- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Weighing Relapse Risk Against Benefit in Advanced NSCLC Immunotherapy: Jonathan Thompson, MD, MS
In advanced non–small cell lung cancer (NSCLC), discontinuing immunotherapy after 2 years can maintain durable responses while reducing financial and toxicity burdens, with decisions guided by residual disease testing and shared decision-making, explained Jonathan Thompson, MD, MS.
At a recent Institute for Value-Based Medicine® event, Jonathan Thompson, MD, MS, a hematology and medical oncology specialist and associate professor at Froedtert and the Medical College of Wisconsin in Milwaukee, discussed how in advanced non–small cell lung cancer (NSCLC), he typically targets 2 years of immunotherapy before considering discontinuation, noting that many patients maintain durable responses after stopping treatment.
Thompson emphasized using circulating tumor DNA (ctDNA) testing to assess minimal residual disease (MRD) and guide decision-making, while also counseling patients about relapse risk, the possibility of retreatment, financial burden, and the potential to avoid late-onset immune-related toxicities. Decisions are made collaboratively, with patients weighing the benefits of continuing vs stopping therapy at the 2-year mark.
This is the fifth part of a 6-part interview series with Thompson.
This transcript was lightly edited; captions were auto-generated.
Transcript
In advanced disease, how do you weigh indefinite immunotherapy against financial burden and explore time-limited strategies?
In the advanced or metastatic setting, I do commonly explore the opportunity to discontinue immunotherapy. Now we do have some evidence to guide us in that situation that many of the original immunotherapy trials in [NSCLC] had very discontinued immunotherapy at the 2-year mark. What we see from the readouts of those trials is that many patients who had an ongoing response at 2 years—even after discontinuing the immunotherapy—were able to maintain response without disease relapse. Commonly, I will shoot for 2 years of therapy and then consider discontinuing at that time point, given those data.
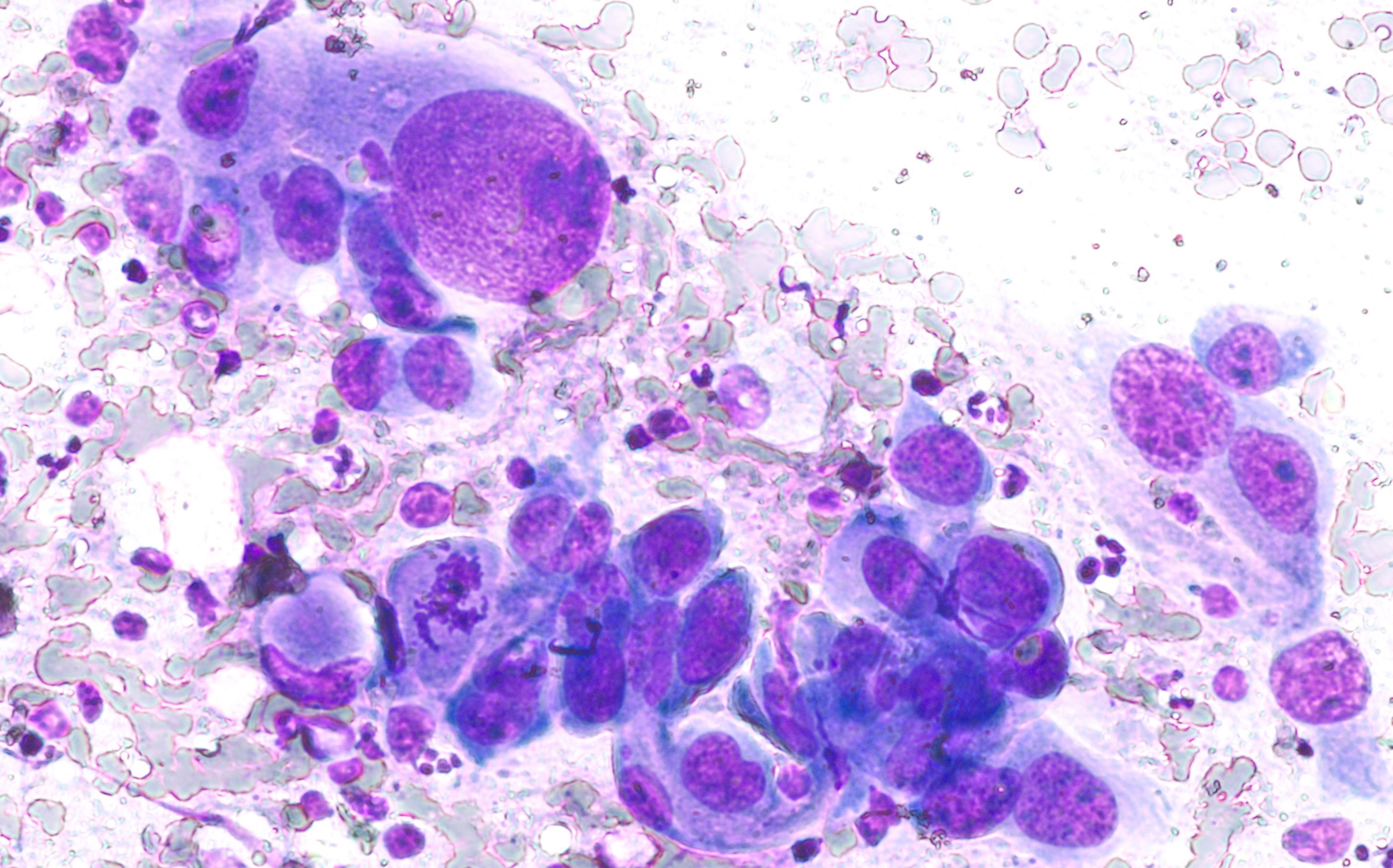
Phogomicrograph of fine needle aspiration cytology of a lung nodule showing non–small cell lung cancer. Image Credit: © David A Litman - stock.adobe.com
Now, typically around that 2-year mark, I'll be using other tools at my disposal to really try to understand if there is evidence of residual disease. I’ll use [ctDNA] tests for [MRD], just to really try to understand the depth of the response they've achieved with immunotherapy. We do tend to see that those who have a complete response with no clear evidence of residual disease generally have better long-term outcomes than those who still have evidence of disease at the 2-year mark.
Now, the challenge, though, is that even with all these tools, sometimes patients do have relapse of their disease after discontinuing immunotherapy. We do see sometimes [the disease] still remains sensitive to [immunotherapy], and we may reinitiate immunotherapy with success, but other times we see the disease is no longer sensitive to the immunotherapy.
These are all conversations to have with the patient as we counsel patients early that we're shooting for at least 2 years of treatment for most. We commonly continue to discuss that at various clinic visits as they're going through immunotherapy, and then we certainly have that detailed conversation right around the 2-year mark. It's truly a shared decision-making experience where I don't ever force patients off of immunotherapy if they're reluctant to do so, but a number of patients do see the value in discontinuing, not only from the financial toxicities that they can be alleviated from by no longer needing these expensive infusions [or] needing as many clinic visits, but also even after 2 years, patients can incur new immune-related adverse events, so those risks can be mitigated by discontinuing treatment.
