- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Medication Adherence: The Lever to Improve Medicare Advantage Star Ratings
Implementing a comprehensive social determinants of health program and addressing the root causes of medication nonadherence could mean the difference between a 3- and 4-star rating in Medicare Advantage.
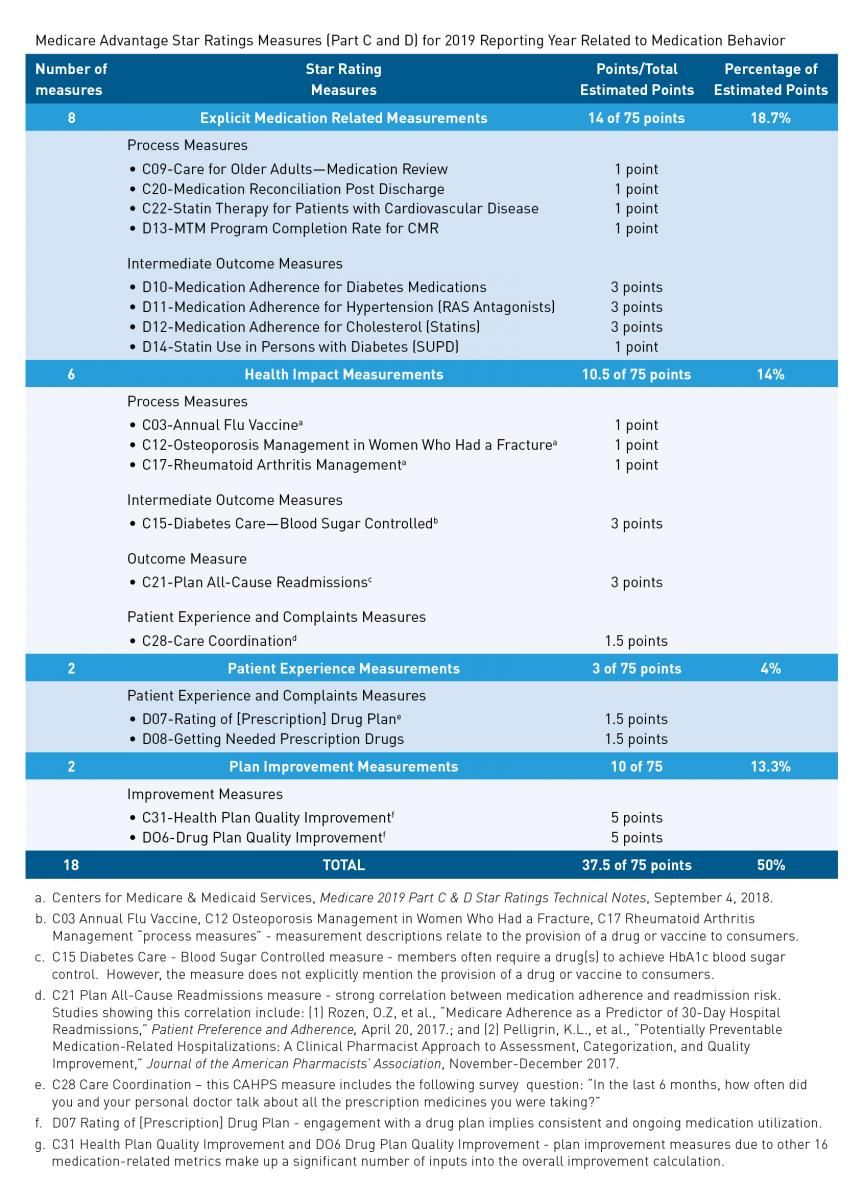
CMS considers medication adherence to be a critical component of plan performance. A cursory scroll through the Medicare Advantage Part C and D measurements reveals that 8 of the 48 measures are specifically related to medication management, including “C20-Medication Reconciliation Post Discharge” and “D10-Medication Adherence for Diabetes Medications.” A closer look, however, reveals that half of the weighting for a health plan’s rating is anchored to medication-related quality measures.
Medication adherence is integral to an organization’s Medicare Advantage Star Rating. It goes beyond doing well on the 8 measures explicitly related to medication use. An analysis conducted by AdhereHealth of CMS’s Star Rating measurement calculus, published in the Medicare 2019 Part C & D Star Ratings Technical Notes1, illustrates that 50% of the weighting for the aggregate rating is tied to a health plan’s support of consumers in taking their prescription medications.
There are many diseases, such as diabetes or hypertension, that can be successfully prevented and managed with drugs. As a result, medication adherence has become critical to a health plan’s ability to improve health outcomes as well as lower total costs. This is reflected across the Star Rating measures. Take for example, the metric “C15-Diabetes Care—Blood Sugar Controlled.” Because many consumers cannot control their blood sugar without medication, a health plan needs an effective diabetic medication adherence approach to score well on this quality measure.
