- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Skin Cancer’s Impact on American Indian/Alaska Native Communities Deserves More Consideration
A retrospective study showcases the need for considering the impact of skin cancers in non-Hispanic American Indian/Alaska Native communities, who experience some of the highest incidences of melanoma in the US.
A recent study published in JAMA Dermatology suggested that the rates of melanoma in non-Hispanic American Indian/Alaska Native communities deserve more consideration, highlighting the need to dedicate more research and attention to these individuals.
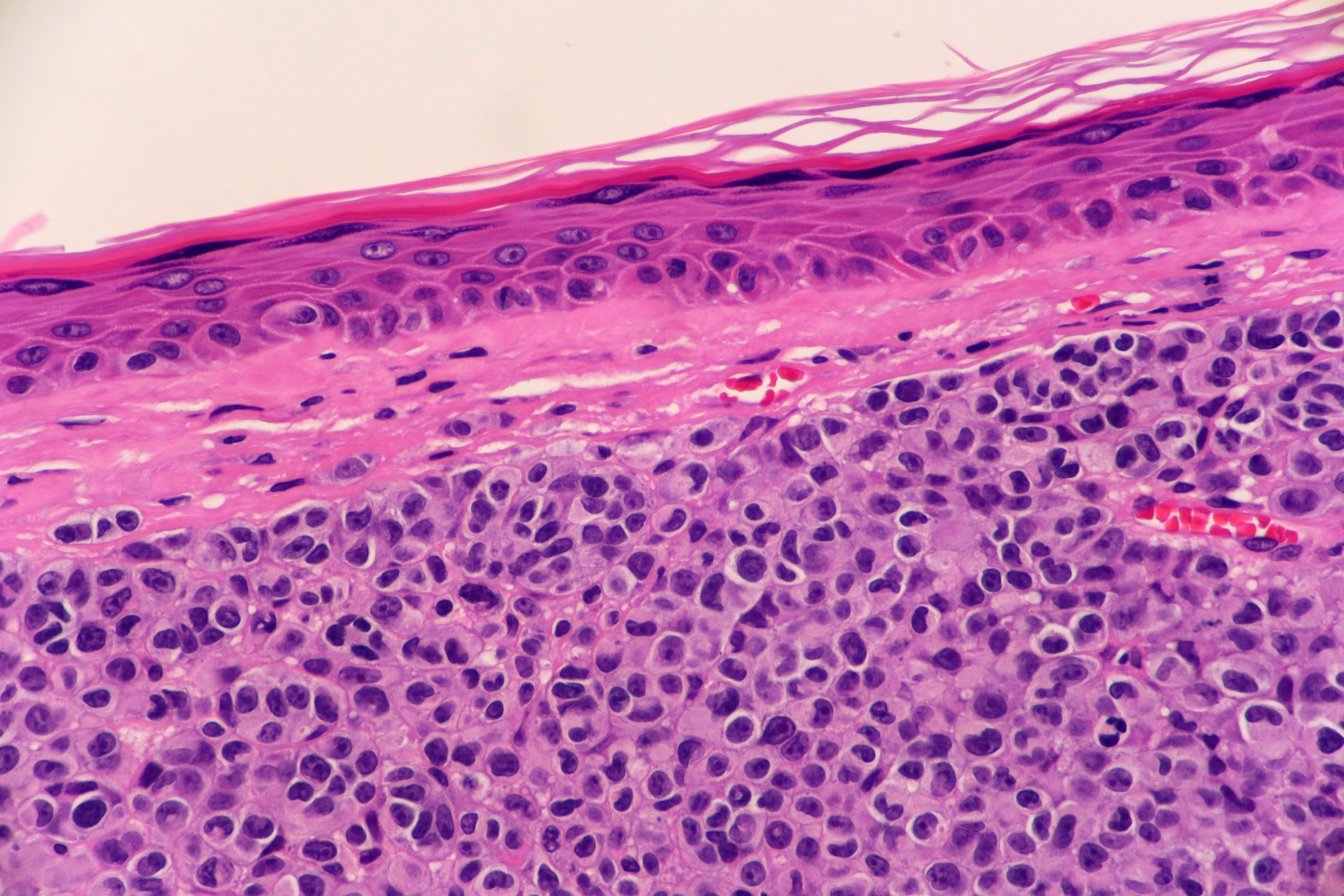
Microscopic View of Nodular Melanoma | image credit: Lisa - stock.adobe.com
At present, the non-Hispanic American Indian/Alaskan Native communities endure the second highest rates of melanoma in the US. These incidences are second behind the non-Hispanic White population; however, knowledge about melanoma trends affecting non-Hispanic American Indian/Alaska Native individuals is lacking. The authors of the present study hypothesize that this could stem from the smaller size of this community. However, given the impact of melanoma on these individuals, researchers designed a study to analyze the prevalence and patterns of melanoma in these communities.
