- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Key Indicators of Myasthenia Gravis Disease Progression Reduced With Efgartigimod
Research presented at the recent annual meeting of the Academy of Managed Care Pharmacy highlights outcomes among patients who have anti-acetylcholine receptor antibody-positive myasthenia gravis that include reduced exacerbations and need for immunoglobulin.
Substantial declines in immunoglobulin use and reduced exacerbations, crises, and hospitalizations were seen following retrospective cohort analyses of patients who have anti-acetylcholine receptor antibody-positive myasthenia gravis and were treated with efgartigimod.
In new research presented at the recent annual meeting of the Academy of Managed Care Pharmacy, data from US medical and pharmacy claims for 2016 through 2024 were used to emphasize the real-world effectiveness of the immunomodulator first approved by the FDA in 2021.1-3 Overall, there were noted reductions in patients’ needs for other treatments, including intravenous and subcutaneous immunoglobulin and plasma exchange, as well as potential for additional reductions in medical costs and hospitalizations for this patient population. Both retrospective cohort studies also exhibited improvement in Myasthenia Gravis Activities of Daily Living (MG-ADL) scale scores.
Immunoglobulin Usage1
Evidence of efgartigimod’s impact on immunoglobulin usage is scarce, despite the latter being used as a rescue treatment for myasthenic crises or acute exacerbations or as maintenance therapy for symptoms that remain uncontrolled despite administration of other treatments. The 12 months before and 12 months after efgartigimod initiation were used to compare outcomes related to immunoglobulin usage among 166 patients for this first study, who were divided into 2 groups: chronic immunoglobulin use (6 or more courses; n = 103) and intermittent immunoglobulin use (1-5 courses; n = 63).
The mean (SD) patient age was 56.9 (14.9) years, and 56.6% of the patients were women. At baseline, the mean Charlson Comorbidity Index (CCI) score was 1.4 (1.8), and the top 3 most common comorbidities were hypertension, diabetes, and obesity and hyperlipidemia (tied for third). Commercial insurance coverage was most common. Baseline overall MG-ADL scores were 8.0 (4.1), 8.3 (4.2), and 7.5 (4.0) in the overall, chronic immunoglobulin, and intermittent immunoglobulin cohorts, respectively.
For the 12 months before efgartigimod use—the date of the first claim had to be between January 1 and December 31, 2022—most patients overall and in each group were receiving immunoglobulin and oral therapy: 59% overall, 56.3% of chronic immunoglobulin users, and 63.5% of intermittent immunoglobulin users. Corresponding rates of immunoglobulin use only were 20.5%, 20.4%, and less than 20.4% (for this final percentage, the total patient count was masked, but was between more than 0 and less than 20 patients).
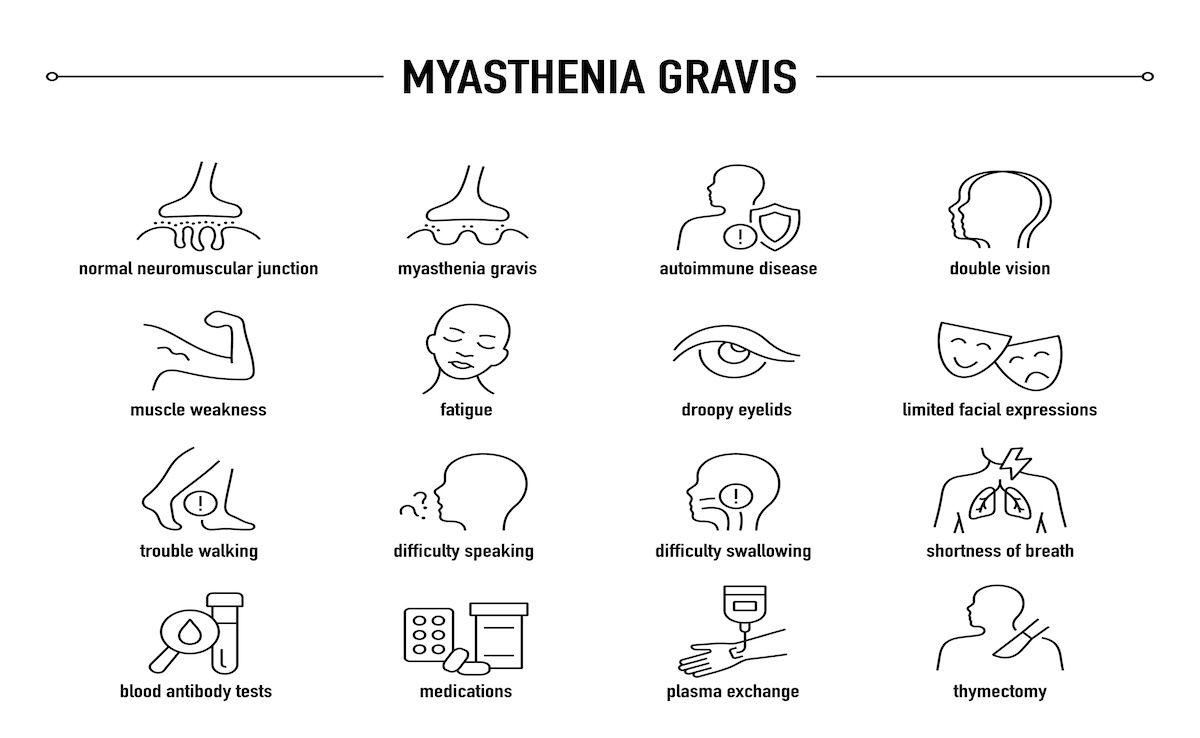
The overall results of these analyses are promising, in that efgartigimod has potential to support enhanced symptom control and thereby improve daily functioning for patients who have anti–acetylcholine receptor antibody-positive myasthenia gravis. | Image Credit: © missbobbit-stock.adobe.com
Following efgartigimod initiation, there was a 95% reduction in all annual immunoglobulin courses (from 1528 to 75). For this analysis, a course was defined as a cluster of immunoglobulin claims occurring 5 days or fewer apart. Among the patients with claims for chronic immunoglobulin use prior to starting treatment with efgartigimod, 84% were able to stop using immunoglobulin after starting on efgartigimod. Further, among those with claims for intermittent immunoglobulin use, 97% were able to stop immunoglobulin use after they started on efgartigimod.
