- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Spontaneous Remission in Childhood Cancer Rare but Fleeting
A case report suggests vigilance is required even when cancers like acute lymphoblastic leukemia appear to go into remission without explanation.
In rare cases, patients with cancer experience the hopeful—but usually short-lived—phenomenon of spontaneous remission. A new case report outlines the experience of one such patient, but also highlights the need for better solutions when this occurs.
The case centers on a 3-year-old female patient who was diagnosed with precursor B-cell acute lymphoblastic leukemia (ALL) and later developed systemic Candida tropicalis infection. Subsequent to the infection, she experienced spontaneous remission of her ALL.
Benjamin J. McCormick, MD, of the Mayo Clinic, in Florida, and Hamayun Imran, MD, of the University of South Alabama, were the authors of the report, which was published in the journal Cureus.1
The patient first arrived at the clinic after her parents noticed fever, oral stomatitis, and pain in one leg and in her vaginal area. Upon admission to the hospital, she began vomiting blood. In their physical examination, clinicians noted hepatomegaly and mild cervical lymphadenopathy. She was given amoxicillin, but subsequent tests soon heightened concerns. Radiography showed suspicious lesions in her leg and lab work revealed pancytopenia.
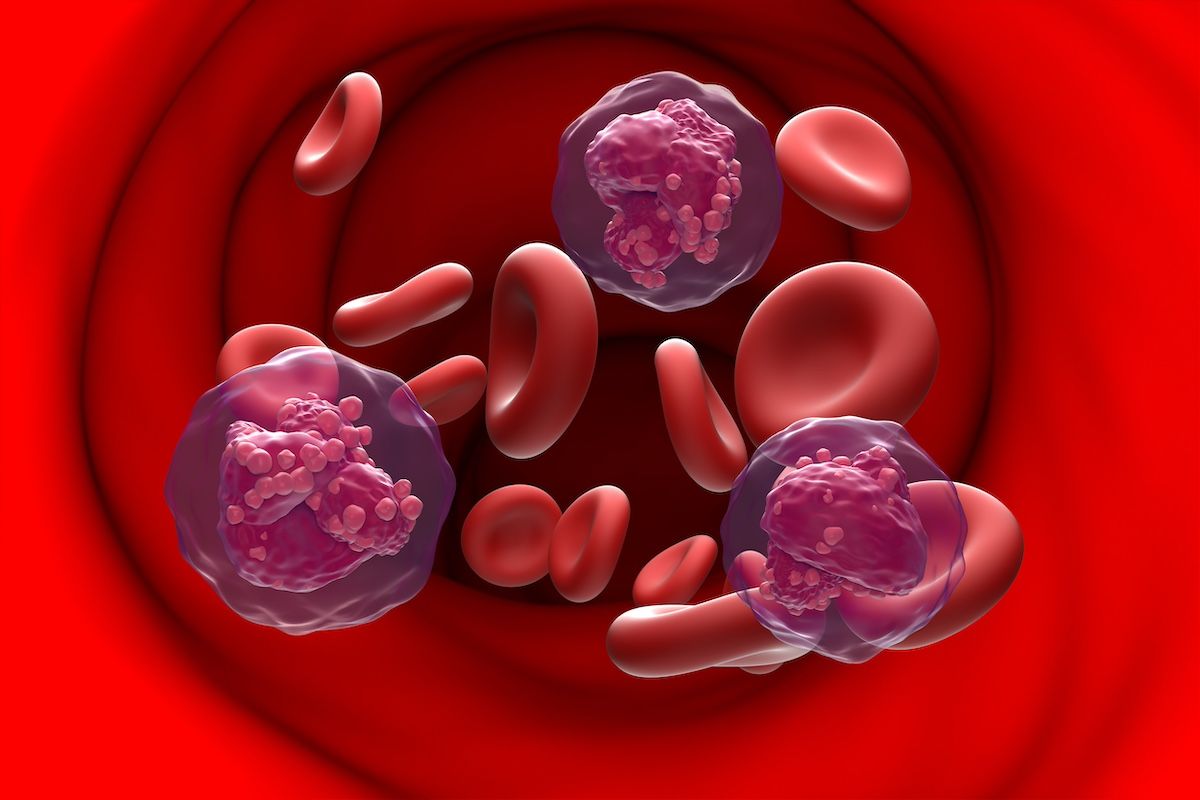
The 3-year-old patient was given consolidation therapy with the high-risk protocol AALL1131. | Image Credit: © Laszlo - stock.adobe.com
The patient’s physicians diagnosed her with standard-risk precursor-B ALL and began induction therapy with the Children’s Oncology Group (COG) protocol AALL0932 (intravenous cytarabine, vincristine, dexamethasone, pegaspargase, and intrathecal methotrexate). After a month, the patient’s bone marrow had 1.5% blasts on flow cytometry, and so she was given consolidation therapy with the high-risk protocol AALL1131 (cyclophosphamide, cytarabine, mercaptopurine, intrathecal methotrexate, vincristine, and pegaspargase).
