- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Long-Term Analysis From DUO Trial Affirms Benefits of Duvelisib
The new data shed light on long-term outcomes for patients receiving duvelisib, although the investigators said the treatment landscape has also shifted significantly since the original trial.
A new final analysis of the phase 3 DUO trial (NCT02004522) shows duvelisib (Copiktra) continued to have a positive benefit-to-risk ratio in patients with relapsed or refractory (R/R) chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL) after a median follow-up of more than 5 years.
The analysis, which was published in the journal Haematologica, also detailed long-term survival data for participants in the trial.1 Those data showed the median overall survival (OS) of patients in the study’s duvelisib group was 52.3 months.
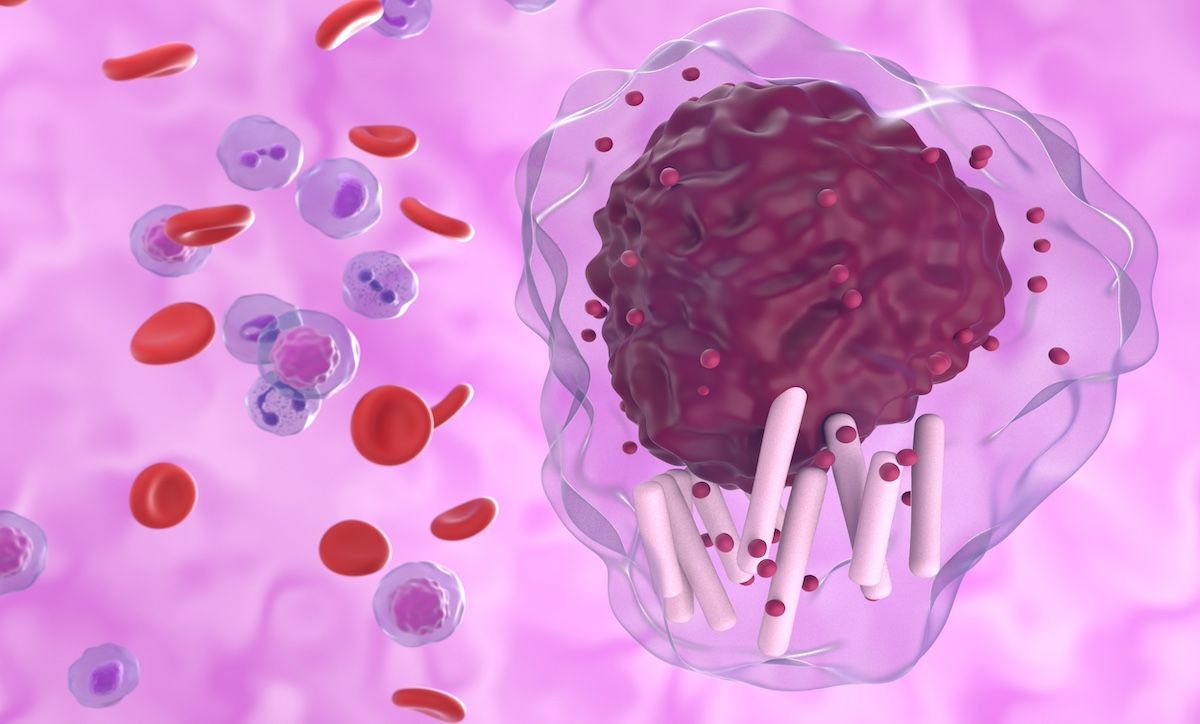
In the DUO trial, duvelisib was compared against the anti-CD20 antibody ofatumumab. | Image Credit: © laszlo - stock.adobe.com
Duvelisib is an oral phosphoinositide 3-kinase-δ/γ inhibitor (PI3Ki). In the DUO trial, it was compared to the anti-CD20 antibody ofatumumab (Kesimpta). To be included in the trial, patients had to have had disease progression or relapse after at least 1 prior line of therapy. They needed to have active disease and no prior exposure to Bruton tyrosine kinase inhibitors (BTKis) or PI3K inhibitors. The authors noted that when the study was initiated in 2013, BTKis were still new and had not been widely integrated into the treatment landscape. Back then, the standard of care for patients with R/R CLL or SLL was chemoimmunotherapy, they noted.
The trial had 319 participants, 160 of whom were randomized to receive 25 mg of oral duvelisib twice daily; the other 159 received ofatumumab intravenously.2 The latter group received infusions weekly for 8 weeks and then monthly for the subsequent 4 months. The study participants had a median age of 69 years, and more than 6 in 10 patients had received at least 2 prior lines of therapy. About one-third of participants (32%) were considered high risk due to del(17p) or TP53 mutations, the authors said.
The initial results were promising, with duvelisib demonstrating superior progression-free survival (PFS) to ofatumumab across all subgroups. OS data were similar in both arms of the study, with neither group reaching a median OS in the primary analysis.
After the study, patients with progressive disease were given the option of crossing over and receiving the other treatment. The authors of the final analysis said 90 patients (57%) in the ofatumumab group switched over to duvelisib, whereas just 9 patients (6%) switched from duvelisib to ofatumumab.1 Most of the patients who switched to duvelisib (77%) achieved a response, with a median duration of response of 14.9 months, the authors said.
When the final analysis was conducted in 2021, the median follow-up time was 63 months, and the median OS for the duvelisib group was 52.3 months, compared with 63.3 months in the ofatumumab group. However, the authors noted that the latter group included patients who had switched over to duvelisib, complicating the results. Duvelisib was administered indefinitely until patients’ disease progressed or until they experienced unacceptable toxicity, while ofatumumab was limited to 12 doses within 7 cycles.
“The large imbalance in patients crossing over from ofatumumab to duvelisib due to PD after a maximum fixed duration of only 7 cycles of ofatumumab essentially meant that comparison of deaths as the study progressed was between patients who were receiving duvelisib in both arms,” they wrote.
The authors said they did not have comprehensive data on which additional therapies participants were prescribed following the end of the trial, but they said the available data suggest that more than 20 additional therapeutic agents were administered to participants post trial.
In terms of safety, the new data showed that 78.5% of participants in the duvelisib group experienced a serious treatment-emergent adverse event (TEAE), the most common of which were infections and infestations and gastrointestinal disorders. Seventy patients discontinued as a result of TEAEs, and 48 patients reduced their doses. Twenty-four patients had TEAEs that resulted in death; the most common causes of death among those patients were infections and infestations (11 patients).
Still, the investigators said these new data affirm that the overall benefit-to-risk balance is favorable for the as-yet-incurable disease. They added, however, that the treatment landscape for CLL/SLL has shifted significantly since the DUO trial started, meaning the patient population of people receiving duvelisib will also be different.
“In light of these changes, future studies to generate prospective data on the efficacy and safety of PI3Ki in the post-BTKi setting, use of duvelisib in combination with other agents, and use of duvelisib as a bridge to other therapies would be informative for clinical practice.
References
- Danilov AV, Flinn IW, Davids MS, et al. The phase III DUO trial of PI3K inhibitor duvelisib versus ofatumumab in relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma: final analysis including overall survival. Haematologica. Published online May 30, 2024. doi:10.3324/haematol.2024.285043
- Flinn IW, Hillmen P, Montillo M, et al. The phase 3 DUO trial: duvelisib vs ofatumumab in relapsed and refractory CLL/SLL. Blood. 2018;132(23):2446-2455. doi:10.1182/blood-2018-05-850461
