- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Why Worry About Restricting Access to Medicines in Medicaid?
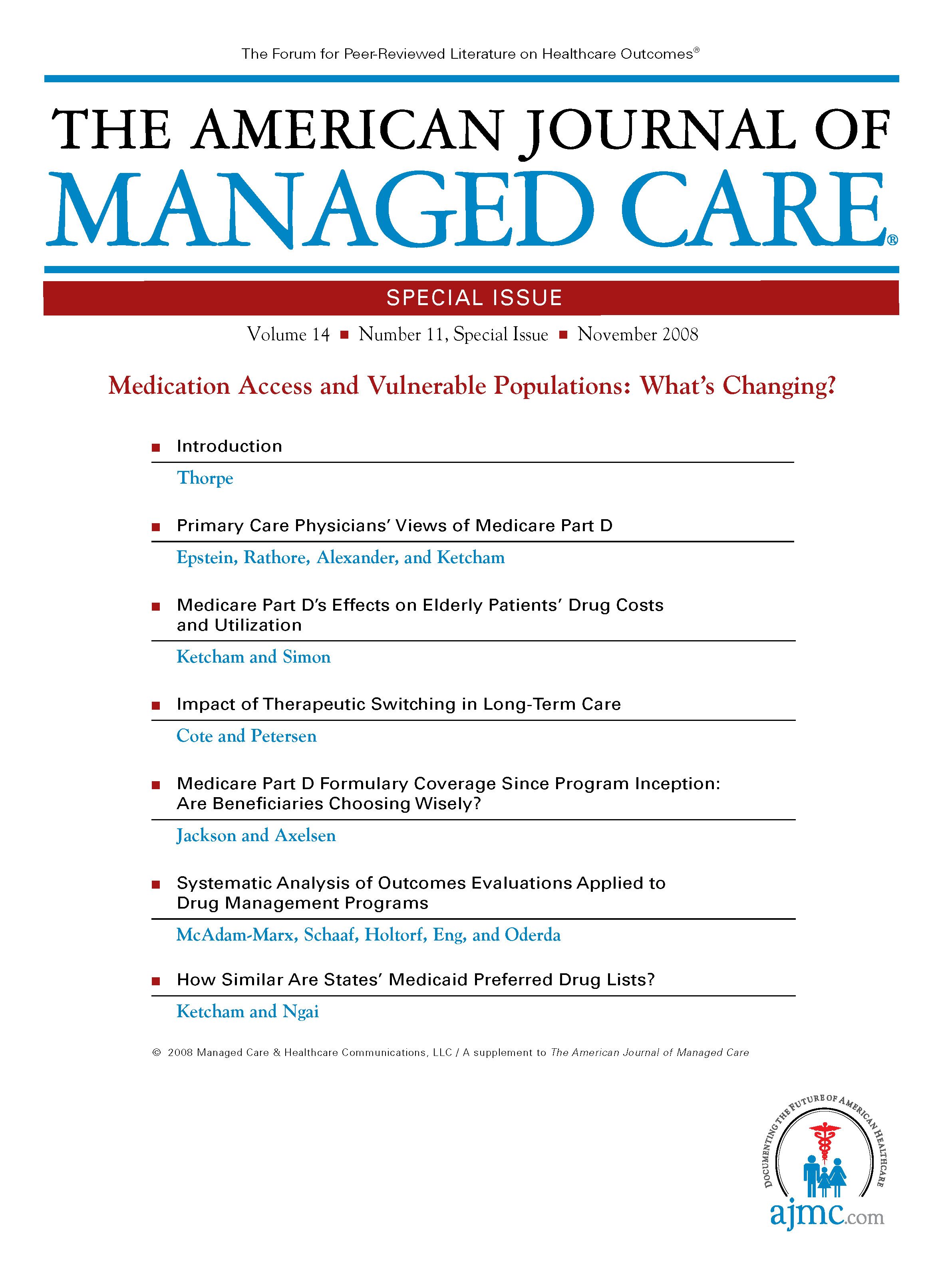
The American Journal of Managed Care
A recent nationwide survey of nearly 1000 black elected officials conducted by the Joint Center for Political and Economic Studies revealed that minority policymakers are quite concerned about the potential effects on their constituents of Medicaid restrictions on drug access (eg, preferred drug lists [PDLs] and/or prior-authorization programs), with 70% believing that such restrictions will make patient health worse.1 The research presented in this special issue of suggests that their concerns are well placed.
A preponderance of states have adopted some kind of access restriction to medicines in their Medicaid programs, and the Medicare drug benefit that begins in 2006 will cause many low-income seniors currently covered in the remaining unrestricted Medicaid programs–as well as their physicians–to become subject to similar restrictions. It is incumbent upon policymakers to understand the consequences of these restrictions. To date, states have focused on the potential for such restrictions to reduce growth in drug spending; this research provides a broader picture of the full effects of such policies. The picture is not pretty.
The articles collected here make 3 basic points. First, the rapid adoption of PDLs should not proceed without broad and serious research into their consequences for patient outcomes; 2 of the articles suggest a link between PDL implementation and patient discontinuation of therapy, increased hospitalizations, and increased physician visits. Second, whatever the ill effects of access restrictions, they fall squarely on a disproportionately minority community. Third, the impact of Medicaid restrictions is not limited to Medicaid patients; instead, the effects are likely to permeate throughout the (largely minority) communities where Medicaid beneficiaries live. Taken together, these results suggest that the current Medicaid access restrictions–and, perhaps, future Medicare access restrictions–may pose a significant obstacle for those who want to resolve the racial and ethnic health disparities that plague our country.
