- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
SERENA-6 Trial Validates Molecular-Guided Therapy Switch to Camizestrant
Camizestrant significantly improves progression-free survival in advanced breast cancer patients with ESR1 mutations.
Early switching from an aromatase inhibitor to camizestrant (AstraZeneca) while continuing treatment with a CDK4/6 inhibitor is significantly more effective for treating hormone receptor–positive (HR+), HER2-negative (HER2–) advanced breast cancer with detectable ESR1 mutation vs continuing with an AI and a CDK4/6 inhibitor, according to new data. The treatment switch is meant to occur during first-line endocrine-based therapy and ahead of observable disease progression.
This is according to 2 studies from the phase 3 SERENA-6 trial (NCT04964934), which are evaluating camizestrant, an investigative, orally selective estrogen receptor degrader, in HR+/HER2– advanced breast cancer with ESR1 mutation, being presented at this year’s San Antonio Breast Cancer Symposium (SABCS).1,2 Together, these investigations demonstrate the efficacy of the camizestrant combination and its safe use in and tolerability by patients, as well as support the use of camizestrant plus a CDK4/6 inhibitor as a potential new treatment strategy in these patients.
SERENA-6 currently has 315 patients enrolled, who prior to switching to camizestrant were receiving one of the following combinations: palbociclib and anastrozole, palbociclib and letrozole, abemaciclib and anastrozole, abemaciclib and letrozole, ribociclib and anastrozole, or ribociclib and letrozole.3 Patients were switched to camizestrant at ESR1 mutation detection—using circulating tumor DNA (ctDNA) every 2 to 3 months.1
Camizestrant and Progression-Free Survival1
In this prespecified final progression-free survival (PFS) analysis, investigators explored the ctDNA dynamics of the ESR1 mutation using next-generation sequencing, comparing baseline measures to cycle 3 day 1 treatment measures (C3D1). The primary data cutoff was November 28, 2024, and the secondary, June 30, 2025. When the ESR1 mutation was detected, patients were randomized to receive either 75 mg camizestrant plus a CDK4/6 inhibitor (type and dose) plus placebo (n = 157) or to continue their aromatase inhibitor plus a CDK4/6 inhibitor plus placebo (n = 158).
There were significantly fewer PFS events in the camizestrant cohort vs the aromatase inhibitor cohort (90 vs 115), with the median PFS being 16.6 months (95% CI, 14.7-19.4) vs 9.2 months (95% CI, 7.2-9.7), for a 54% reduced risk of death (HR, 0.46; 95% CI, 0.34-0.62; P < .00001). At 2 years, the PFS rate was 32.2% vs 14.3%, respectively.
For the key secondary end point of PFS2, the numbers were only better for the camizestrant vs the aromatase inhibitor cohort:
- 62 vs 71 PFS2 events
- 25.7 months (95% CI, 20.3-28.9) vs 19.4 months (95% CI, 17.8-21.4) for median PFS2
- 50.9% vs 34.8% for PFS2 rate overall
In addition, for the secondary end point of chemotherapy-free/antibody-drug conjugate survival, again camizestrant prevailed
- 66 vs 76 survival events
- median survival of 22.7 vs 18.7 months (HR, 0.69)
- 37 vs 49 deterioration events
- median time to deterioration of 23.0 vs 8.3 months (HR, 0.49)
Overall, after 8 weeks (C3D1), the median (IQR) change from baseline in ESR1 mutation allele frequency via ctDNA was a 100% reduction in the camizestrant cohort but a 66.7% increase (–67.9% to 465.0%) in the aromatase inhibitor arm. Corresponding ESR1 mutation allele frequencies above 500% were 0.8% vs 24.4%.
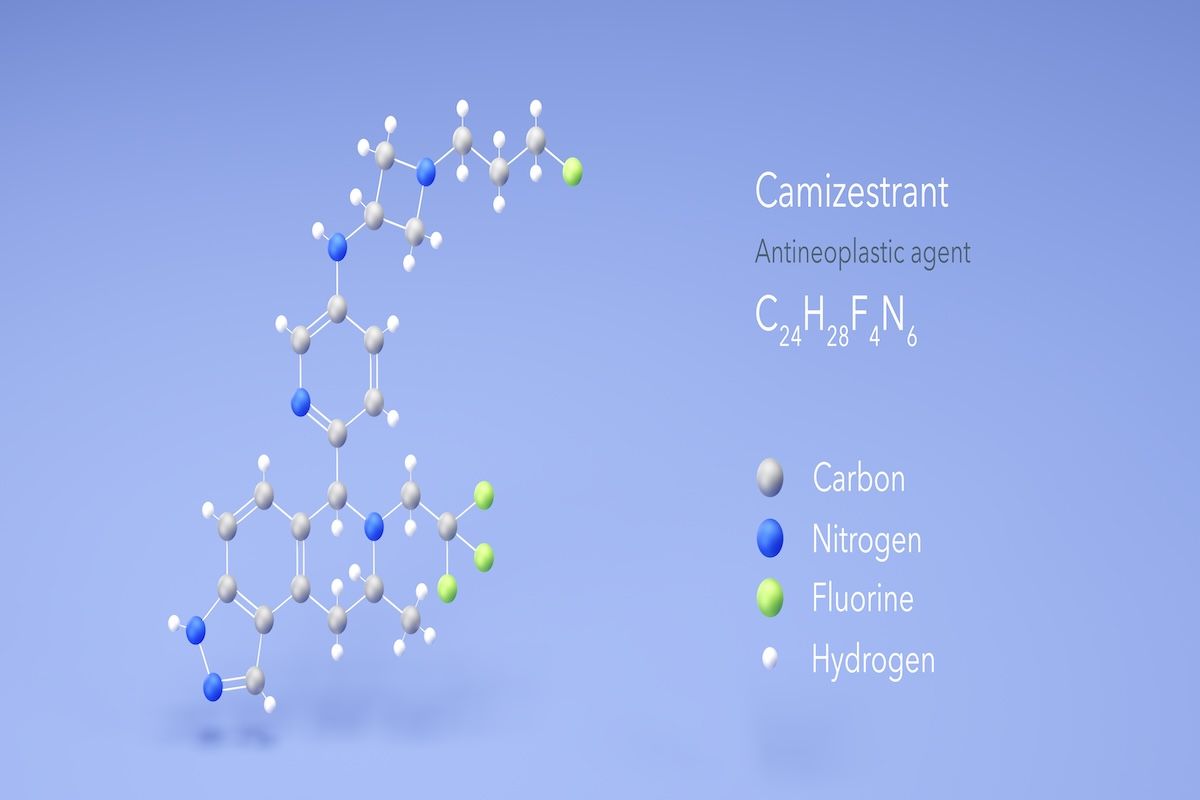
Updated SERENA-6 trial data on early switching from an aromatase inhibitor to camizestrant while continuing treatment with a CDK4/6 inhibitor show the new combination to be significantly more effective for treating HR+/HER2– advanced breast cancer with detectable ESR1 mutation. | Image Credit: © Сергей Шиманович-stock.adobe.com
