- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
MRI Biomarker May Signal Early Heart Damage in DMD
Septal circumferential strain (Ecc) was significantly decreased in LGE-negative boys with Duchenne muscular dystrophy (DMD) and correlated to ventricle changes.
MRI-derived septal circumferential strain (ECC) emerged as a promising biomarker for detecting early impairments in cardiac function in boys with Duchenne muscular dystrophy (DMD), even before signs appear on traditional tests, in a recent study published in Diagnostics.1
Researchers at the University of Maryland explored the utility of cine Displacement Encoding with Stimulated Echoes (DENSE) MRI to measure ECC in boys with DMD who did not yet show late gadolinium enhancement (LGE), a marker of heart fibrosis. These findings demonstrate how septal ECC could help clinicians identify early cardiac dysfunction, a leading cause of death in patients with DMD, enabling earlier interventions.
The study enrolled 10 boys with DMD who were LGE-negative and compared their data with 12 boys of similar age without DMD. Researchers found that septal ECC was significantly reduced in boys with DMD compared with controls. Specifically, septal ECC values were less negative for boys with DMD than those without (–0.13 vs –0.16, P = .019), pointing to reduced myocardial shortening in the septal region.
This impairment in septal ECC outperformed left ventricular ejection fraction (LVEF), a conventional measure of heart function, in distinguishing patients with DMD from those without. When combined with LVEF in a binomial logistic regression model, the 2 metrics together offered superior diagnostic accuracy, achieving an area under the curve of 0.83. This finding underscores the value of septal ECC as a complementary tool to conventional measures like LVEF.
“Importantly, septal ECC could be used as an earlier biomarker than LGE and LVEF for indicating the subtle beginning of LV cardiac engagement in DMD without the need for an exogenous contrast agent,” the study authors said. “Thus, this may enable more frequent, earlier, and better patient-specific treatment decisions.”
Insights Into Ventricular Interactions
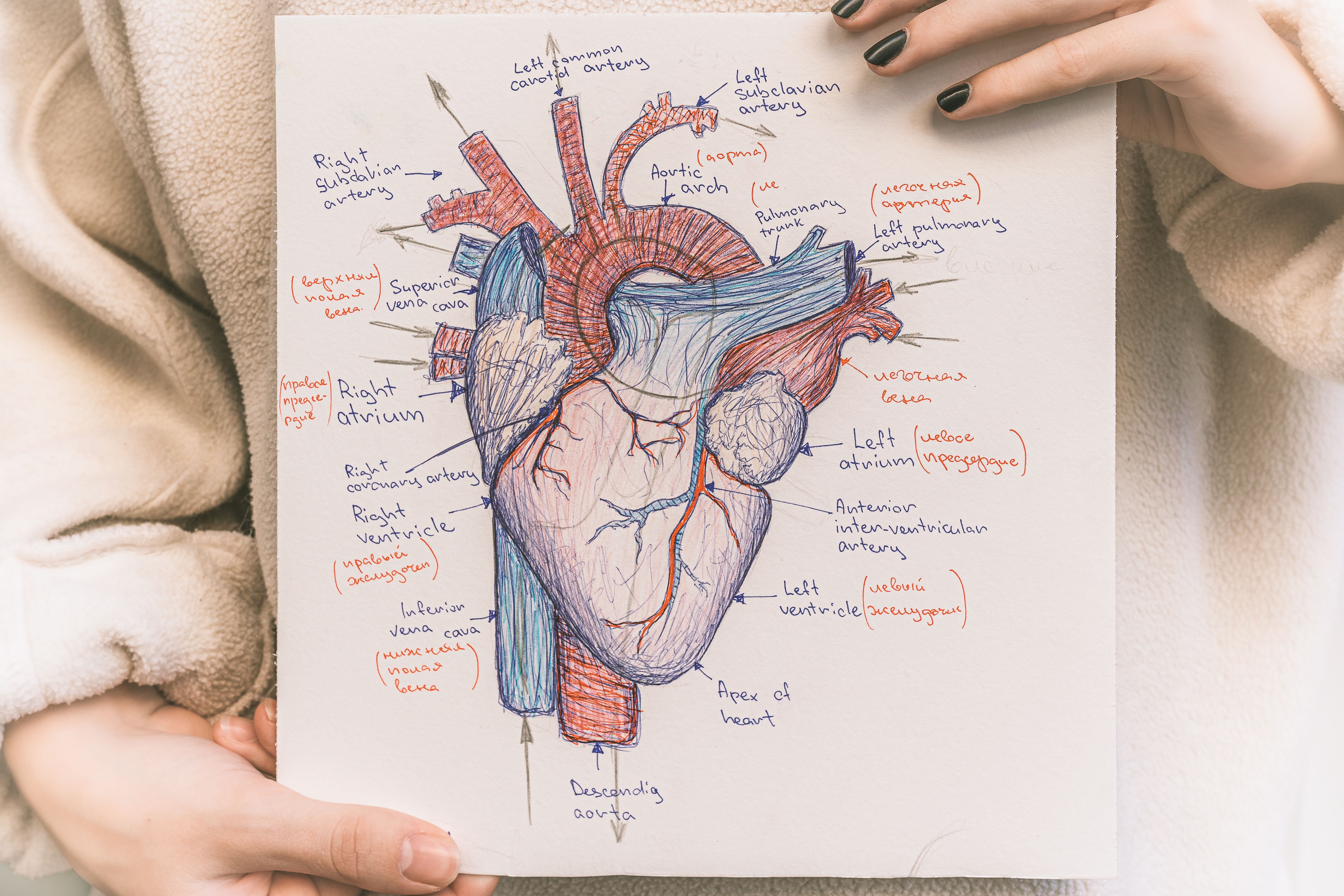
Septal circumferential strain outperformed LVEF in distinguishing patients with DMD from those without. | Image credit: larisikstefania – stock.adobe.com
