- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Impact of Reinsurance of Gene Therapies on Employer Financial Risk
The explosion of innovation in health care comes with a price tag. While the cost of an individual product or service may be small in the scheme of national health expenditures, a single event can be financially devastating to a self-insured plan sponsor. This is especially true for the growing proportion of smaller employers that assume the financial risk for providing health care benefits to their employees.
Between 2013 and 2017, rising insurance premiums and administrative costs, coupled with the coverage mandates of the Affordable Care Act (ACA), drove nearly a quarter of midsized (100-499 employees) and smaller (<100 employees) employers out of the traditional (or fully funded) insurance market and into self-insured (or self-funded) arrangements. By 2017, 31% of midsized and 16% of smaller employers offered a self-funded health plan.1 For employers that have decided to go it alone, claims payouts and the risk of unanticipated losses rise in step with the cost of innovation.
Self-funded plans, authorized by the Early Retirement Income Security Act (ERISA), come in 2 varieties. In a totally self-funded plan, the employer is responsible for all insurable risk and pays claims through a third-party administrator. Totally self-funded plans are rare because of the risk of catastrophic claims. In partially self-funded plans, the employer uses a stop-loss carrier to limit claims exposure. This is called stop-loss coverage (not to be confused with reinsurance, in which a secondary reinsurer provides protection for stop-loss carriers.)
The potential for million- and multimillion-dollar treatments over the coming decade has raised new questions about the purpose of stop loss coverage. As employers and third-party carriers wrestle with these questions, patients’ need for access to lifesaving innovation remains critical. Manufacturers whose products are at the center of this issue can help to lead a constructive discussion.
Anatomy of Stop Loss
Stop-loss coverage shields self-insured employers from individual catastrophic claims as well as overall exposure. In exchange for an annual premium, the stop-loss carrier provides the employer with protection against shock claims (high-dollar, low-frequency events like sepsis), as well as outlier cost spikes arising from cancer care, premature births, organ transplants, and other resource-intensive health events. Increasingly, complicated cases involving a single high-cost drug, such as those for hemophilia, are becoming an area of concern.
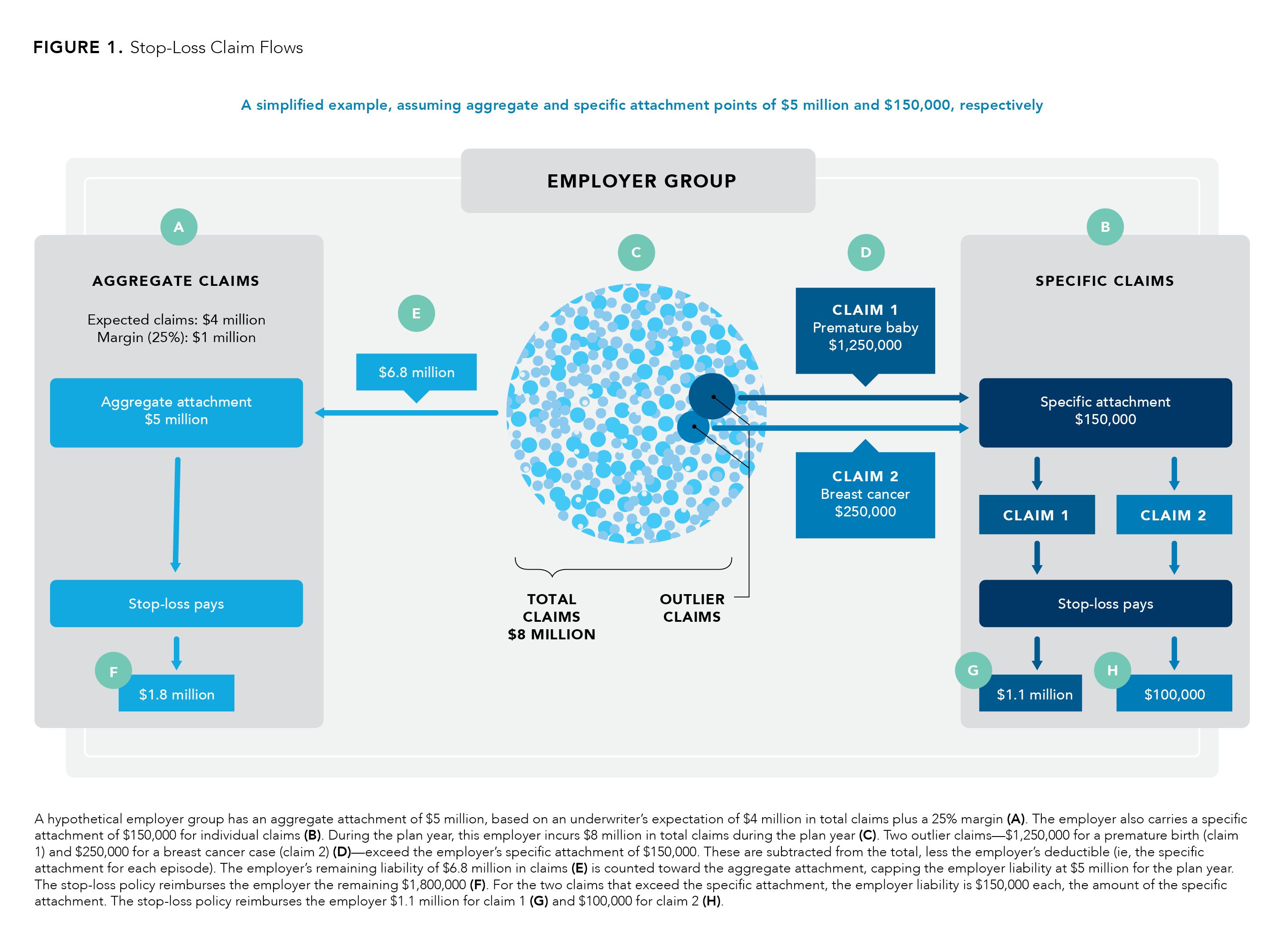
Stop-loss policies usually contain 2 components: specific and aggregate coverage2:
- Specific coverage protects against claim severity for a single individual. An attachment point—essentially, an individual deductible for each member of the plan that an employer must cover before a stop-loss claim is paid—defines a dollar limit on the employer’s liability for any single individual during the plan year. Any excess costs become the responsibility of the stop-loss carrier.
