- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Prophylaxis With Recombinant ADAMTS13 Demonstrates Superiority vs Standard Therapy in Congenital TTP
The multinational, open-label, controlled, randomized, crossover, phase 3 TAK-755 (NCT03393975) trial demonstrated superior efficacy and safety of recombinant ADAMTS13 as prophylaxis in patients with congenital thrombotic thrombocytopenic purpura (cTTP) compared with standard therapy.
The use of recombinant ADAMTS13 demonstrated efficacy and tolerability as a prophylactic therapy in patients with congenital thrombotic thrombocytopenic purpura (cTTP) compared with standard therapy, according to a recent study published in The New England Journal of Medicine.1
Thrombosis event concept | image credit: Matthieu - stock.adobe.com
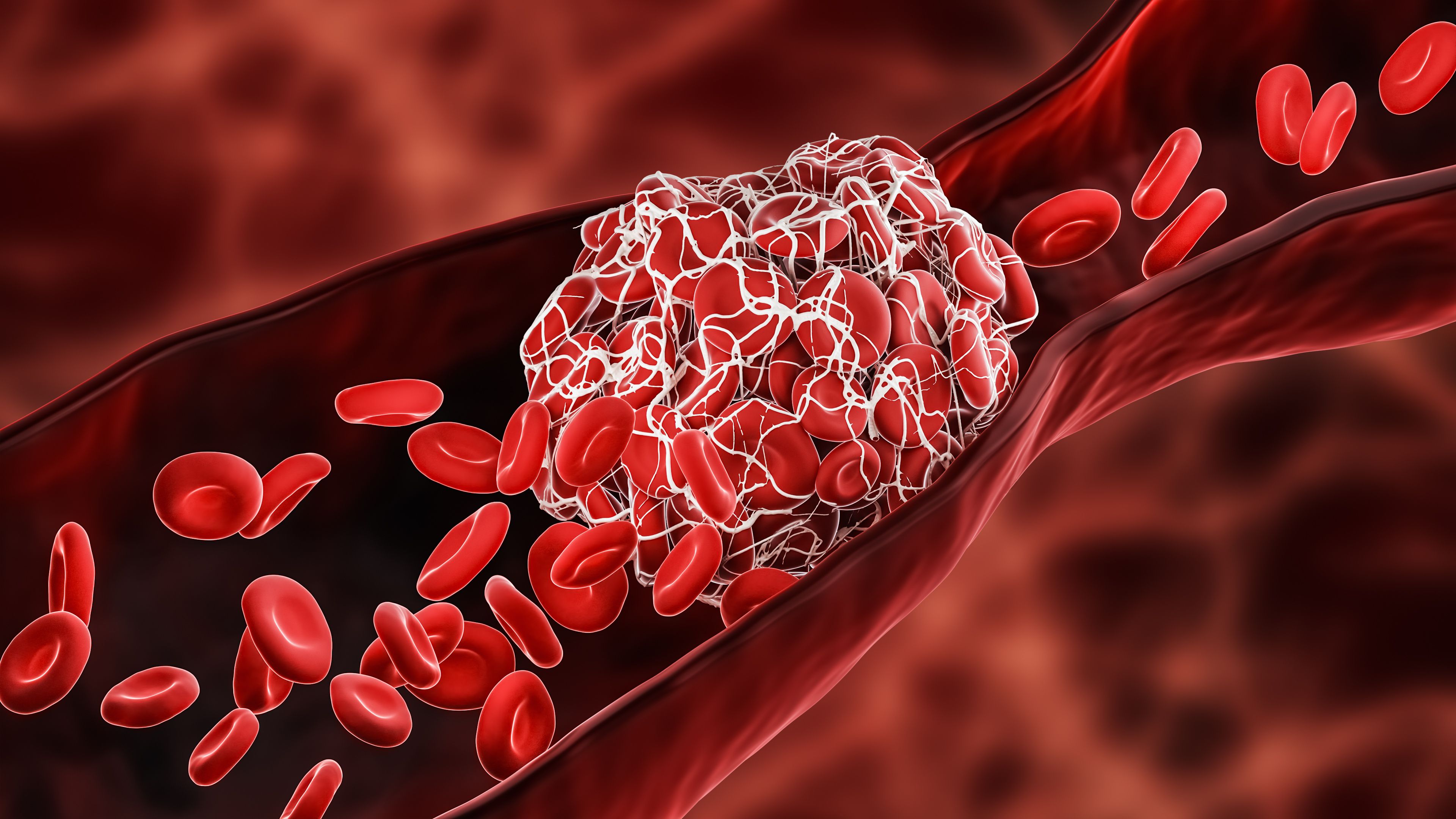
Fewer than 1000 individuals in the US are estimated to have cTTP, an autosomal recessive disorder characterized by low platelet levels, hemolytic anemia, and neurologic symptoms.2 Extensive thrombosis brought about by cTTP can additionally impact the nervous system and contribute to personality changes, bouts of confusion, headaches, and even seizures. Furthermore, the gastrointestinal tract, heart, and kidneys can be negatively affected by the abnormal clotting. This ultra-rare condition stems from a mutation in the ADAMTS13 gene, and symptoms can manifest at any age but commonly arise during infancy or throughout early childhood. Forms of trauma, infection, and pregnancy are known to trigger acute events in this condition.1
At present, ADAMTS13 replacement is the standard of care in cTTP—through various on-demand or prophylactic plasma infusions. Because these infusions depend on plasma from donors and, as the current authors add, can bring about significant burden (severe allergic reactions, lengthy time commitments, etc), exploring other forms of treatment could bring benefits to patient experiences and outcomes. To investigate this further, Scully et al reported results from the TAK-755 (NCT03393975) phase 3 trial, which compared the safety and efficacy of recombinant ADAMTS13 vs standard treatment for on-demand/prophylactic approaches in child and adult patients with cTTP.