According to the authors, the most accurate regression model indicated that decreased LVEF and both left and right ventricular end-diastolic volumes (LVEDV, RVEDV) were associated with significantly reduced septal ECC in LGE-negative boys with DMD compared with controls. This finding may be explained by suboptimal sarcomere length due to lower end-diastolic volumes, impairing myocardial contractility as indicated by reduced ECC. Additionally, as a critical interface between the left and right ventricles, the septum may be impacted by decreased biventricular end-diastolic volumes, highlighting its role in ventricular interdependence.
The septum has been previously reported as a highly ventricular-interdependent functional unit.2 However, the authors noted that, unlike the septal ECC, the LV free wall ECC did not show a similar correlation in this study, likely due to compensatory mechanisms observed in conditions like septal infarction.1
“Considering that the LV and RV are connected to the pulmonary circuit and the pulmonary circuit may not be normal in these patients, the changes in end-diastolic loading conditions may be attributed to chronic pulmonary insufficiency,” the authors said.
The study faced a number of limitations, primarily its small sample size, reflecting the inherent challenges of recruiting participants with a rare genetic disease like DMD and well-matched controls. The researchers also noted that while the statistical methods yielded significant findings, the regression model may have overfitted septal ECC due to multiple testing and refitting, potentially resulting in overly optimistic P-values. Additionally, the study's single-time-point evaluation limits the ability to assess longitudinal changes in cardiac function.
“Future work will include the evaluation of within-subject longitudinal changes in ECC assessment to characterize the progression of cardiac involvement and to determine if ECC could be longitudinal imaging end-points for clinical trials,” the authors noted.
References
- Liu ZQ, Maforo NG, Magrath P, et al. MRI-based circumferential strain in boys with early Duchenne muscular dystrophy cardiomyopathy. Diagnostics (Basel). 2024;14(23):2673. doi:10.3390/diagnostics14232673
- Saleh S, Liakopoulos OJ, Buckberg GD. The septal motor of biventricular function. Eur J Cardiothorac Surg. 2006;29 Suppl 1:S126-S138. doi:10.1016/j.ejcts.2006.02.048
Insurance Insights: Dr Jason Shafrin Estimates DMD Insurance Value
July 18th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the July 2024 issue of The American Journal of Managed Care® that estimates the insurance value of novel Duchenne muscular dystrophy (DMD) treatment.
Listen
Quantitative Muscle Ultrasound a Promising Noninvasive Biomarker for DMD
July 29th 2025Quantitative muscle ultrasound correlates strongly with ambulatory and timed function tests in Duchenne muscular dystrophy, suggesting it could complement or even replace more burdensome assessments.
Read More