- Aggregate coverage provides protection against the cumulative impact of smaller claims. When an employer’s total claims payments reach an aggregate attachment point, often calculated monthly, the stop-loss provider picks up all remaining costs up to the limit of the policy. Stop-loss claims paid are not included in the aggregate attachment point.
Stop-loss pricing is a complicated affair. Attachment points determine the level of risk an employer is willing to absorb and are priced on an actuary’s determination of the group’s expected losses. Policies are subject to underwriting on an annual basis. At renewal, carriers evaluate current claims data to determine whether this year’s attachment points represent a reasonable risk for the price. However, the smaller the group, the less reliable its experience for pricing purposes.2
An individual with unusually high expenses may be carved out or excluded from the plan the following year, leaving the employer to pay all claims on that individual. Alternatively, a carrier may offer a laser —a higher specific attachment point—for a beneficiary known to have a high-cost condition and whom underwriters believe is likely to breach the deductible in the coming plan year. Rather than raise the premium, the carrier adjusts the threshold for that single claimant. In some cases, a laser may be required as a condition of any coverage.2
A laser may be many multiples of the specific attachment point. As an example, an employee undergoing cancer treatment may be lasered at $500,000, whereas the remainder of the employer’s population carries a $150,000 specific attachment point. The deductible for the employee who is lasered will be similar to what the underwriter believes the cost of her treatment will be.3 Cancer is a common condition for lasers; others are kidney failure, severe injuries, and conditions that may ultimately require an organ transplant.4
Aggregate attachment points are determined by estimating total claims expected and then adding a risk corridor—a margin of anywhere from 10% to 25% of expected claims—to account for medical inflation, fluctuations in the size of the employer’s workforce, or other unexpected circumstances.2,3 If, for instance, the underwriter expects total claims (not including those that exceed the specific deductible) to reach $4 million and the stop-loss carrier adds a 25% risk corridor, then the employer’s aggregate liability will $5 million (Figure). It is rare for an employer to hit this, as it would involve a very high percent of employees hitting these limits in 1 year.
Figure.
Market Trends and Dilemmas
Once the domain of large employers, self-insurance has become popular with smaller companies that seek to control expenses. In the past, the rule of thumb was that once a company offered health benefits to more than 250 beneficiaries, a transition from fully insured to self-insured status made sense. The savings on premiums, taxes, and insurers’ reserves and administrative costs outweighed the cost of claims payments, assuming the employer also had help from a stop-loss carrier with outliers.5
But today, groups as small as 100 beneficiaries are self-insuring. Why?
