
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
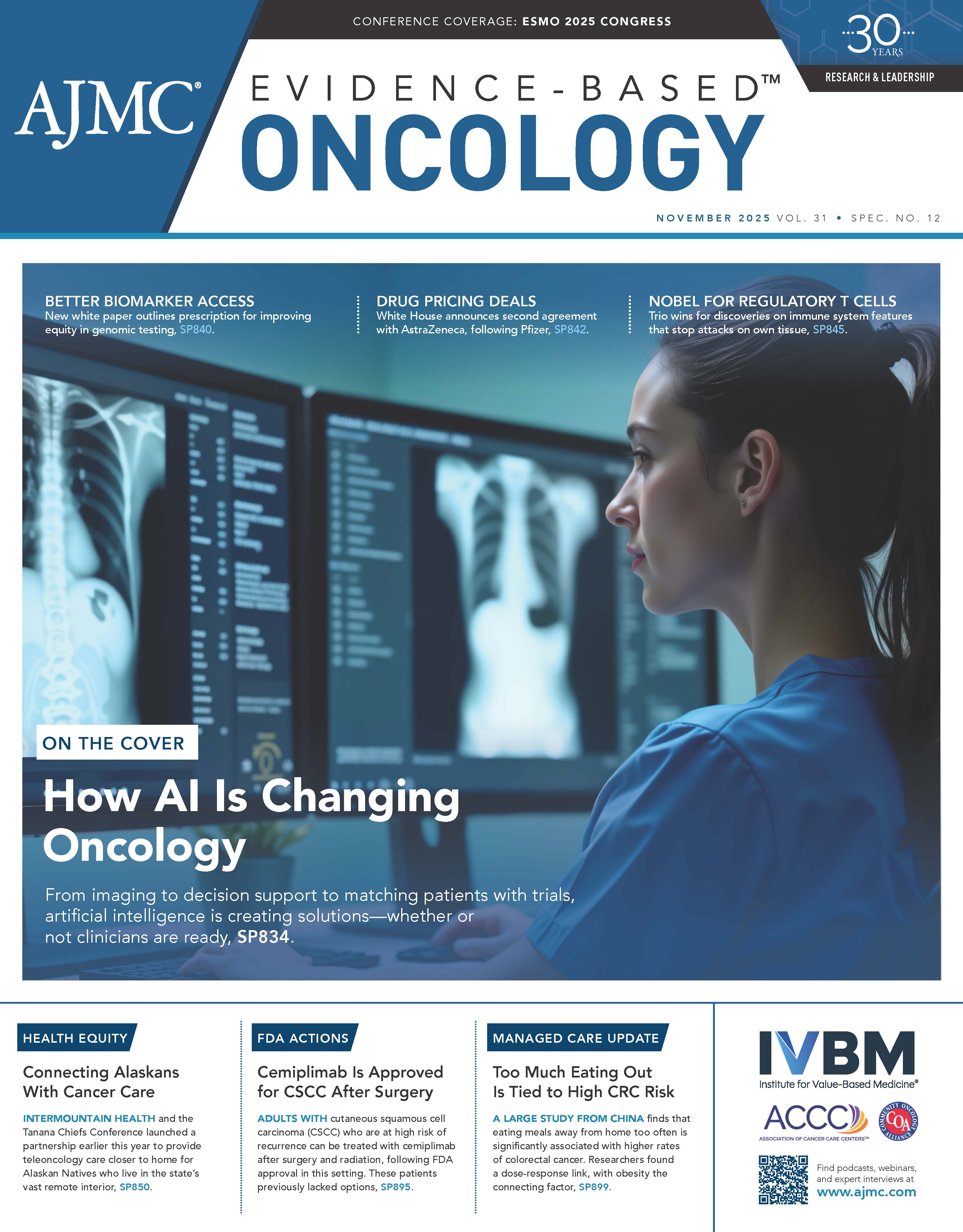
Navigating Costs and Logistics of Cellular Therapies, ADCs, and Novel Diagnostics in Cancer Care
Experts discuss the evolving landscape of CLL treatment, cellular therapies, and innovative diagnostics shaping patient care and cost-effectiveness in oncology.
