- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
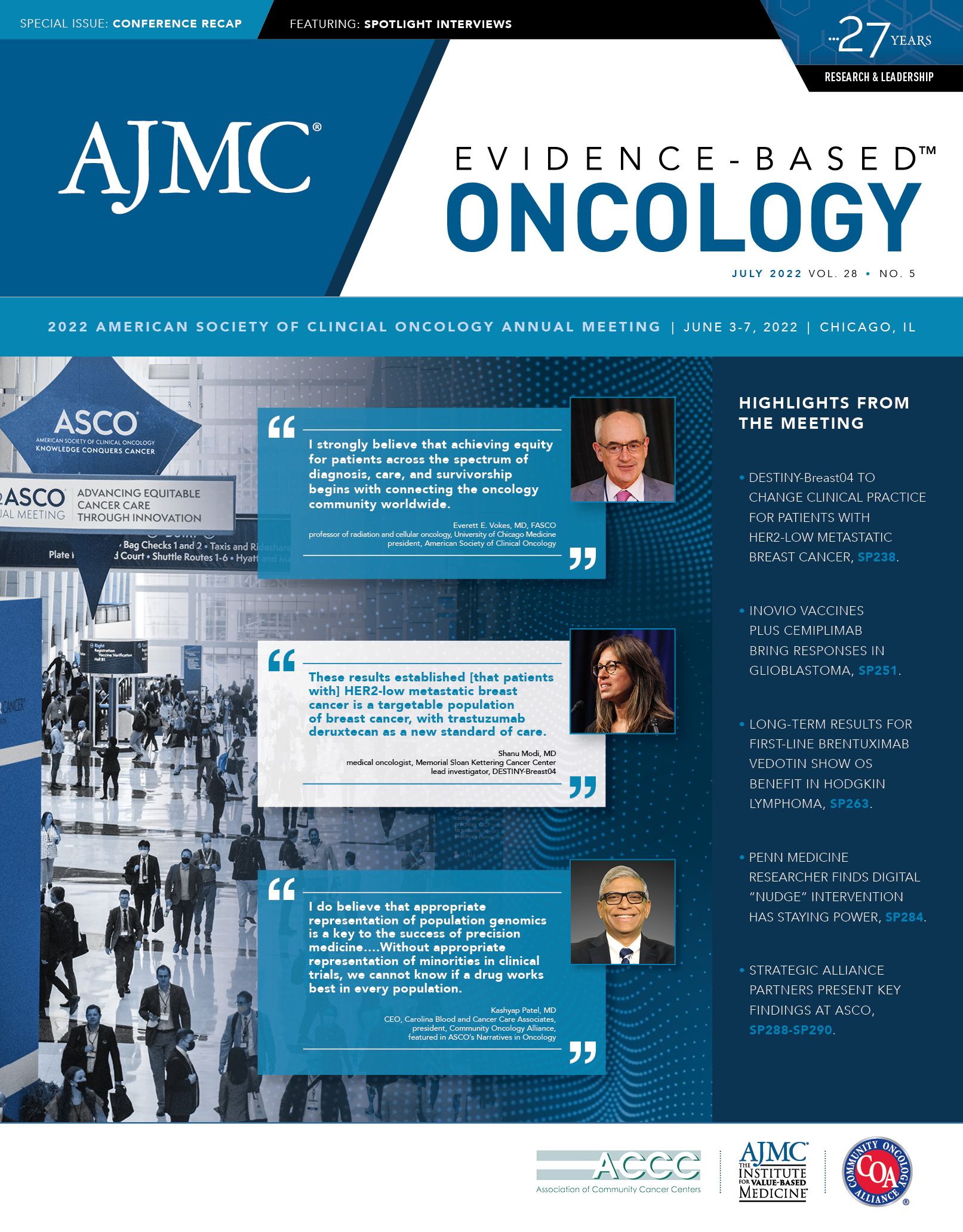
Over 6 Years, First-line Brentuximab Vedotin Cuts Risk of Death in Hodgkin Lymphoma by 41%
Data presented at ASCO show that after 6 years, patients with advanced Hodgkin lymphoma who were treated with a combination of brentuximab vedotin and chemotherapy had a sharply reduced risk of death and a reduced risk of a secondary cancer.
When first presented in 2017, results for ECHELON-1 (NCT01712490) showed a modest modified progression-free survival (PFS) benefit for brentuximab vedotin when given with chemotherapy in patients with previously untreated stage III or IV classic Hodgkin lymphoma.1
The trial compared the classic combination of doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine (ABVD) with brentuximab vedotin (Adcetris), doxorubicin, vinblastine, and dacarbazine (A + AVD) in patients with advanced Hodgkin lymphoma. Some taking the new regimen would experience peripheral neuropathy, and some would need growth factors. Early on, the question was whether it was worth it, given the adverse effects and the cost.
