- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Subcutaneous Trastuzumab Induces Immune Function in HER2+ Breast Cancer
Trastuzumab administered subcutaneously delivered unique immunomodulation effects vs intravenous trastuzumab in patients with treatment-naïve HER2-positive (HER2+) breast cancer
Targeted Oncology™ originally published this article. This version has been lightly edited.
Subcutaneous (SC) trastuzumab induced stromal tumor infiltrating lymphocyte (sTIL) enrichment and favorably varied immune parameters in patients with HER2-positive breast cancer with residual disease after neoadjuvant treatment and had comparable efficacy to intravenous (IV) trastuzumab, according to a study published in Journal for ImmunoTherapy of Cancer.
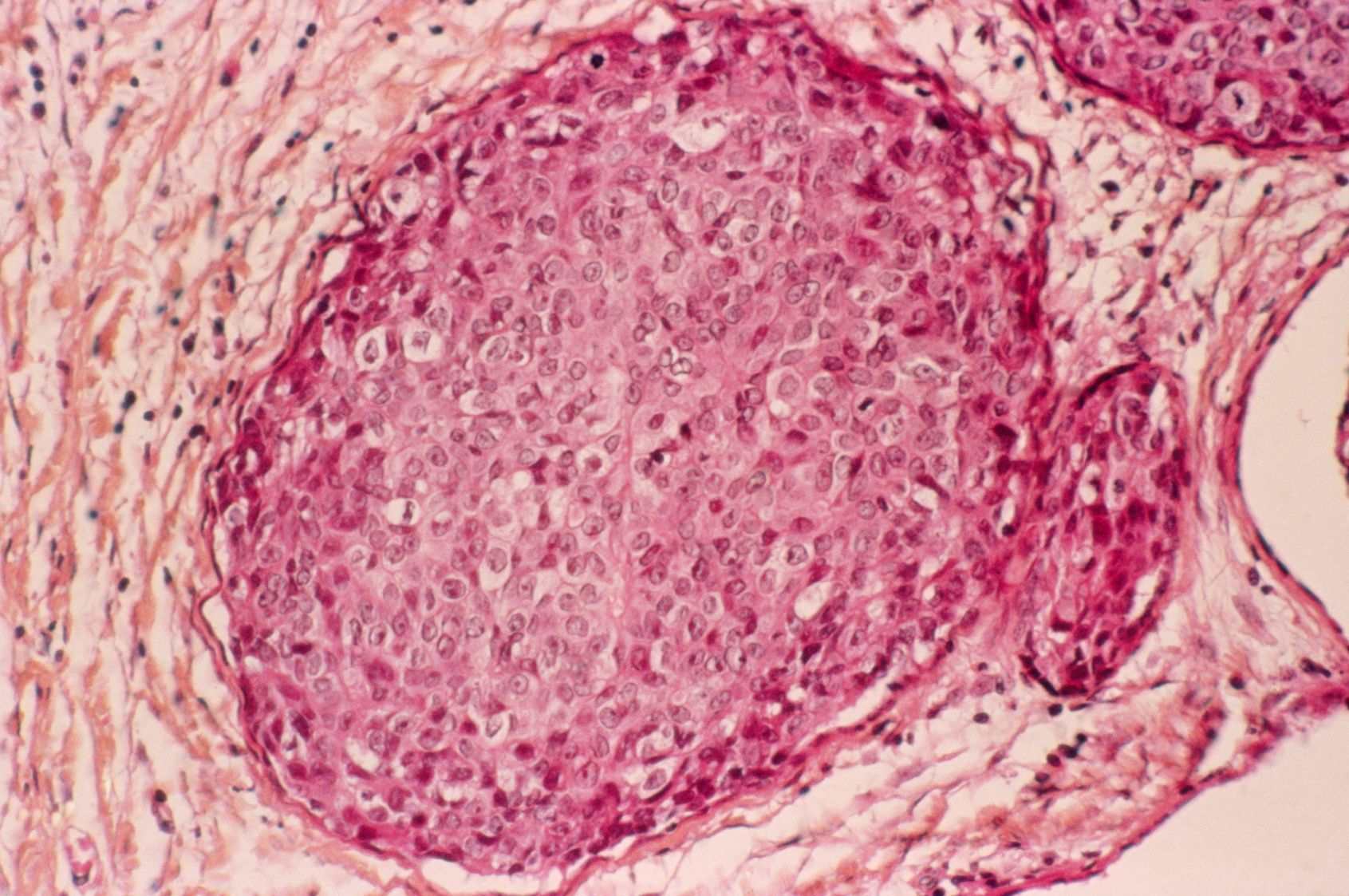
Breast cancer
Image Credit:Science RF - stock.adobe.com
Sixty-three patients were enrolled in the phase 2 IMMUN-HER study (NCT03144947) evaluating SC (n = 32) vs IV (n = 31) trastuzumab administration. In the IV trastuzumab arm, 20 of 31 patients (64.5%; 95% CI, 45.5%-80.1%) experienced a pathological complete response compared with 19 of 32 (59.4%; 95% CI, 40.1%-76.3%) patients in the SC trastuzumab arm. A relatively high rate (46%) of sTILs in postneoadjuvant residual tumors was seen in the SC administration arm compared with the IV administration arm (27%).
Further, an upregulation of PD-1 on sTILs of residual disease and a decline of CD4-positive FoxP3-positive regulatory T cells was observed in the SC administration arm, while PD-L1 was upregulated in residual tumors in the IV administration arm. Both arms had significant CD8-positive T-cell increases in residual disease.
“In our patients, PD-L1 expression on pretreatment sTILs inversely correlated with CD3 expression on sTILs in residual disease after SC trastuzumab, thus suggesting that SC administration of trastuzumab may favor a shift towards T-cell mediated antitumor response,” the study authors wrote.