The ACA helped accelerate this shift. The law included new coverage mandates and administrative costs, and it required qualified health plans to cover 10 categories of essential health benefits (EHB), some of which were less essential to some employers than others. Self-insured employers are exempt from the EHB clause. Moreover, in a self-insured arrangement, the employer has access to its own claims history, which allows management to make more informed decisions about plan design.6
But where the ACA created incentives for small employers to migrate away from fully insured plans, it also created trapdoors for them to mind along the journey. The health care reform law removed annual and lifetime limits on benefits, making catastrophic claims a much greater risk for self-insured groups, especially smaller ones. For an employer with 100 covered lives, a single million-dollar claim could be greater than the sum of all other claims in a given year.7
One insurance carrier saw its number of annual claims that exceeded $1 million rise by 68% between 2013 (the year before ACA protections were implemented) and 2016, according to the Massachusetts Institute of Technology’s Center for BioMedical Innovation. The center estimates the incidence of such claimants today at 1 per 10,000 to 15,000 covered lives each year.7
With benefit limits lifted, claims in excess of $1 million were no longer rare. Stop-loss coverage became essential not only for smaller employers, but also for larger employers that once might have been able to absorb 1 or 2 million-dollar claims but now struggle with 10 or 20.8
That brings us back to innovation. Potentially curative therapies have reached the market today, and as many as 50 cell and gene therapies could receive Food and Drug Administration approval by 2030.9 Although many are for limited populations, they nonetheless contribute to the frequency of high-dollar claims. Tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta), chimeric antigen receptor (CAR) T-cell therapies for blood cancers, debuted in 2017 at list prices of $475,000 and $373,000 each for a course of treatment.10
And those don’t even make the top 10 list in terms of cost (Table). Two gene therapies, onasemnogene abeparvovec (Zolgensma) and voretigene neparvovec (Luxturna), developed respectively for a rare muscular disorder and a form of blindness, rank first and third. Zolgensma will set a plan sponsor back $2.1 million; Luxturna, $850,000.11
Table.
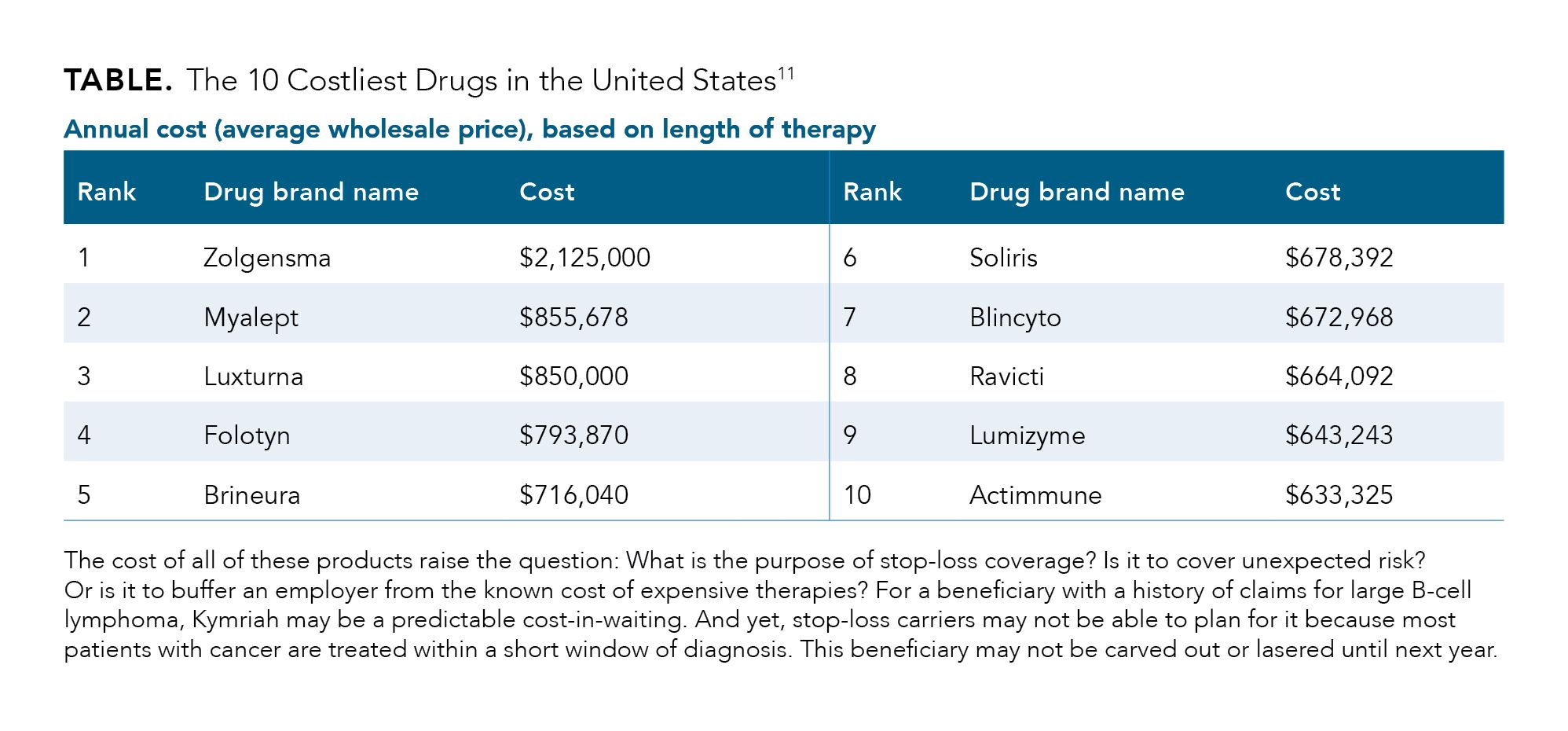
The costs of all of these products raise the question: What is the purpose of stop-loss coverage? Is it to cover unexpected risk? Or is it to buffer an employer from the known cost of expensive therapies? For a beneficiary with a history of claims for large B-cell lymphoma, tisagenlecleucel may well be a predictable cost-in-waiting. And yet, reinsurers may not be able to plan for it because most patients with cancer are treated within a short window of diagnosis. This beneficiary may not be carved out or lasered until next year.