Six years later, the answer at the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting was a resounding yes, according to Stephen M. Ansell, MD, PhD, professor of medicine, Mayo Clinic College of Medicine, Rochester, Minnesota. On June 3, Ansell presented a prespecified update for ECHELON-1, which showed that over the long haul, the new combination with brentuximab vedotin cut the risk of death by 41% and the risk of secondary cancers for patients whose Hodgkin lymphoma was already advanced when they received their diagnosis.2 The results demonstrated that:
- After a median follow-up of 73 months, OS significantly favored A + AVD vs ABVD (HR, 0.590; 95% CI, 0.396-0.879; P = .009).
- 39 OS events occurred in the A + AVD arm vs 64 in the ABVD arm. Estimated 6-year OS rates were 93.3% for A + AVD compared with 89.4% for ABVD.
- The PFS benefit for A + AVD widened over time; at 6 years it was estimated to be 82.3% vs 74.5% for ABVD (HR, 0.678; 95% CI, 0.532-0.863).
- Fewer second malignancies were reported in the A + AVD arm than in the ABVD arm (23 vs 32).
- Although it was an imperfect measure of fertility, said study authors, more female patients in the A + AVD arm than in the ABVD arm reported pregnancy (49 vs 28) or live births (42 vs 19). No stillbirths were reported.
- No new safety signals were seen, and investigators reported that treatment-emergent peripheral neuropathy continued to resolve or improve in both arms over time; 86% and 87% of cases in the A + AVD and ABVD arms were reported to have resolved or improved by the last follow-up.
Ansell reviewed the design of ECHELON-1 and reminded the audience of several key elements: patients were randomly assigned 1:1 to receive up to 6 cycles of A + AVD (n = 664) or ABVD (n = 670) on days 1 and 15 every 28 days. He noted that 15% of patients were over age 60 years, and one-fourth had poor prognostic factors. Given this starting point, Ansell said the 6-year OS results are remarkable.
“This really shows that brentuximab vedotin plus chemotherapy significantly improved the overall survival, with a 41% reduction in the risk of death when compared with the standard ABVD chemotherapy,” he said. “Overall median survival was not reached, with a follow-up now of 73 months. This is highly significant.”
Results were mostly consistent across subgroups, including age. However, the one difference was that male patients appeared to have greater benefit than female patients.
A commentator on the abstract, Alison J. Moskowitz, MD, clinical director of Lymphoma at Memorial Sloan Kettering Cancer Center in New York, New York, said the latest data from ECHELON-1 highlight how far the treatment landscape has come in Hodgkin lymphoma since the 1960s, when the disease was “universally fatal.”
The ABVD regimen has been the standard since the mid-1970s, she said, with other regimens used as salvage therapies when ABVD failed. Moskowitz reviewed the criticism of ECHELON-1 and noted the seemingly small PFS benefit in the early results. “This was met with not that much enthusiasm initially,” she said. “One of the criticisms was the use of the modified progression-free survival, which can be associated with some bias, particularly in a nonblinded study.”
But the other issue was whether the observed benefit mattered. “Many people questioned whether this difference was big enough to justify the higher rates of peripheral neuropathy—as well as the [therapy’s] cost—and also the requirement for growth factors and for getting the highest rates of neutropenic fever.”
But with longer follow-up, “We saw the 3-year progression-free survival was starting to widen a bit. We also saw that this benefit was observed in patients with both stage III and stage IV disease.”
With more follow-up, the PFS was maintained, she said, and transferred to OS. “I agree with the prior speakers that this is now a preferred treatment for stage III and stage IV Hodgkin lymphoma.”
References
1. Connors JM, Jurczak W, Straus DJ, et al; ECHELON-1 Study Group. Brentuximab vedotin with chemotherapy for stage III or IV Hodgkin’s lymphoma. N Engl J Med. 2018;378(4):331-344. doi:10.1056/NEJMoa1708984
2. Ansell SM, Connors JM, Radford JA, et al. First-line brentuximab vedotin plus chemotherapy to improve overall survival in patients with stage III/IV classical Hodgkin lymphoma: an updated analysis of ECHELON-1. J Clin Oncol. 2022;40(suppl 16):7503. doi:10.1200/JCO.2022.40.16_suppl.7503
.