The idea that Medicaid could actually make disparities worse is disheartening to me personally, as the chief medical officer at a hospital treating a largely minority community and as a policy analyst. The Medicaid program has provided a healthcare safety net for the poor for nearly 40 years; and by virtue of the composition of the covered population, it has almost certainly reduced healthcare disparities significantly over that time, perhaps more than any other government program. But well-documented disparities still exist; and starting from where we are now, it seems likely that restricting access to the most advanced technology will cause the disparities to increase. As I have detailed elsewhere, narrowing patients'therapeutic options has potentially negative ramifications, especially for minority patients, from a purely genetic standpoint.2 Dosage adjustments might be necessary in using generic drugs as therapeutic substitutions in untested racial and ethnic groups. There is a distinct possibility of a toxic accumulation of such drugs from slower metabolism, or the need for medical service substitutions to supplement the ineffective generic drugs in some racial and ethnic and minority groups. Either outcome will demand a greater use of health system resources and thus obviate the original purpose of cost containment. Also, it is well known that cultural differences may impact patients'navigation of and treatment within the healthcare system. Most physicians are unaware of the importance of genetic and cultural factors in determining whether patients will respond to and adhere to prescribed regimens, or at least are unaware of the degree of importance of those factors. It seems clear that neither genetic nor cultural factors have been weighed by states that seek to adopt formularies (often adopted to extract price concessions from manufacturers) in their Medicaid programs. Headen and Masia point out what seems self-evident to a physician practicing in Harlem–that changes in Medicaid are going to affect minority patients.3 But the degree of concentration of the physician population treating Medicaid patients detailed by those authors, combined with the spillovers into the non-Medicaid patient population reported by Shinogle and Virabhak,4 provides strong evidence that not only will Medicaid patients be worse off under a restricted-access regime, but also that those effects will themselves be concentrated in minority communities. These effects can only serve to increase health disparities. If the goal of the Surgeon General is to eliminate health disparities by 2010, this Medicaid restriction of access to the latest and most effective medications by legislatures is a giant step backwards.
The paper by Wilson et al suggests a large and statistically significant increase in the likelihood of quitting therapy after a PDL is introduced.5 Of course, if patients fail to adhere to therapy after a PDL is adopted, a policymaker who only examines the drug-cost spending line will likely be pleased, as the negative consequences of failing to take medicine will not appear in the drug budget at all. In the extreme case, if nobody took any medicines, Medicaid would spend nothing on drugs. Naturally, most people think that there would be dire consequences for patients under such a scenario, including unnecessary deaths, hospitalizations, surgeries, and generally worse health. Murawski and Abdelgawad suggest, however, that even those who are solely focused on costs should be concerned about PDLs, as they seem to increase the use of other, potentially much more expensive services for Medicaid patients.6
Those who promote the use of restrictive formularies in Medicaid point to the private sector, which has used such techniques for years, as their model. But those insured privately usually have some way to obtain medicines that do not make the "preferred"list on the formulary, either through a higher copayment or by paying out of pocket. Over time, employers or employees can insist that the best medicines receive coverage and can vote with their feet, switching plans altogether if they are dissatisfied. A person on Medicaid cannot afford to pay out of her own pocket, has no "higher copayment" option, and cannot switch plans. Instead, if she wants access to the latest treatments, she is asked to convince her time-strapped physicians to engage in the bureaucracy. Lichtenberg suggests that PDLs tend to favor older drugs, and though the difference is so far relatively small, it almost surely will increase over time.7 So, although the privately insured will gain access to a wide range of treatments, Medicaid beneficiaries will see a slow narrowing of their therapeutic options. They most certainly will be obligated to use older and cheaper drugs that are placed on the PDL to save money.
The research presented here should be the beginning–not the end–of the debate over the link between restrictions on medication access, health outcomes, and health disparities. As indicated by the authors themselves, their research is far from conclusive. Instead, much of the work here suggests a need for a great deal more research. States are operating under enormous budgetary pressures, and are entitled and in fact obligated to seek ways of safely and appropriately influencing their spending on all services, including prescription drugs. On the other hand, speaking as a clinician, I believe it is clear that if the experiment evaluated here were a clinical trial, minority advocates would insist it be halted. The laser-like focus on cost may be causing policymakers to miss the big picture in their search for a few extra dollars in their budgets, and it is critical for them to focus more widely if we are to close the stubborn gaps in health disparities that continue to prove so frustrating. Prescription drugs represent less than 10% of all Medicaid spending.1 Is a 5% or 10% cut in 10% of the Medicaid budget really worth risking further deterioration in minority health? Balancing the state budget on the backs of the poor is both short sighted and predatory. When the least among us must sacrifice their health as a matter of legislative decree, our system of government has failed in its obligation to care for all of its citizens. In 2002, the Institute of Medicine declared that in order to solve the health disparities dilemma8:
...A comprehensive, multi-level strategy is needed to eliminate these disparities. Broad sectors–including healthcare providers, their patients, payors, health plan purchasers, and society at large–must work together to ensure all patients receive a high quality of healthcare."
The kinds of restrictions being adopted in state Medicaid programs–restrictions that those who manage the coming Medicare drug benefit may seek to emulate–seem the reverse of what the Institute of Medicine suggests.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