Stop-loss Providers Respond
In the long term, answers to questions like those above will influence how those who write stop-loss policies will approach costly new innovations. For the short term, however, many are already taking steps to limit their own exposure. At their core, each of the following short-term responses to market trends is a variation on the same concern: as high-cost innovations serve an ever-greater number of people, stop-loss coverage becomes more expensive and includes more qualifications and lasers.
HIGH-COST AND HIGH-RISK PATIENTS. As stop-loss contracts are subject to underwriting on an annual basis, carriers begin to review medical and prescription drug claims data a few months before a policy will renew. The purpose of this exercise is to identify individual claimants with a high likelihood of breaching the specific deductible during the next plan year.
To avoid unwelcome coverage surprises in the next or subsequent years, employers will need data mining and analytics capabilities that enable them to take a population health management approach. This means identifying those in their workforces who are not only at high risk now but also those who may be thought of as rising risk.
LASERS. Beneficiaries with a history of claims for a high-cost therapy, injectable drug, or other service have long been at risk for being lasered. Now, as the cost of innovation soars to new heights, even people with a higher-than-average predisposition for a costly illness may be candidates for lasers. Because a laser can be a sweeping liability to plan assets, a self-insured employer typically can absorb only 1 or 2 such cases.
Employers should work with their third-party administrators to understand their stop-loss carriers’ own appetite for risk and whether the carrier is sensitive to a particular diagnosis, therapy, or dollar threshold. This may help the employer to identify individuals who are at risk of being lasered and proactively evaluate their eligibility for patient assistance programs on a regular basis.
EXCEPTIONS. If the stop-loss carrier does not offer a laser on a high-cost beneficiary, it may choose 1 of several actuarial options: build a high-cost treatment into premiums, increase the cost threshold (ie, the specific attachment) for each beneficiary—or, perhaps a worst-case scenario for the employer, exclude the individual from coverage altogether.
While the ACA guarantees coverage for people with pre-existing conditions in ERISA plans, this protection is not incumbent on stop-loss carriers that back a self-funded plan.
Patient exclusions drive up the cost of claims in ERISA plans. The cumulative effect of exclusions may force employers to move back into the fully insured market, where services are more tightly managed and where they have less control over costs and less transparency of claims.