For safety, 23% and 33% of adverse events (AEs) were associated with pertuzumab (Perjeta) plus docetaxel with IV or SC trastuzumab, respectively. Ninety-two percent of all patients experienced AEs, with most being mild (grade 1 or 2).
The study enrolled patients with treatment-naïve nonmetastatic HER2-positive breast cancer. Patients needed to have an Easter Cooperative Oncology Group performance status of 1 or below, baseline left ventricular ejection fraction of 55% or higher, and normal organ function.
Patients in the study received neoadjuvant IV 5-fluorouracil 500 mg/m2, epirubicin 75 mg/m2, and cyclophosphamide 500 mg/m2 every 3 weeks for 3 cycles. Patients were then randomized to receive IV trastuzumab, pertuzumab, and docetaxel or SC trastuzumab and IV pertuzumab and docetaxel every 3 weeks for 4 cycles. Patients underwent surgery 3 to 7 weeks after neoadjuvant therapy, and then they received either IV or SC trastuzumab every 3 weeks for 14 cycles. Docetaxel dose modification was permitted, but dose modification was not allowed for pertuzumab or trastuzumab.
“A more mature follow-up is required to look for distinct prognostic significance of residual diseases bearing different immune profiles of TILs after either SC or intravenous neoadjuvant trastuzumab,” the study authors wrote. “Based on our findings, novel immunotherapy strategies using [SC trastuzumab and pertuzumab] should be tested in clinical trials to achieve SC-specific, antitumor immune response.”
Reference
Pellegrino B, Tommasi C, Serra O, et al. Randomized, open-label, phase II, biomarker study of immune-mediated mechanism of action of neoadjuvant subcutaneous trastuzumab in patients with locally advanced, inflammatory, or early HER2-positive breast cancer-Immun-HER trial (GOIRC-01-2016). J Immunother Cancer. 2023;11(11):e007667. doi:10.1136/jitc-2023-007667