The landscape of hematology and oncology is undergoing a rapid transformation, driven by innovative cellular therapies, time-limited regimens, highly targeted antibody-drug conjugates (ADCs), and precision diagnostics. Navigating this surge of novel treatments presents a critical challenge: how to maximize clinical efficacy and patient satisfaction while ensuring cost-efficient and streamlined care delivery.
At an Institute for Value-Based Medicine® event held September 11 in Salt Lake City, Utah, 4 expert panel discussions illuminated key areas where strategic thinking regarding access, logistics, and cost-utility assessment is paramount for realizing the full value of these breakthroughs.
Redefining CLL Treatment
Hu | Image: Huntsman Cancer Institute
Ermann | Image: Huntsman Cancer Institute
The management of chronic lymphocytic leukemia (CLL) is increasingly complex, moving beyond monotherapy to doublets, triplets, and fixed-duration schedules. A central discussion, moderated by Boyu Hu, MD, director of lymphoma and chronic lymphocytic leukemia at the University of Utah Huntsman Cancer Institute (Huntsman), revolved around optimizing treatment choices between continuous Bruton tyrosine kinase inhibitors (BTK inhibitors) and fixed-duration combination therapies such as obinutuzumab and venetoclax (Venclexta; AbbVie Inc/Genentech USA, Inc).
Treatment-naive patients have many options, with treatment decisions driven by patient preferences and what works with their lifestyle, explained Daniel Ermann, MD, associate professor in the Division of Hematology and Hematologic Malignancies at Huntsman. The long-term cost implications of indefinite therapy are substantial, and time-limited therapy may actually be more cost-effective overall,1 despite the immediate costs associated with infusions and intense monitoring.
“...the time-limited therapy wins out in regard to cost, even though there’s infusions and there’s all these labs and everything,” observed Ermann. This cost advantage stems from avoiding the sustained cost of indefinite oral medication and potential hospitalizations due to long-term adverse effects like bleeding or atrial fibrillation associated with continuous BTK inhibitor use.
The panelists largely favored a sequential approach, reserving the combination of agents for later lines of therapy or specific high-risk scenarios. This strategy leverages extended progression-free survival (PFS) intervals, effectively postponing subsequent costly therapies. Harsh Shah, DO, assistant professor of medicine at Huntsman, highlighted how disease biology drives selection, noting that certain high-risk features showed a median PFS of only about 54 months with fixed-duration venetoclax, whereas continuous BTK inhibitors offered 6- to 7-year PFS ranges for the same patient populations.2,3
Shah | Image: Huntsman Cancer Institute
“Now, certainly there will be patients who, for whatever reason, cannot tolerate a BTK inhibitor,” Shah said. “If someone has had a history of ventricular arrhythmia, that’s a patient that I’m not going to give a BTK inhibitor to. Or patients who require dual antiplatelet therapy, that’s sort of high risk to give a BTK inhibitor to.”
Toxicity and patient preference also heavily influence choice and costs. Although fixed-duration regimens offer a treatment-free interval that patients appreciate, they carry initial high toxicity, especially when including an anti-CD20 antibody like obinutuzumab, which increases infection risk.
Furthermore, the concept of “functional cure” emerged from the discussion, suggesting that if drugs are sequenced effectively, patients can achieve decades of survival without exhausting all options. Ermann noted that using a drug up front does not preclude its reuse later.
Finally, the discussion touched on the immense cost of curative potential therapies. Chimeric antigen receptor (CAR) T-cell therapy, while offering a potential cure for a fraction with CLL, comes with a staggering price tag. Furthermore, after CAR T-cell treatment, a careful evaluation of patient fitness is needed to guide future transplant decisions, noted Brian McClune, DO, associate professor at Huntsman.
“I’m probably going to draw human leukocyte antigen testing and make sure I have a donor identified and picked out, because we know, as good as it is to have a CAR T-cell product right now,…remission isn’t exactly what we’re missing in the lymphoma space.”
The Double-Edged Sword of Novel Diagnostics and ADCs in Breast Cancer
Havard | Image: Utah Cancer Specialists

In the breast cancer space, novel diagnostics, particularly circulating tumor DNA (ctDNA) for minimal residual disease assessment, and novel therapies are being adopted, leading to more strategic sequencing of therapies.
