- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Retrospective Analysis Suggests Allo-HSCT Feasible for R/R DLBCL After CAR T Failure
Among the 10 patients in the retrospective analysis, the median overall survival after allogeneic hematopoietic stem cell transplantation (allo-HSCT) for relapsed/refractory diffuse large B-cell lymphoma (R/R DLBCL) was 21 months.
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a viable option for patients with relapsed/refractory diffuse large B-cell lymphoma (R/R DLBCL) who experienced failure with chimeric antigen receptor (CAR) T-cell therapy, according to a new report.
The report, which was based on a retrospective analysis of 10 cases, was published in Experimental Hematology & Oncology.
People with R/R DLBCL who fail CAR T are a particularly difficult-to-treat patient group, noted the study investigators. There is no standard chemotherapy regimen for these patients, and their prognosis is poor, they wrote. Given the limited options, the authors said one option that should be considered is allo-HSCT.
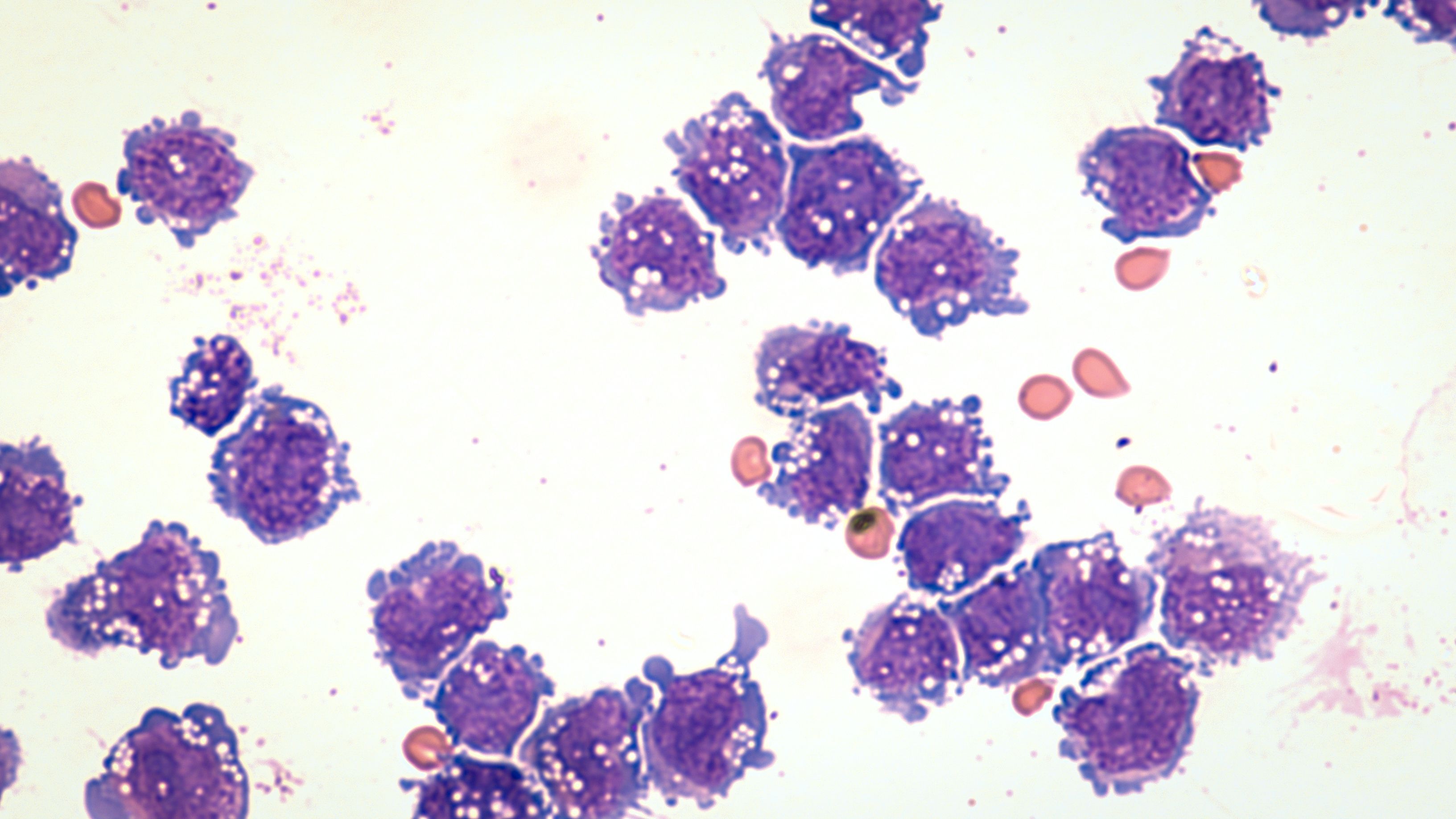
Microscopic image of diffuse large B-cell lymphoma
Image credit: David A Litman-stock.adobe.com
To better understand the efficacy and feasibility of the treatment, the authors retrospectively analyzed 10 patients with R/R DLBCL who received CAR T therapy at the First Affiliated Hospital of Soochow University, relapsed, and underwent allo-HSCT. Half of the patients were male and half of the patients were female. They ranged in age from 27 to 52 years, and their median (IQR) age was 43.5 (27-52) years. Eight of the patients had stage IV cancers, and the remaining patients had stage III disease. The patients were treated between October 2017 and June 2022.
Regarding their prior CAR T therapy, all patients received autologous CAR T treatments. In 4 cases, the therapy targeted CD19, and in the other 6 cases, patients received CD19-/CD22-targeted therapy. Three patients experienced a complete response, 4 patients had a partial response, and 3 patients had stable or progressive disease despite treatment.
