- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
PET/CT Helps Predict Relapse in Patients With Myeloma Undergoing CAR T-Cell Therapy
Patients with extramedullary disease had inferior progression-free survival.
PET/CT scans can help identify patients with multiple myeloma (MM) who are at risk of adverse outcomes following treatment with chimeric antigen receptor (CAR) T-cell therapies, according to a new report published in HemaSphere.1 The authors of the study said their findings could help clinicians tailor therapeutic regimens to high-risk patients, for example, by incorporating concomitant radiation therapy.
PET/CT is a critical tool for MM staging, treatment response monitoring, and the detection of extramedullary disease (EMD), the authors explained. PET/CT has also been found to be a valuable prognostic indicator for patients with MM who undergo autologous stem cell transplantation (ASCT).2
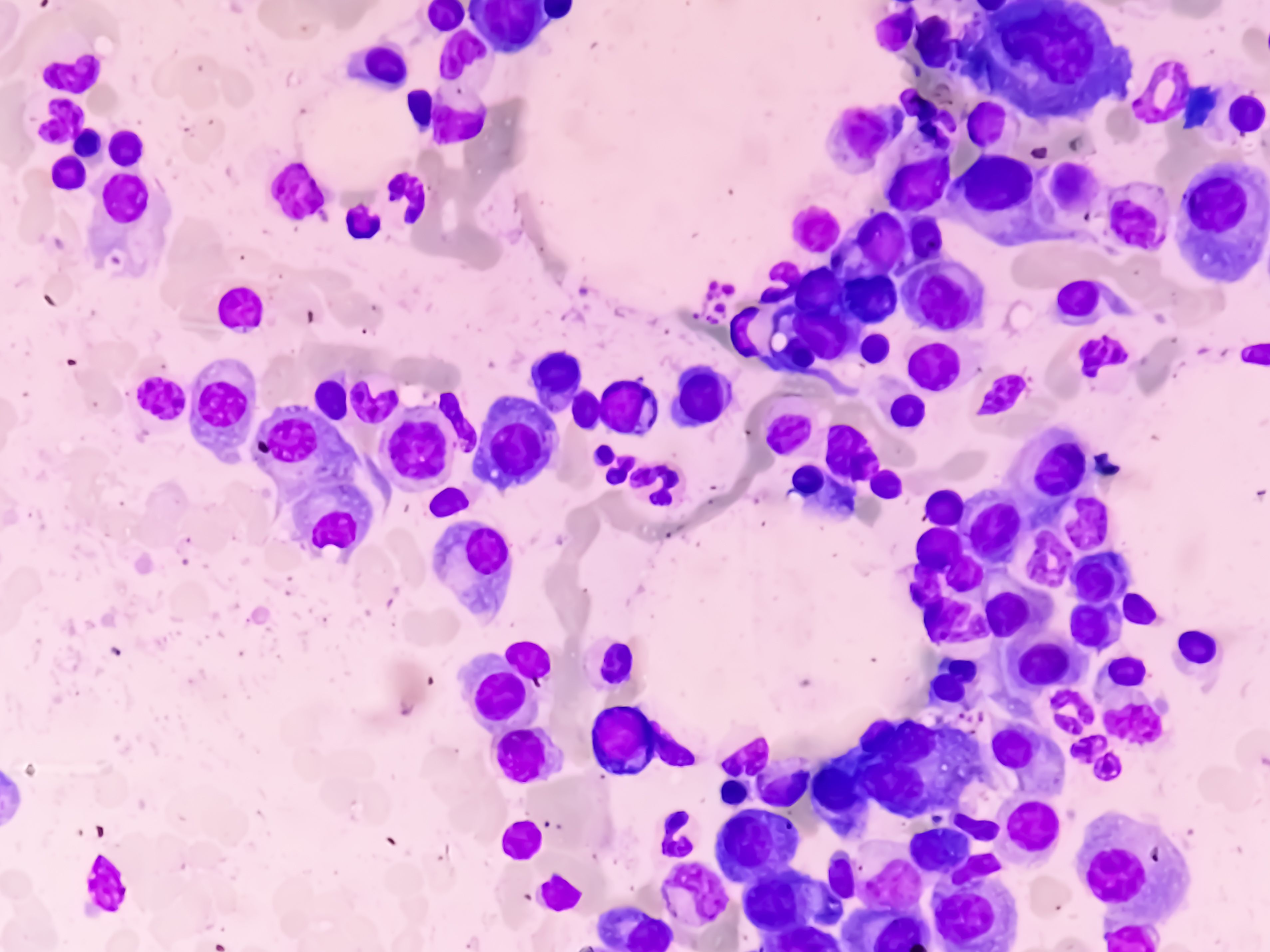
In follow-up PET/CTs, the investigators said those with complete metabolic remissions tended to have superior PFS. | Image credit: Saiful52 - stock.adobe.com
“However, its role in treatment with chimeric antigen receptor (CAR) T-cell therapies for relapsed/refractory multiple myeloma has yet to be clearly defined,” the authors wrote.1
In an effort to better understand potential associations between PET/CT imaging and outcomes for patients undergoing CAR T-cell therapy, the investigators identified 61 patients with MM who were treated with either idecabtagenevicleucel (ide-cel; Abecma) or ciltacabtageneautoleucel (cilta-cel; Carvykti).
Of the 61 patients, 53 patients had imaging performed prior to CAR T infusion, and 43 had imaging available from 30 days after infusion. The investigators compared those data to other biomarkers and patient outcomes to see whether PET/CT had prognostic value.
Patients who had bone-independent EMD had progression-free survival of just 3 months, compared to 15 months for those without bone-independent EMD (P = .01). The investigators found that EMD was associated with inferior progression-free survival (PFS), but the number of lesions was not, nor was metabolic tumor volume (MTV).
The authors said patients with high MTV had significantly higher baseline soluble B-cell maturation antigen (sBCMA) and interleukin-6 (IL-6) levels. However, they said higher MTV did not affect CAR T-cell expansion and did not decrease the fitness of the bystander T-cell compartment.
