- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Most Diagnosed With Long COVID Were Never Hospitalized
The latest report from FAIR Health shows that the majority of people diagnosed post-COVID condition were never hospitalized.
The majority (75.8%) of patients diagnosed with a post-COVID condition had never been hospitalized for COVID-19, according to a new study from FAIR Health. Among patients who presented with a post-COVID diagnosis, 81.6% of females had not had a COVID-19 hospitalization compared with 67.5% of males.
The study was among the first to use the official ICD-10 diagnostic code (U09.9) for post-COVID conditions that became effective October 1, 2021. Analyzing private claims data from 78,252 patients diagnosed with the U09.9 code from October 1, 2021, to January 31, 2022, the study was released on May 18 as a white paper entitled Patients Diagnosed with Post-COVID Conditions: An Analysis of Private Healthcare Claims Using the Official ICD-10 Diagnostic Code.
Also known by such terms as long COVID and post-acute sequelae of COVID-19, post-COVID conditions comprise a wide range of health problems that may occur 4 weeks or more after infection with the virus that causes COVID-19. In the new FAIR Health study, the population of patients diagnosed with post-COVID conditions is analyzed by COVID-19 hospitalizations, age, gender, number of days from initial COVID-19 diagnosis to last post-COVID diagnosis during the study period, preexisting chronic comorbidities, co-occurring diagnoses and risk scores.
Among the key findings:
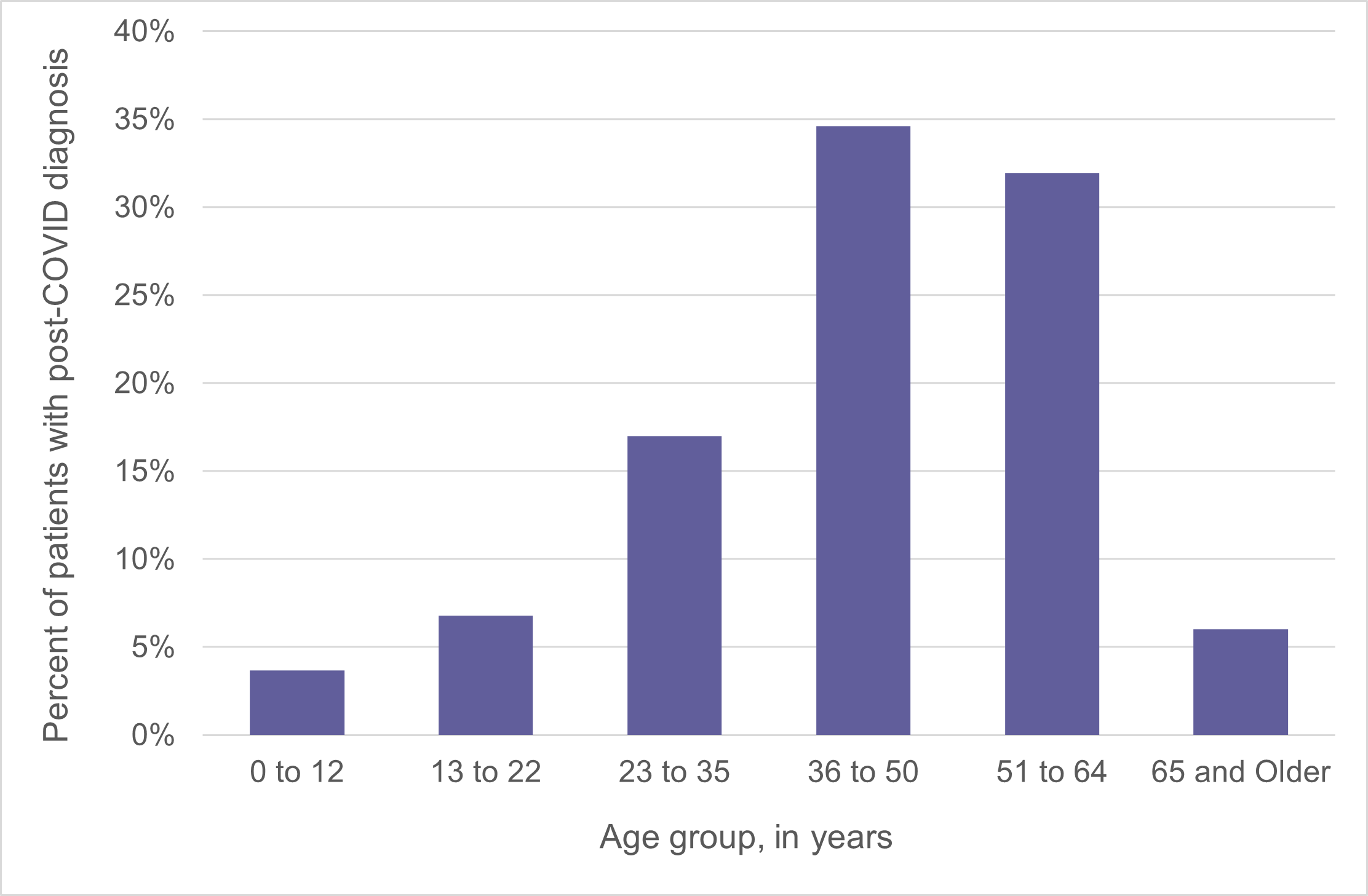
- The age group 36 to 50 was the most likely to be diagnosed with U09.9 post-COVID conditions; 34.6% of patients with that diagnosis were in that age group (FIGURE 1).
FIGURE 1
Females were more likely than males to be diagnosed with U09.9 post-COVID conditions. Females made up 59.8% of the population of patients with that diagnosis, while males made up 40.2% (FIGURE 2).
FIGURE 2
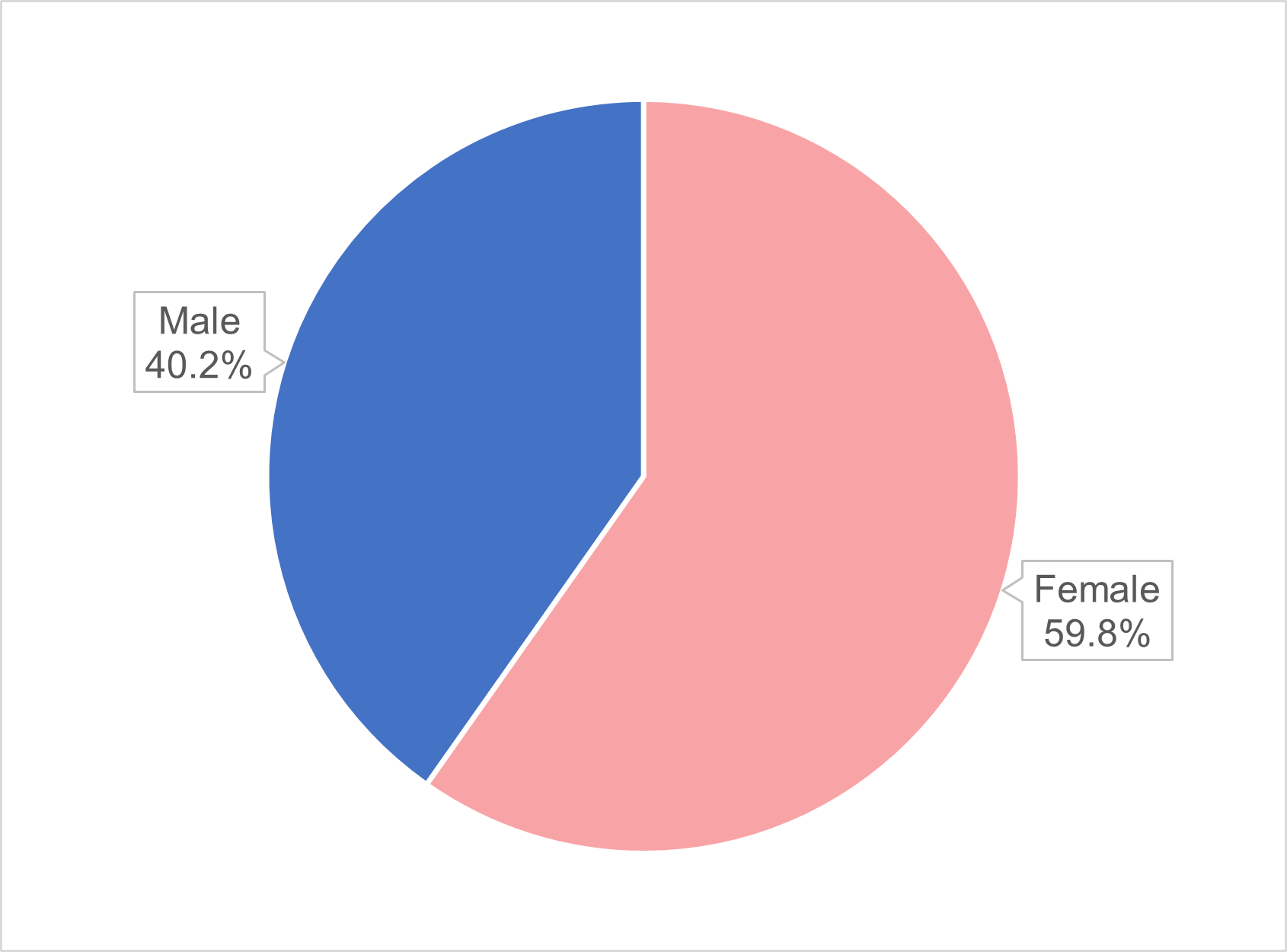
By comparison, within the cohort of people diagnosed with COVID-19 in the FAIR Health repository, 53.8% of patients were female and 46.2% were male.
Of patients who presented with a U09.9 post-COVID condition, 30.7% had no identified preexisting chronic comorbidities.
- The 3 diagnoses most commonly co-occurring on the same claim line with the U09.9 post-COVID diagnosis in patients across all ages and genders were abnormalities of breathing (23.2% of patients with post-COVID conditions), cough (18.9%) and malaise and fatigue (16.7%).
- In patients with a U09.9 post-COVID diagnosis, certain co-occurring diagnoses were more common in some age groups than across all age groups: for example, multisystem inflammatory syndrome in patients aged 0 to 12; abnormalities of heartbeat in the age group 13 to 22; generalized anxiety disorder in patients aged 23 to 35; and hypertensive diseases in the age group 65 and older.
- “Other and unspecified myopathies” (diseases that affect the muscles that control voluntary movement) occurred in patients in the post-COVID population 11.1 times more often than in the same population prior to COVID-19. Pulmonary embolism occurred 2.6 times more often. “Other disorders of brain,” including post-viral fatigue syndrome and certain forms of encephalopathy, occurred two times more often.
- On average, in all age groups, patients with a U09.9 post-COVID condition had higher Department of Health & Human Services-Hierarchical Condition Category (HHS-HCC) risk scores after their diagnosis of COVID-19 than before. HHS-HCC risk scores identify which patients are likely to consume more healthcare resources and potentially incur more healthcare-related costs in the long run.
Post-COVID conditions have become an issue of growing national concern. FAIR Health is pleased to shed light on this issue using the official ICD-10 diagnostic code for such conditions that became effective last fall. We hope these findings prove helpful for all individuals diagnosed with post-COVID conditions, as well as for providers, payors, policy makers and researchers.
This is the second FAIR Health study on post-COVID conditions; the first was released in June 2021, before the ICD-10 code for such conditions became effective. Other FAIR Health studies on the COVID-19 pandemic have examined projected US costs for COVID-19 patients requiring inpatient stays, the impact of the pandemic on hospitals and health systems, the impact on healthcare professionals, key characteristics of COVID-19 patients, the impact on the dental industry, risk factors for COVID-19 mortality, the impact on pediatric mental health and treatment and hospitalization costs.
For the new white paper, click here.