SECONDARY REINSURERS. Yes, stop-loss carriers themselves purchase reinsurance. It is not uncommon for carriers to transfer individual-claim risk (anywhere from $1 million for a smaller carrier to $5 million or more for a larger one) to a secondary reinsurer in exchange for a per-person, per-month premium. When this happens, a portion of an employer’s premium for stop-loss coverage becomes a pass-through expense to the employer.12
Because of the increasing severity and frequency of high-cost drug claims, secondary reinsurers are beginning to exit the market. Stop-loss carriers are a safety valve for self-insured employers (and for traditional payers as well), and secondary reinsurers are their safety valve. As each valve closes, pushing risk back toward the payer, the cost of self-insuring grows, forcing the employer to consider alternatives to its current strategies for managing risk.
MONITORING PIPELINES. Stop-loss carriers follow manufacturers’ pipelines to identify potential new treatments, especially innovations likely to be high cost. These potential treatments are matched to individuals within the employer’s population whose medical and claims histories suggest they may be candidates for it. The stop-loss carrier’s underwriters may, in turn, set qualifications for these beneficiaries, although at times there may be no way to tell if treatment will happen in the plan year.
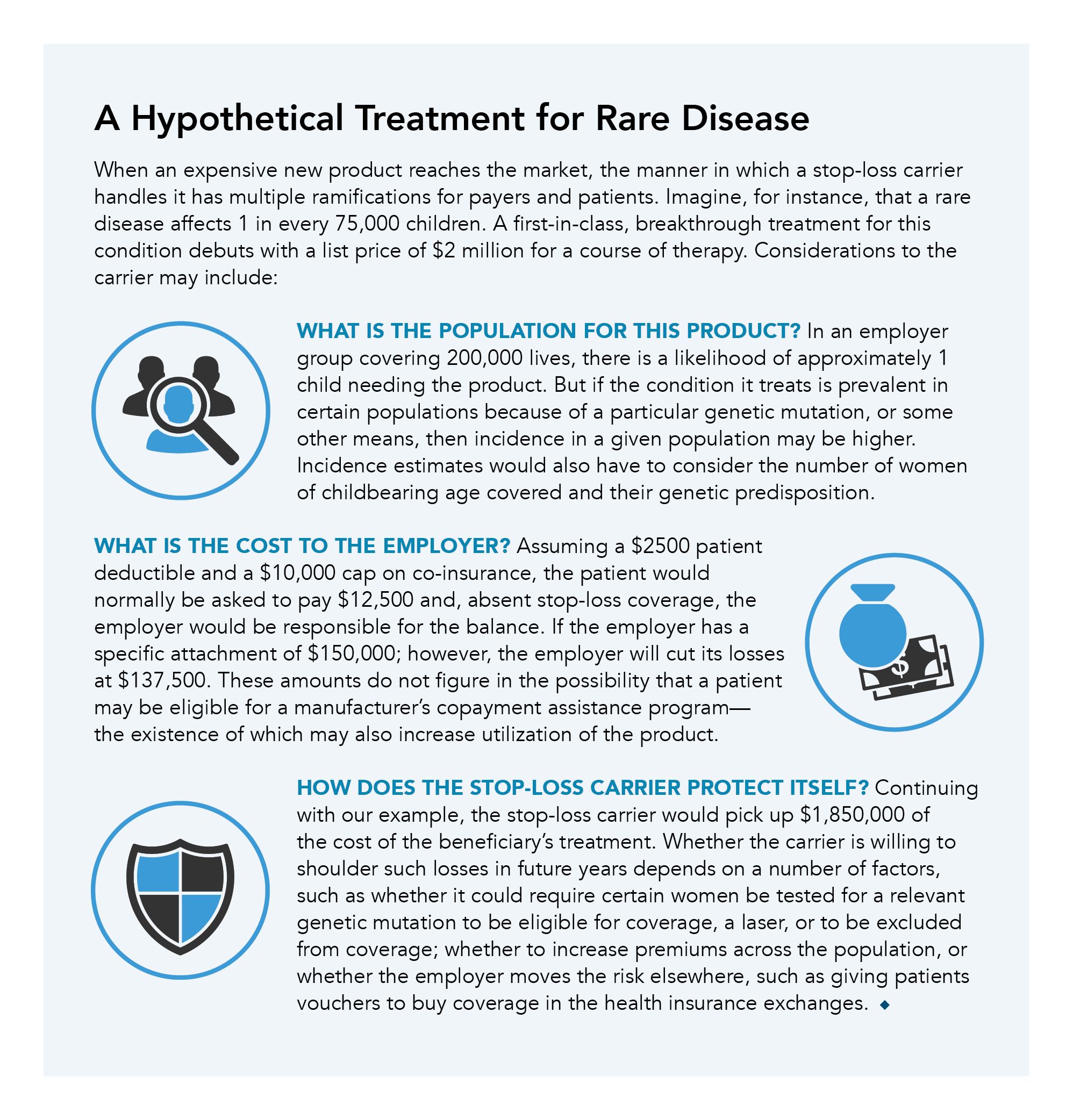
The uncertainty in how carriers may view and treat new products (see A Hypothetical Treatment for Rare Disease) underscores the need for manufacturers to communicate their pipelines in ways that convey meaningful value to each “customer”—not just investors, but also to employers, clinical nurse reviewers at traditional insurers, and even to stop-loss claims teams.
