- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Patient Safety Improvements Save 87,000 Lives and $20 Billion
Efforts to improve patient safety have reduced hospital-acquired conditions by 17% from 2010 to 2014 and saved 87,000 lives and nearly $20 billion
Efforts to improve patient safety have reduced hospital-acquired conditions by 17% from 2010 to 2014 and saved 87,000 lives and nearly $20 billion, according to data released by HHS.
The report found that patients in the hospital experienced 2.1 million fewer hospital-acquired conditions. Hospital-acquired conditions include adverse drug events, catheter-associated urinary tract infections, central line associated bloodstream infections, pressure ulcers, and surgical site infections, among others.
Interim estimates for 2014 from HHS’ Agency for Healthcare Research and Quality (AHRQ) show the rate of hospital-acquired conditions staying steady from 2013. AHRQ estimates 36,000 fewer patients died in hospitals in 2014 as a result of the decline.
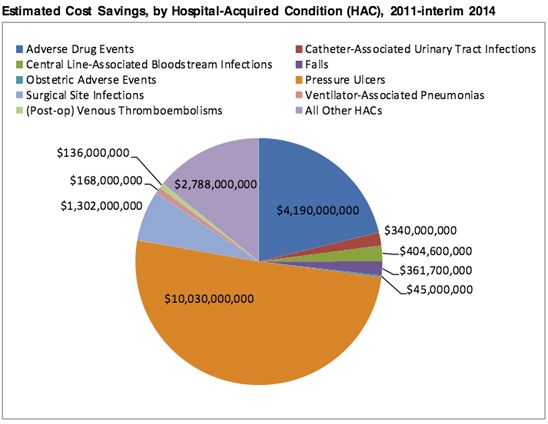
Image: HHS. Saving Lives and Saving Money: Hospital-Acquired Conditions. Update Interim Data From National Efforts To Make Care Safer, 2010—2014.
“Patients in America’s hospitals are safer today as a result of this partnership with hospitals and health care providers,” HHS Secretary Sylvia M. Burwell, said in a statement. “The Affordable Care Act has given us tools to build a better health care system that protects patients, improves quality, and makes the most of our health care dollars.”
The most deaths averted were as a result of pressure ulcers (42,716 deaths averted), followed by adverse drug events (16,670 deaths averted), and catheter-associated urinary tract infections (7922 deaths averted).
“While there is always more work to be done to improve patient safety, the collaborative efforts of hospitals and HHS have delivered great results that will continue to help the field on the quality improvement journey, said Rick Pollack, president and CEO of the American Hospital Association.
HHS associates the major strides in patient safety to efforts by the federal Partnership for Patients initiative, Hospital Engagement Networks, Quality Improvement Organizations, and other public and private partners.
“These results demonstrate that it’s possible to improve national patient safety performance resulting in millions of people avoiding infections and adverse events,” said Patrick Conway, MD, deputy administrator for innovation and quality and chief medical officer at CMS. “As a practicing physician, I know the importance of safety culture and care teams focused on keeping every patient as safe as possible.”