Although ctDNA testing has high clinical validity for predicting relapse, it currently lacks clinical utility—providers don’t yet know how to act on a positive result. In addition, they must contend with the rising costs of these tests, which remain outside clinical guidelines for routine use. Christos Vaklavas, MD, physician leader in breast cancer at Huntsman, emphasized the financial pressure created by these diagnostics, adding that one ctDNA test maker recently raised its prices.
“It’s a great test, but we don’t know what to do with it, with a result,” he said. “I think, for the time being, it sounds more problematic to draw it.”
Adding to the complexity are issues of unregulated patient access. Patients are obtaining ctDNA tests through nonphysician channels, leading to decisions that undermine established, evidence-based treatment plans. Robert Havard, MD, medical oncologist and hematologist at Utah Cancer Specialists, recounted a cautionary tale of a patient with very high-risk breast cancer who obtained a ctDNA test at a wellness clinic “and made pretty high-level clinical decisions based on the results of this test to not pursue any other treatment.”
This unregulated access poses a safety risk and may lead to costly relapses. Mei Wei, MD, an oncologist specializing in breast cancer at Huntsman, and moderator of the panel, stressed the need for controlled access.
“I think the access is good, but we need a better regulation to provide a patient with the appropriate access instead of all…the access,” she said.
Sequencing ADCs
ADCs are transforming metastatic breast cancer treatment and “have taken breast cancer by storm,” said Namita Chittoria, MBBS, MD, assistant professor at Huntsman. The challenge now lies in sequencing the 3 major ADCs—sacituzumab govitecan, trastuzumab deruxtecan (T-DXd), and datopotamab deruxtecan (Dato-DXd)—which carry different costs, adverse effect profiles, and long-term monitoring requirements.
When assessing value, toxicity management and associated costs are paramount. For instance, T-DXd requires frequent CT scans to monitor for interstitial lung disease, and Dato-DXd introduces quality-of-life issues with stomatitis and keratitis. Sacituzumab govitecan is generally well tolerated despite initial concerns about neutropenia and diarrhea. Chittoria also detailed the pricing structures, noting that single infusions can range from $10,000 to $20,000, depending on the agent and schedule.
The experts voiced caution regarding the sequencing of ADCs that share the same antigen target (TROP2) and similar payloads (such as Dato-DXd and sacituzumab govitecan). Vaklavas noted that sequentially using agents with identical targets and mechanisms of action significantly diminishes the second ADC’s efficacy. “I don’t think many of us will be enthusiastic to use an ADC with an identical target and the payload with [the] identical mechanism of action,” he cautioned.
CAR T, Bispecifics, and the Challenge of Scale and Access
Hunter | Image: Intermountain

During the third panel, the experts discussed how health systems and practices want to transition high-cost cellular immunotherapies from inpatient to outpatient settings to reduce infrastructure costs and improve patient experience.
Although most institutions start bispecific antibody and CAR T-cell therapies in the inpatient setting, LDS Hospital has successfully transitioned 90% of CAR T infusions to the outpatient setting, explained Bradley Hunter, MD, medical oncologist with Intermountain Healthcare. He emphasized that the transition requires extensive infrastructural build-out and system training, but the long-term benefits include reduced costs and increased patient satisfaction.
“I remind people…your general oncologist gives checkpoint inhibitors all the time. They are way more toxic than bispecific antibodies,” he said.
Bispecifics offer a distinct logistical advantage because they are an off-the-shelf treatment and easier to administer and master than highly specialized CAR T-cell therapy. Amandeep Godara, MBBS, associate professor at Huntsman, predicted that bispecifics would increasingly move into the community setting, especially with the use of prophylactic measures, such as tocilizumab, that cut the incidence of cytokine release syndrome (CRS) from as high as 70% down to 10%.4
“...Most of your patients now would not get CRS if you end[ed] up using these prophylactic measures,” he said. “And I think that truly will be [how] everybody becomes comfortable using these bispecific antibodies....”
Manni Mohyuddin, MD, assistant professor at Huntsman, echoed this and predicted that bispecifics would become dominant in community-based myeloma treatment.
The panelists also discussed the barrier to care for these therapies for patients who have long distances to travel—a challenge of particular importance for the area of the country where they practice.
“It’s unfortunate for our patients that they have to travel as much as they do, and we all understand when you live in a rural or frontier location, it’s not going to be as convenient to access treatment,” said Hunter. As a result, patients sometimes decide to forego treatment, even for a potentially curable disease.