From 1999 to 2019, data were gathered from a population-based cancer registry in connection to the Indian Health Service (IHS) database. For the purposes of this study, researchers valued this link to the IHS because, as the authors mention, American Indian/Alaska Native individuals are frequently miscategorized in various cancer registries as non-Native. Data found in connection to the IHS identified individuals with memberships to a federally recognized tribe who also had been receiving their health care from the IHS.
Researchers measured incidence rates of invasive cutaneous melanoma; grouped their assessment according to histology, tumor site, sex, age, socioeconomic factors, and stage at diagnosis; and analyzed these trends over time.
Notable results showed that incidences of melanoma, per 100,000 people, were lower in women (9.2; 95% CI, 8.6-9.8) compared with in men (13.0; 95% CI, 12.2-13.8). These incidences also increased with age in these groups. Notably, the authors mentioned that men 55 years and older had twice the incidence rate of melanoma compared with women of their same age (34.5 [95% CI, 31.8-37.3] vs 16.6 [95% CI, 15.1-18.3]).
The most prevalent type of histologic melanoma was melanoma not otherwise specified (6.1; 95% CI, 5.7-6.4), followed by superficial spreading melanoma (2.9; 95% CI, 2.6-3.1) and nodular melanoma (0.9; 95% CI, 0.7-1.0). Other forms of melanoma such as acral lentiginous melanomas and lentigo maligna melanomas were not commonly reported.
The analysis also examined rates of melanoma at the county level, specifically purchased/referred care delivery area (PRCDA) counties, meaning they hold or are adjacent to federally recognized tribal lands. Additionally, these counties contain more American Indian/Alaska Native individuals compared with non-PRCDA counties. Among PRCDA counties, researchers found that metropolitan PRCDA counties experienced higher rates of melanoma compared with PRCDA counties in smaller urban or rural areas (12.1 [95% CI, 11.4-12.9] vs 8.1 [95% CI, 7.2-9.2]).
Socioeconomic analyses revealed that these rates were lower in PRCDA counties with an economic status of distressed compared with those with a status of competitive or attainment (4.0 [95% CI, 3.3-4.7] vs 17.7 [95% CI, 15.8-19.8] vs 7.7 [95% CI, 6.1-9.7]). Furthermore, rates of melanoma were higher in the PRCDA counties with greater percentages of poverty and unemployment (8.2 [95% CI, 7.6-8.8] and 7.3 [95% CI, 6.8-7.9]). Those counties with more residents 65 years and older also had increased disease rates (lowest vs highest proportion: 9.9 [95% CI, 9.4-10.6] vs 12.3 [95% CI, 10.9-13.9]).
In their geographic analysis, it was seen that the men and women who lived in the Southern Plains region experienced higher incidences of melanoma (23.8 [95%CI, 21.5-26.2] and 15.5 [95%CI, 14.0-17.2], respectively). Incidence rates increased with age across all observed regions, and these instances increased between 1999 and 2016 for all individuals in these communities (P < .001).
“Access to specialty care services, including dermatology, may also be limited among American Indian/Alaska Native people who rely on the IHS system for health care,” the authors stated, adding that “Health care for American Indian/Alaska Native people has been historically underfunded, and access to dermatology services may be limited due to priority for referrals that need immediate attention.” The study’s results reinforce the need to recognize skin cancer as a problem facing American Indian/Alaska Native communities. As additional factors such as access could also influence the impact of these cancers, the authors encourage further studies be conducted to consider Indigenous perspectives, raise awareness, and explore potential intervention strategies and risk factors at play.
Reference
Townsend JS, Melkonian SC, Jim MA. Melanoma incidence rates among non-hispanic, American Indian/Alaska Native individuals, 1999-2019. JAMA Dermatol. Published online December 27, 2023. doi:10.1001/jamadermatol.2023.5226