Near the end of consolidation therapy, the patient experienced the first of a handful of pendulum swings in her condition. First, she was put into intensive care for septic shock and acute respiratory distress syndrome, after which clinicians diagnosed her with Candida tropicalis fungemia. The infection kept her hospitalized for more than 2 months, including 58 days on ventilation. Once she was removed from ventilation, a new bone marrow test found no evidence of residual ALL. The remission lasted 9 months through her hospital discharge. However, the remission did not last: 51 weeks after her last chemotherapy treatment, her care team diagnosed her with relapsed disease. She started reinduction therapy, but developed Escherichia coli septicemia and subsequently died.
McCormick and Imran said spontaneous remission is a rare, but not unprecedented, phenomenon. The authors said a search for similar cases of spontaneous remission among pediatric patients with ALL yielded fewer than 20 reported cases since 1996. In each case, they said, remission was temporary, lasting just weeks or months.
The authors found spontaneous remission to be somewhat more commonly reported in cases of pediatric acute myeloid leukemia (AML). A 1994 review of spontaneous remission reports in AML suggested that remission typically lasts between 0 and 16 months.2 That report noted that infections and transfusions had sometimes been associated with spontaneous remission, but the review found that neither was an “absolute requirement.”
As for spontaneous remission in ALL, McCormick and Imran said there are multiple theories about the cause.
“Several mechanisms have been proposed to explain the phenomenon of SR (spontaneous remission), including endogenous or iatrogenic steroid effects, cytokine mediation following sepsis, and cytotoxic T-cell surveillance of cancer cells,” they wrote.1
The cytokine theory is prevalent because cytokines have been shown in vitro to have anti-tumor effects, and some patients, like the one in this case report, had a history of fever with bacterial or viral septicemia prior to remission.
“It has been proposed that fungal toll-like receptors (eg, TLR2/TLR9), especially when compounded by a cytokine storm, may shift the immune system into an activated tumor microenvironment stimulating antileukemic effects,” they wrote.
However, the investigators said remission may likely be multifactorial in nature.
Yet, what is also clear, they said, is that spontaneous remission does not appear to be permanent. Given that reality, they said it may be preferable to use low-dose maintenance chemotherapy to improve the patient’s prognosis following spontaneous remission. There are no reports of that strategy being used, McCormick and Imran said, but given the current lack of guidelines on how to treat such patients, they said new strategies are needed.
References
- McCormick BJ, Imran H. Spontaneous remission of acute lymphoblastic leukemia following Candida tropicalis fungemia. Cureus. 2024;16(6):e62435. Published 2024 Jun 15. doi:10.7759/cureus.62435
- Delmer A, Heron E, Marie JP, Zittoun R. Spontaneous remission in acute myeloid leukaemia. Br J Haematol. 1994;87(4):880-882. doi:10.1111/j.1365-2141.1994.tb06762.x