MG-ADL scores were reduced to 4.0 (2.8), 3.7 (2.9), and 4.5 (2.7) among all patients and chronic and intermittent immunoglobulin uses, respectively.
Hospitalization2
As with the first study, patient outcomes were compared for the year before and the year after treatment was initiated with efgartigimod. In this analysis that looked at the effects on hospitalization, however, there were 439 patients included who had at least 1 claim for a non-efgartigimod myasthenia gravis–related treatment in the year before starting treatment with it and continuous treatment with only the medication during the observation period. Concurrent use of additional targeted therapies for generalized myasthenia gravis was not allowed between January 1 and December 31, 2022, and exacerbations were defined using International Classification of Diseases, 10th Revision, codes.
The mean (SD) patient age for this second analysis was 60.6 (14.6) years, and more than half of the patients were men (54.4%). Their mean CCI score was 1.3 (1.8), and the top 3 most common comorbidities were hypertension, hyperlipidemia, and diabetes. Most had commercial insurance or Medicare coverage, and the most common baseline MG-ADL scores—these data were only available for 45.6% of the overall patient population—ranged from 5 to 9 (47%) or 10 to 24 (35.5%).
Compared with the year before efgartigimod use, in the year after efgartigimod use began, there were drops across the board in 6 classes of medications, with the most significant reductions seen for intravenous and subcutaneous immunoglobulin and plasma exchange:
- Intravenous/subcutaneous immunoglobulin: 37.8% to 5.7%
- Plasma exchange: 8.0% to less than 8% (for this final percentage, the total patient count was masked, but was between more than 0 and less than 20 patients)
- Acetylcholinesterase inhibitors: 71.1% to 66.7%
- Oral glucocorticoids: 70.2% to 65.8%
- Nonsteroidal immunosuppressives: 45.8% to 44.0%
- Targeted therapies: 15.5% to 0%
In addition, from before to after efgartigimod initiation, there was a 68% reduction in disease exacerbations, a 71% reduction in crisis events, a 63% reduction in overall hospitalizations, and a 60% reduction in intensive care unit visits. Also, the mean MG-ADL score dropped from 8.0 before efgartigimod initiation to 3.7 by the end of the year after treatment began.
Limitations on Both Analyses1-2
The authors of both posters noted that potential coding errors, selection biases, and missing clinical data, including lab values and physician notes, may limit the generalizability of their findings to a larger population of patients living with myasthenia gravis. In addition, for the first poster, immunoglobulin usage was estimated based on the claims, so exact dosing could not be included in the dataset, and for the second poster, details were not available on individual treatment combinations.
Next Steps
Additional datasets are needed to evaluate longer-term outcomes following efgartigimod imitation in clinical practice. However, the overall results are promising, in that efgartigimod has potential to support enhanced symptom control and thereby improve daily functioning for patients who have anti-acetylcholine receptor antibody-positive myasthenia gravis.
References
1. Jefferson M, Qi C, Narayanaswami P, et al. Changes in intravenous or subcutaneous immunoglobulin usage before and after efgartigimod initiation in patients with myasthenia gravis. Poster presented at: AMCP 2025; March 31-April 3, 2025; Houston, TX. Poster G14.
2. Jefferson M, Smith GA, Narayanaswami P, et al. Hospitalization outcomes after efgartigimod initiation in patients with myasthenia gravis. Poster presented at: AMCP 2025; March 31-April 3, 2025; Houston, TX. Poster G23.
3. Efgartigimod alfa. Drugs.com. Updated November 29, 2024. Accessed April 17, 2025. https://www.drugs.com/efgartigimod-alfa.html#:~:text=Efgartigimod%20alfa%20is%20a%20biologic,under%20the%20brand%20name%20Vyvgart
The Importance of Examining and Preventing Atrial Fibrillation
August 29th 2023At this year’s American Society for Preventive Cardiology Congress on CVD Prevention, Emelia J. Benjamin, MD, ScM, delivered the Honorary Fellow Award Lecture, “The Imperative to Focus on the Prevention of Atrial Fibrillation,” as the recipient of this year’s Honorary Fellow of the American Society for Preventive Cardiology award.
Listen
Promoting Equity in Public Health: Policy, Investment, and Community Engagement Solutions
June 28th 2022On this episode of Managed Care Cast, we speak with Georges C. Benjamin, MD, executive director of the American Public Health Association, on the core takeaways of his keynote session at AHIP 2022 on public health policy and other solutions to promote equitable health and well-being.
Listen