Health plans seeking a lever to improve their Star Ratings would be wise to devote resources towards building a comprehensive medication adherence program. A significant and fairly rapid ROI is possible from these investments, given the prominent role that medication adherence plays in the Star Ratings. Four- and 5-star Medicare Advantage plans receive pay-for-performance bonuses of approximately $500 per member per year from CMS— which equates to $25 million for a 50,000-member plan. A 1-star improvement also increases the likelihood that members will enroll in a plan by 8% to 12%, according to a 2018 Navigant study.2 When both enrollment and CMS bonuses are taken into account, health plans can increase annual revenues by 13.4% to 17.6% by improving from a 3- to a 4-star rating.
How Medication Behaviors Influence Star Ratings
The analysis shows that 18 of the 45 (40%) unique measures in the Medicare Advantage (Part C and D) Star Ratings framework relate in some way to medication behaviors:
- Eight of the measurements are explicitly tied to medication adherence or review, either for all consumers or for consumers taking a particular drug (ie, statins).
- Six of the measurements address specific health impacts that CMS wants health plans to focus on, from blood sugar control in consumers with diabetes to reducing readmissions. In some cases, the measurement definitions mention the importance of taking or discussing the importance of taking needed medications proven by paid pharmacy claims. In other cases, the medical literature provides ample evidence of a causal link between proper medication use and the outcome being measured by hospital admission reductions.
- Two of the measurements relate to patient experience. One measures how easy it is for consumers to get needed prescription drugs. The other experience measure rates patient experience with the drug plan.
- Two measurements relate to health plan improvement, or how much the plan improved over the past year. It’s important to include these measurements in an analysis because the other 16 medication-related metrics represent a significant number of inputs into the plan improvement calculation; as such, these additional measures compound the impact of a plan’s year-over-year medication improvement on the total Star Rating.
Health plans can achieve up to 75 estimated points across all the Star Rating measures. However, not all Star Ratings measures are weighted equally. CMS is trying to encourage healthcare organizations to measure outcomes of care (eg, controlling blood sugar) in addition to whether important processes are carried out (eg, postdischarge medication reconciliation). For this reason, CMS has tripled weighted measures that are focused on achieving desired outcomes.
This chart provides more detail:
Medication-related behavior influences 37.5 out of 75 estimated points achievable in the Star Ratings—or 50% of a Medicare Advantage health plan’s performance. Thus, medication adherence has more influence on a plan’s performance than preventive screenings, member appeals, and other aspects of quality measured in the Star Ratings.
Best Practices for Medication Adherence
Some health plans try to raise their Star Ratings by focusing on improving a handful of measures. However, a broader approach focused on building a comprehensive medication adherence program may lift a health plan’s rating higher, given how medication behaviors are woven throughout the Star Ratings.
Current best practice approaches to medication adherence incorporate several key strategies. One strategy is the use of data analytics to stay on top of when consumers start a new medication as well as when and why they do not comply with their physician’s recommendations. A multidisciplinary approach to case management is another critical element. The team needs to include pharmacists, nurse practitioners, pharmacy technicians, and engagement staff so that consumers can be readily matched with the expert who can most help them with a particular type of adherence issue. For instance, a consumer challenged with medication side effects might be connected to a pharmacist or a pharmacy technician who has been expertly trained to help the consumer overcome barriers to care.
The most important step in medication adherence is engagement, or getting consumers to become actively involved in their own healthcare. It is important to leverage analytics integrated into a clinical workflow system to be the means of knowing which consumers require outreach on an actionable engagement. The first stage of consumer engagement is to identify and alleviate any social determinants of health (SDOH), or socioeconomic issues, impeding a consumer’s ability to fill and take medication. This can include a lack of food, limited access to the pharmacy, issues with transportation to the physician’s office, an inability to cover the cost of copayments, and health literacy issues.
To help consumers overcome SDOH, health plans can modify the formulary to support engagement around adherence. For instance, eliminating copayments for chronic medications knocks down barriers to care. Further, switching consumers to combination medications that treat two conditions at once also helps this barrier. As an example, consumers with diabetes can be put on a combined insulin-statin medication, which the plan purposely puts on a lower formulary tier, instead of having to take separate medications. The consumer is now ingesting one less drug and has lower out-of-pocket costs. This approach helps engage the consumer so they are more open to working with the health plan on adhering to their medications.
Health plans should evaluate their current medication adherence strategy against the best practices outlined above. Implementing a comprehensive SDOH program and addressing the root causes of nonadherence could mean the difference between a 3- and 4-star rating, and, more importantly, greatly benefit consumers’ overall health and wellness.
Author Information
Jason Z. Rose, MHSA, is CEO of AdhereHealth.
References
1. Centers for Medicare & Medicaid Services, Medicare 2019 Part C & D Star Ratings Technical Notes, September 4, 2018.
2. Navigant, The Impact of Star Ratings on Rapidly Growing Medicare Advantage Market, February 27, 2018. https://www.navigant.com/insights/healthcare/2018/medicare-advantage-star-ratings-analysis
