple myeloma. Int J Mol Sci. Published online March 12, 2019. doi:10.3390/ijms20051248
7. How long can I live with multiple myeloma? Roswell Park. March 26, 2021. Accessed August 10, 2021. https://www.roswellpark.org/cancertalk/202103/how-long-can-i-live-multiple-myeloma
8. Osterwell N. Multiple myeloma: from palliative care to chronic therapy? MedPage Today. April 11, 2016. Accessed August 10, 2021. https://www.medpagetoday.com/reading-room/asco/multiple-myeloma/57193
9. Millar H. Inching toward a cure for multiple myeloma. Cure®. October 6, 2015. Accessed August 10, 2021. https://www.curetoday.com/view/inching-toward-a-cure-for-multiple-myeloma
10. Mayo Clinic staff. Multiple myeloma. Mayo Clinic. Accessed August 10, 2021. https://www.mayoclinic.org/diseases-conditions/multiple-myeloma/symptoms-causes/syc-20353378
11. What is multiple myeloma? American Cancer Society. Updated February 28, 2018. Accessed August 10, 2021. https://www.cancer.org/cancer/multiple-myeloma/about/what-is-multiple-myeloma.html
12. About the MMRF. Multiple Myeloma Research Foundation. Accessed September 7, 2021. https://themmrf.org/about/
13. The Cancer Genome Atlas Program. National Cancer Institute. Accessed September 7, 2021. https://www.cancer.gov/about-nci/organization/ccg/research/structural-genomics/tcga
14. Predicting Progression of Developing Myeloma in a High-Risk Screened Population (PROMISE). Clinicaltrials.gov. Updated June 23, 2021. Accessed September 9, 2021. https://clinicaltrials.gov/ct2/show/NCT03689595
15. Multiple myeloma: diagnosis. Cancer.net. Accessed September 9, 2021. https://bit.ly/38REpUr
16. The MMRF CoMMpass Study. Multiple Myeloma Research Foundation. Accessed September 9, 2021. https://themmrf.org/finding-a-cure/our-work/the-mmrf-commpass-study/
17. What is the MyDRUG study? Multiple Myeloma Research Foundation. Accessed September 9, 2021. https://themmrf.org/finding-a-cure/our-work/my-drug/
18. MMRF CureCloud Research Initiative. Clinicaltrials.gov. Updated July 27, 2020. Accessed September 13, 2021. https://clinicaltrials.gov/ct2/show/NCT03657251
19. What is the MMRF CureCloud? Multiple Myeloma Research Foundation. Accessed September 13, 2021. https://themmrf.org/finding-a-cure/our-work/the-mmrf-curecloud/
20. CureCloud. Multiple Myeloma Research Foundation. Accessed September 13, 2021. https://mmrfcurecloud.org/
21. Marinac CR, Ghobrial IM, Birmann BM, Soiffer J, Rebbeck TR. Dissecting racial disparities in multiple myeloma. Blood Cancer J. Published online February 17, 2020. doi:10.1038/s41408-020-0284-7
22. Waxman AJ, Mink PJ, Devesa SS, et al. Racial disparities in incidence and outcome in multiple myeloma: a population-based study. Blood. 2010;116(25):5501-5506. doi:10.1182/blood-2010-07-298760
23. Kazandjian D. Multiple myeloma epidemiology and survival: a unique malignancy. Semin Oncol. 2016;43(6):676-681. doi:10.1053/j.seminoncol.2016.11.004
24. Turesson I, Velez R, Kristinsson SY, Landgren O. Patterns of multiple myeloma during the past 5 decades: stable incidence rates for all age groups in the population but rapidly changing age distribution in the clinic. Mayo Clin Proc. 2010;85(3):225-230. doi:10.4065/mcp.2009.0426
25. Multiple myeloma: risk factors. Cancer.net. August 2021. Accessed September 27, 2021. https://www.cancer.net/cancer-types/multiple-myeloma/risk-factors
26. Rajkumar SV, Kumar S. Multiple myeloma: diagnosis and treatment. Mayo Clin Proc. 2016;91(1):101-119. doi:10.1016/j.mayocp.2015.11.007
Early Data Show Promising Outcomes as CAR T-Cell Therapy Expands Beyond Academic Centers
January 12th 2026Abstracts presented at ASH 2025 explore CAR T-cell therapy's effectiveness in newly authorized treatment centers, revealing promising outcomes for multiple myeloma patients and the prospect of expanded access.
Read More