This study enrolled patients between October 13, 2017, and August 12, 2022, and included data from 34 sites throughout the US, United Kingdom, Europe, and Japan. The authors split their patients into 2 cohorts: those who had treatment to stave off TTP events (prophylactic cohort) and those who had treatment after an existing event (on-demand cohort). At a ratio of 1:1, individuals were organized to receive prophylaxis with recombinant ADAMTS13 therapy (dosed at 40 IU per kilogram of body weight) or standard therapy. The treatment period lasted for 6 months before individuals switched to the alternative treatment for 6 months—following these periods, everyone underwent recombinant ADAMTS13 therapy for another 6 months. Researchers were primarily concerned with tracking the rate of experienced acute TTP events (defined as a 2-fold increase of lactate dehydrogenase levels from baseline, a 50% decrease in platelet levels, or a platelet level drop below 100,000 per mcL).
Of the 48 patients, 32 finished the trial. During prophylaxis treatment, 0 acute TTP events were reported. The most prevalent TTP event reported was thrombocytopenia, which occurred an annual rate of 0.74 during recombinant ADAMTS13 therapy (95% CI, 0.37-1.50) and 1.73 during standard therapy (95% CI, 0.92-3.23) during periods 1 and 2. Throughout these periods, the average platelet count was reported at 256 x 109 per liter for recombinant ADAMTS13 (95% CI, 121-391) and 239 x 109 per liter in standard therapy (95% CI, 113-364). The authors noted that 80% of patients receiving recombinant ADAMTS13 therapy had a higher average platelet count than those receiving standard therapy.
Overall, 71% of patients who had recombinant ADAMTS13 therapy experienced an adverse event compared with 84% of those with standard therapy. The investigators attributed these events to the trial drug in 48% of standard therapy cases compared with only 9% of recombinant ADAMTS13 cases. No patients receiving recombinant ADAMTS13 experienced an event that led them to discontinue or interrupt their time in the trial. There were 8 patients who had to interrupt or discontinue the trial in the standard therapy group.
Additionally, the authors reported that no neutralizing antibodies developed for those treated with recombinant ADAMTS13 therapy. This therapy group achieved an average maximum activity level of ADAMTS13 of 101% after recombinant ADAMTS13, whereas those after standard therapy achieved a maximum average of 19%.
References
1. Scully M, Antun A, Cataland SR, et al. Recombinant ADAMTS13 in congenital thrombotic thrombocytopenic purpura. N Engl J Med. 2024;390(17):1584-1596. doi:10.1056/NEJMoa2314793
2. Congenital thrombotic thrombocytopenic purpura. Genetic and Rare Diseases Information Center. Accessed June 4, 2024. https://rarediseases.info.nih.gov/diseases/9430/congenital-thrombotic-thrombocytopenic-purpura