Hypothetical Treatment for Rare Disease
Where We Go From Here
Historically, stop-loss carriers have functioned as traditional insurers, using actuarial analyses to determine their potential responsibility for otherwise random risk. As the emergence of costly therapies for conditions that can be expected to occur causes stakeholders to rethink reinsurance, employers and payers may lose or have limited access to a tool that is vital to their efforts to finance health care delivery.
Failure to address this problem has multiple potential ramifications. As patients are lasered or carved out altogether, costs rise for both plan sponsors and patients through higher premiums and cost sharing, respectively. Payers may tighten coverage policies for costly therapies, with the potential to limit or delay access to therapy. The loss of secondary reinsurers may lead to health plan consolidation and a decrease in state and regional health plans, as only the large national players will be able to absorb the risk of high-cost treatments. And self-insured employers—especially smaller ones—might find that giving beneficiaries vouchers to shop for coverage in the health exchanges is cheaper than self-insuring. That’s not say the future is grim. To the contrary, creative thinking can open several paths forward:
SOLICIT COOPERATION ACROSS ENTITIES. Manufacturers will need to communicate value, ensuring that traditional and stop-loss payers have an accurate understanding of a drug’s place in therapy and which patients are appropriate candidates for it. Consider how trade groups (eg, the Academy of Managed Care Pharmacy and the Pharmaceutical Care Management Association) and patient advocacy organizations can be part of the solution.
INCLUDE STOP-LOSS PROVIDERS IN RISK SHARING ARRANGEMENTS. There is a need for payers to give stop-loss carriers a seat at the table when developing coverage policy for new products and to treat them as partners in outcomes-based or other nontraditional payment structures. Manufacturers will need to think about tools, such as warranties, that may help payers manage the financial challenges inherent with innovation.
CREATE A NEW BENEFIT FOR HIGH-COST THERAPIES. Vertically integrated traditional insurers are beginning to fill the void created by stop-loss exceptions, offering protection plans that cover 1 or more specific high-cost therapies in exchange for a per-member, per-month fee. This model does not include supportive care that a member might need and leverages aggregate volume to support claims expenses. These models rely heavily on the integrated company’s data capabilities and offer a nuanced alternative to traditional stop-loss dollar limits.13
POOL AGGREGATE RISK. The current paradigm is for individual employers to purchase stop-loss coverage for their own work forces. As an alternative, self-insured employers may investigate whether to form or join a captive—in essence, a private insurer set up by a small employer or group of employers to pool risk—to absorb some of shock from the self-funded plan. Doing so might mitigate the need for patient exclusions in stop-loss coverage.
LEVERAGE MANUFACTURER, PATIENT REGISTRY, AND CLAIMS DATA. When it comes to rare diseases and treatments for them, manufacturers and payers have an opportunity to partner with one another by tracking patient outcomes over time and sharing de-identified data. This real-world monitoring of clinical and financial outcomes can lead to the development of realistic risk profiles and may ease barriers related to portability of coverage when a patient finds new coverage and to portability of risk for the new payer.
COOPERATE WITH TECHNOLOGY DEVELOPERS. After federal incentives for providers to embrace electronic health record (EHR) systems took effect, forward-looking pharmaceutical companies began to develop digital channel strategies and formed relationships with EHR vendors. Embedding referrals to patient assistance programs into EHRs may help to reduce the likelihood that a beneficiary who is at risk of being carved out by a stop-loss provider will be denied access to an expensive therapy.