For tumor-infiltrating lymphocyte (TIL) therapy, the complex logistics and the 6 to 8 weeks it takes to manufacture the product can create a significant barrier, often resulting in patients’ disease progressing before treatment is available.
Siwen Hu-Lieskovan, PhD, MD, associate professor and director of solid tumor immunotherapy at Huntsman, contrasted TIL’s prolonged process with CAR T-cell therapy. This lengthy wait time means that even highly motivated patients become too sick or their disease too advanced to receive the therapy.
Optimizing Care Delivery and Minimizing Administrative Waste
Mullalley | Image: Intermountain

A group of clinical pharmacists closed out the night, emphasizing the substantial administrative and logistical hurdles that can undermine efficient care delivery and add “time cost” that payers often overlook.
Site-of-care restrictions, driven by insurance attempts to optimize cost reduction and resource efficiency, mandate that certain high-cost supportive care (such as intravenous immunoglobulin [IVIG]) or even specific immunotherapies be administered outside of hospital-based infusion centers. The goal of these restrictions is to save money: IVIG could cost $20,000 in a hospital setting compared with $5000 at home but can result in care fragmentation.
“…The fragmentation can cause high levels of patient confusion and anxiety, and of course, there’s a lot of loss of continuity of care there,” said Kelley Julian, PharmD, BCOP, PGY-2 oncology residency director at Huntsman.
The lack of communication between external and internal systems introduces potential safety gaps. Megan Mullalley, PharmD, BCOP, BCPS, system oncology pharmacy manager at Intermountain Healthcare, pointed out the inherent danger in fragmented data. “How do you know what the patient received?Did they receive the drug?Do external facilities get that information back to you?”
This risk of missing critical information is a hidden cost that organizations must consider when enforcing external site-of-care policies.
Payer Lag and Administrative Burden
Cavalieri | Image: Huntsman Cancer Institute

The pharmacist’s role is crucial in operationalizing new therapies, a process involving formulary admission, system builds, safety checks, and securing insurance approvals, which often lag months behind FDA approval and guideline updates. Emma Jones, PharmD, BCOP, a clinical pharmacy specialist at Huntsman, explained that pharmacists can overcome the inertia of slow-moving payers.
“We know that guidelines and insurance lag with the data, and although pharmacists are rule followers to a T, and we don’t like to go outside of the box, we do assist physicians with letters of medical necessity,” she said. “When we know these therapies are appropriate and they’re evidence based, and we know it’s the best thing for our patients, and our providers are eager to start them, then we can assist with writing those letters to say, ‘This is an evidence-based therapy, and we need this approved as soon as possible.’”
Finally, pharmacists act as the patient safety net, especially when physicians request therapies not yet covered by guidelines or based on complex next-generation sequencing data. Courtney Cavalieri, PharmD, clinical oncology pharmacist at Huntsman, explained that having a pharmacist carry out an internal safety check can ensure that innovation is balanced with patient well-being, even when practicing in the “gray zone” where evidence is emerging.
“I always like to have a conversation. I’m always asking, ‘OK, why?Why is this something you want to do?’” she said. “I’m always backing up to, ‘Is this going to be safe?’”
References
1. Huntington SF, Manzoor BS, Jawaid D, et al. Real-world comparison of health care costs of venetoclax-obinutuzumab vs Bruton’s tyrosine kinase inhibitor use among US Medicare beneficiaries with chronic lymphocytic leukemia in the frontline setting. J Manag Care Spec Pharm. 2024;30(10):1106-1116. doi:10.18553/jmcp.2024.24049
2. Kater AP, Harrup R, Kipps TJ, et al. The MURANO study: final analysis and retreatment/crossover substudy results of VenR for patients with relapsed/refractory CLL. Blood. 2025;145(23):2733-2745. doi:10.1182/blood.2024025525
3. Tam C, Thompson PA. BTK inhibitors in CLL: second-generation drugs and beyond. Blood Adv. 2024;8(9):2300-2309. doi:10.1182/bloodadvances.2023012221
4. Kowalski A, Lykon J, Diamond B, et al. Tocilizumab prophylaxis for patients with multiple myeloma treated with bispecific antibodies. Blood Adv. 2025;9(19):4979-4986. doi:10.1182/bloodadvances.2025016913
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.