In follow-up PET/CTs, the investigators said those with complete metabolic remissions tended to have superior PFS.
“By evaluating PET/CT findings before and after treatment, we elucidated the complex interplay between tumor burden, metabolic activity, and patient outcomes, revealing novel insights into the stratification of high-risk individuals and potential avenues for optimizing therapeutic interventions,” the authors wrote.
Total MTV was linked with the risk of early relapse, which they said shows that volumetric tumor burden assessment has greater predictive value than lesion enumeration.
The authors noted that a significant downside of the use of PET/CT is that it is open to interpretation, and thus inter-observer variability occurs. However, they said incorporating the Italian Myeloma criteria for PET Use (IMPeTUs) led to a more standardized interpretation of PET/CT findings, which showed that patients with diffuse bone marrow uptake (>Deauville 3) had worse outcomes.
“Combining IMPeTUs-defined risk factors—EMD and marrow infiltration—proved highly effective in stratifying patients, enabling identification of individuals at risk for early relapse or extended survival,” they wrote.
Only 37% of patients achieved complete metabolic remission on follow-up, which the authors noted is an indication of why PET/CT can be valuable in detecting residual disease not captured by traditional biochemical markers.
The authors said their 30-day follow-up might be too short to fully capture treatment response and progression, and future studies are necessary to better understand how to use PET/CT in patient risk stratification and monitoring.
References
- Born P, Fandrei D, Wang SY, et al. Prognostic significance of PET/CT for CAR T cell therapy in relapsed/refractory multiple myeloma. Hemasphere. 2025;9(6):e70159. Published 2025 Jun 15. doi:10.1002/hem3.70159
- Moreau P, Attal M, Caillot D, et al. Prospective evaluation of magnetic resonance imaging and [18F]fluorodeoxyglucose positron emission tomography-computed tomography at diagnosis and before maintenance therapy in symptomatic patients with multiple myeloma included in the IFM/DFCI 2009 trial: results of the IMAJEM study. J Clin Oncol. 2017;35(25):2911-2918. doi:10.1200/JCO.2017.72.2975