Following failure of CAR T therapy, 2 patients were given venetoclax-based (Venclexta; AbbVie/Roche) salvage therapy, one patient received ibrutinib (Imbruvica; Pharmacyclics/Janssen) plus tislelizumab (Tevimbra; BeiGene), and the remaining 7 did not receive treatment until they were given allo-HSCT. The median gap between CAR T therapy and transplantation was 84.5 (31-370) days, the authors said.
At a median follow-up of 21 months, half of the patients had attained a complete response and 1 patient had a partial response to allo-HSCT. At 1 year, 7 of the patients had survived and 4 patients had progression-free survival (PFS). The median overall survival was 21 months, and the median PFS was 5 months.
Two patients experienced acute graft-vs-host disease (GVHD); one case was grade 3 and one was grade 2, the authors said. Mild chronic GVHD occurred in 1 patient. At the last follow-up, 2 patients had died due to relapse and progression, 1 had died due to acute renal failure, and 1 patient died due to severe pulmonary infection. Two patients had not experienced relapse.
The study investigators said the treatment paths of patients in China who relapse after CAR T therapy may differ due to the lack of availability of certain therapies there.
“FDA-approved therapies for R/R DLBCL, which can be employed after CAR T failure include polatuzumab vedotin (Polivy) plus bendamustine (Treanda) and rituximab (Rituxan), tafasitamab-lenalidomide (Monjuvi-Revlimid), and selinexor (Xpovio), which are not available in China,” they wrote.
In cases where such therapies are unavailable, they said allo-HSCT may be a worthwhile option. They said their data compare favorably to the otherwise “dismal” outcomes of patients who progress following CAR T therapy.
“[The study] has shown that allo-HSCT is a feasible and safe choice with favorable outcomes for R/R DLBCL patients with failure of CAR-T therapy,” they concluded.
Reference
Cong M, Ai S, Kang L, et al. Outcomes of allogeneic hematopoietic stem cell transplantation in R/R DLBCL patients with failure of CAR-T therapy. Exp Hematol Oncol. Published online January 16, 2024. doi:10.1186/s40164-024-00473-y
