- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Size Matters When It Comes to Cancer Drug Vials and Healthcare Waste, Says BMJ Study
The pharmaceutical industry needs to rethink its approach to packaging cancer drugs into a one-size vial to avoid drug wastage and save over $1.7 billion in 2016.
The pharmaceutical industry needs to rethink its approach to packaging cancer drugs into a one-size vial to avoid drug wastage and save over $1.7 billion (bn) in 2016, a new paper authored by researchers at the Memorial Sloan Kettering Cancer Center and the University of Chicago suggests.
The problem arises, the authors explain, from single-dose vials of a specific size for expensive cancer medications. The dose to be administered to a patient varies by body size, and most often than not, providers are left with excess drug in the vial, which is usually discarded because of safety concerns.
The authors list the following directives from federal agencies on the proper use of drugs available as single-dose vials:
FDA guideline. “Significantly more drug than is required for a single dose may result in the misuse of the leftover drug product. Similarly, the need to combine several single-dose vials for a single patient dose may lead to medication errors and microbial contamination.”
CMS advisory. “It is permissible for healthcare personnel to administer repackaged doses derived from [single-dose vials] to multiple patients, provided that each repackaged dose is used for a single patient in accordance with applicable storage and handling requirements.”
CDC guideline. “Vials labeled by the manufacturer as ‘single dose’ or ‘single use’ should only be used for a single patient. These medications typically lack antimicrobial preservatives and can become contaminated and serve as a source of infection when they are used inappropriately.”
To develop an estimate on the extent of this problem in oncology care, the authors analyzed spending on the top 20 cancer drugs, dosed based on body size, that are packaged as single-dose vials and collectively account for more than 93% if sales in the space. They estimated the total amount of leftover drug and the resulting 2016 revenues for each drug. Vial sharing was estimated based on Medicare claims data that included claims for amounts that did not match the full contents of the vial. The authors corrected for vial sharing percentage, adjusted the analysis to mirror a cancer patient population, and apportioned projected 2016 US revenues to administered or leftover drug.
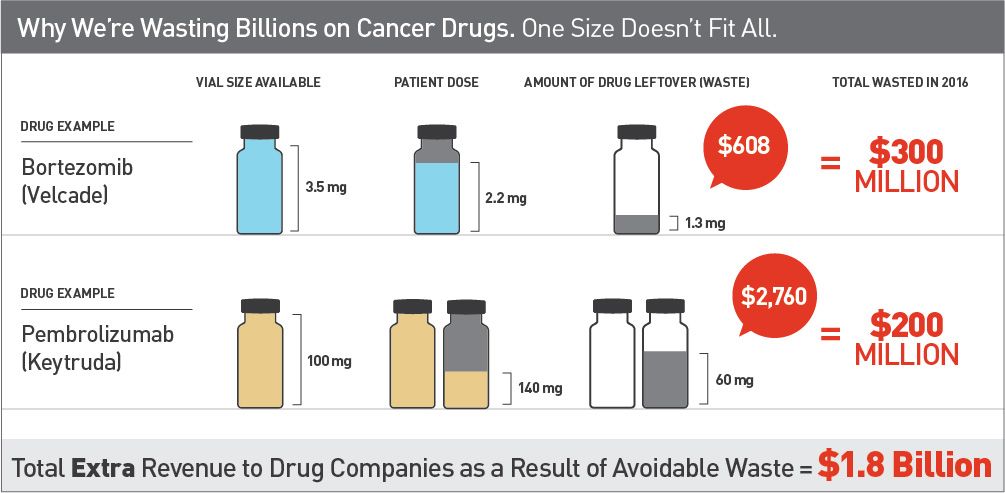
The results projected that the total US revenue from these drugs would be about $18 bn in 2016, 10% ($1.8 bn) of which will be from discarded drug. Specifically, the study estimated that,
- 7% of $3.9 bn in rituximab sales will be from discarded drug, totaling $254 million (m)
- 33% of $697 m in carfilzomib sales will be discarded, totaling nearly as much, $231m
The study goes on to suggest that if every patient received the highest dose approved by the FDA, revenue from discarded drugs would fall to $1.4 bn, and if every cancer patients weighed 10% less than the survey participants, the estimate would rise to $2 bn.
“This is all due to decisions about how much drug companies decide to put in each single dose vial. They almost certainly realize how these decisions translate into revenue,” said lead author Peter B. Bach, MD, director, Center for Health Policy and Outcomes, Memorial Sloan Kettering Cancer Center. “Vial contents can be selected to minimize rather than maximize waste, saving the U.S. health care system and patients billions of dollars. This is a rare opportunity to lower costs for patients and our healthcare system in a manner that cannot adversely affect health outcomes.”
The authors propose several policy options to overcome this waste and save costs, including multiple vial sizes and asking drug manufacturers to refund discarded-drug cost to health plans and CMS. A consensus among authorities at the FDA, CMS, and CDC on vial contents and vial sharing could also provide bigger savings to our healthcare system without compromising on outcomes, the authors write.
Reference
Bach PB, Conti RM, Muller RJ, Schnorr GC, Saltz LB. Overspending driven by oversized single dose vials of cancer drugs. BMJ. 2016;352:i788.