Conclusions
Stop-loss coverage is a key risk-mitigation component for self-funded health plans. The emergence of gene therapies and other costly one-time treatments is forcing a re-examination of what stop-loss coverage is for and what all parties can do to provide patients with access to innovative treatment, prevent plan sponsors from catastrophic costs, and avoid reinsurers from exiting the market. When all parties are engaged in the discussion, solutions with “something for everyone” are possible.
AUTHOR INFORMATION
Marc Hixson, MBA, is the president and CEO of Coeus Consulting Group and has a background across many areas of biopharma and the health care system. Neil Minkoff, MD, serves as chief medical officer of Coeus and has been a senior physician leader at Harvard Pilgrim Health Care. Kim Gwiazdzinski, MBA, RPh, is the vice president of Outcomes and Value-Based Contracting of Coeus, with prior roles at Prime Therapeutics and Novo Nordisk. Jim Clement, MHA, is a partner at Coeus, specializing in strategy and outcomes and formerly with Aetna Pharmacy Services.
References
1. Employee Benefit Research Institute. Employer Trends in Self-Insured Health Plan Coverage. September 5, 2019. Accessed October 3, 2020. ebri.org/docs/default-source/infographics/36_ig-selfinsur-5sept19. pdf?sfvrsn=35603c2f_4
2. National Association of Insurance Commissioners. Stop-loss funding, self-funding and the ACA. 2015. Accessed October 3, 2020. naic.org/documents/SLI_SF.pdf
3. Medcost. Maximizing benefits, limiting risk. 2018. Accessed October 3, 2020. medcost.com/sites/default/files/2018-07/White%20Paper_StopLoss_8_13_FINAL.pdf
4. Giles PC. Demystifying medical stop loss lasers. QBE North America. 2017. Accessed October 3, 2020. qbe.com/us/-/media/north%20america/files/qbe%20insights/71354-misc-demystifying-lasers-white-paper-v2.pdf?la=en
5. Jensen K. What the fund? All about fully, partially, and self-funded health plans. Filice. 2015. Accessed October 3, 2020. filice.com/2015/08/26/funded-health-plans
6. Miller S. More small and midsize firms choose to self-insure. Society for Human Resource Management. July 29, 2016. Accessed October 3, 2020. newdigs.mit.edu/sites/default/files/NEWDIGS_FoCUS_Reinsurance_
190916.pdf.
7. Massachusetts Institute of Technology Center for Biomedical Innovation. The role of stop-loss insurance and reinsurance in managing performance-based agreements. September 16, 2019. Accessed October 3, 2020.https://newdigs.mit.edu/sites/default/files/NEWDIGS_Fo-
CUS_Reinsurance_190916.pdf.
8. Moore R. Time for self-funded health plan sponsors to revisit stop-loss insurance. Plan Sponsor. June 14, 2019. Accessed October 3, 2020. plansponsor.com/in-depth/time-self-funded-health-plan-sponsorsrevisit-stop-loss-insurance
9. Quinn C, Young C, Thomas J, Trusheim M. Estimating the clinical pipeline of cell and gene therapies and their potential economic impact on the US healthcare system. Value Health. 2019;22(6):621-626. doi:10.1016/j.jval.2019.03.014
10. Weintraub A. Move over, Novartis: Kite and Gilead break into CAR-T market with early axi-cel nod. Fierce Pharma. October 18, 2017. Accessed October 3, 2020. fiercepharma.com/regulatory/kite-and-gilead-joinnovartis-
red-hot-car-t-market-early-axi-cel-approval
11. Chase L. The 10 most expensive drugs in the U.S., period. GoodRx. August 25, 2020. Accessed October 3, 2020. goodrx.com/blog/most-expensive-drugs-period
12. Fuerstenberg R. How big can claims get? Mercer. May 9, 2019. Accessed October 3, 2020. mercer.us/our-thinking/healthcare/how-big-can-bigclaims-get.html
13. Greenberg B, Trebes N. Our take: how insurers are scrambling to cover multimillion-dollar gene therapies. Advisory Board Co. September 9, 2019. Accessed November 3, 2020. advisory.com/daily-briefing/2019/09/09/gene-therapies