Camizestrant and Vision2
“I think this is really the first evidence that using molecular progression, or molecular changes, to change therapy in metastatic breast cancer is a viable strategy,” said Adam Brufsky, MD, PhD, professor of medicine at the University of Pittsburgh School of Medicine, in an interview with The American Journal of Managed Care® (AJMC®).4 “Based on the FDA approval of camizestrant, it could potentially be a practice-changing trial.” Brufsky is presenting these findings on Friday, December 12, at SABCS.
This analysis drilled down to more detail on camizestrant’s visual impact on patients, measuring this at baseline and at weeks 26 and 52 after treatment initiation using the National Eye Institute 25-Item Visual Function Questionnaire (NEI-25). Ophthalmologic assessments were conducted at baseline, when clinically indicated, and after treatment ended. Photopsia, or seeing light flashes when not looking at light,5 was the most common nonhematological event in both patient groups in SERENA-6 (20%, camizestrant cohort; 8%, aromatase inhibitor cohort); also reported were blurred vision, visual impairment, diplopia, photophobia, and visual perseveration. The data cutoff was November 28, 2024.
Twice as many patients in the camizestrant cohort vs the aromatase inhibitor cohort reported impact on their vision (32.0% vs 16.1%). However, among the 49 patients in the camizestrant cohort who had this event, 90% were grade 1. Median times to visual adverse effect were 8 vs 23 days, respectively.
There were no treatment discontinuations or changes in visual acuity; both retinal and optic nerve integrity were preserved, and mean NEI-25 scores were comparable at weeks 26 and 52: 89.2 and 86.6 in the camizestrant cohort and 86.8 and 87.6 in the aromatase inhibitor cohort, with corresponding global vision ratings of 73.8 and 71.5 and 72.3 and 68.0. Altogether, these visual effects were mostly low grade and seen early in treatment.
References
- Bidard F, Mayer EL, Park Y, et al. Updated results and an exploratory analysis of ESR1m circulating tumor DNA (ctDNA) dynamics from SERENA-6, a phase 3 trial of camizestrant (CAMI) + CDK4/6 inhibitor (CDK4/6i) for emergent ESR1 mutations (ESR1m) during first-line (1L) endocrine-based therapy and ahead of disease progression in patients (pts) with HR+/HER2- advanced breast cancer (ABC). Presented at: San Antonio Breast Cancer Symposium; December 9-12, 2025; San Antonio, Texas. Abstract RF7-03.
- Brufsky A, Bidard F, Mayer EL, et al. Visual functioning and characterization of visual effects from SERENA-6, a Phase 3 study of switch to camizestrant (CAMI) from aromatase inhibitor (AI) while continuing CDK4/6 inhibitor (CDK4/6i) at emergence of ESR1 mutations (ESR1m) during first-line therapy for patients (pts) with HR+/HER2− advanced breast cancer (ABC). Presented at: San Antonio Breast Cancer Symposium; December 9-12, 2025; San Antonio, Texas. Poster PD10-04.
- 3.Phase III study to assess AZD9833+ CDK4/6 Inhibitor in HR+/HER2-MBC with detectable ESR1m before progression (SERENA-6) (SERENA-6). ClinicalTrials.gov. Updated October 7, 2025. Accessed December 11, 2025. https://clinicaltrials.gov/study/NCT04964934
- McCormick B, Brufsky A. Camizestrant-related photopsia mostly mild, nondisabling in patients with advanced breast cancer: Adam Brufsky, MD, PhD. AJMC. December 9, 2025. Accessed December 11, 2025. https://www.ajmc.com/view/camizestrant-related-photopsia-mostly-mild-nondisabling-in-patients-with-advanced-breast-cancer-adam-brufsky-md-phd
- Photopsia (eye flashes). Cleveland Clinic. Reviewed June 13, 2023. Accessed December 11, 2025. https://my.clevelandclinic.org/health/symptoms/25069-photopsias-eye-flashes
