- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Integrative Oncology Program Improves Efficiency and Outcomes in Oncology Care
Advances in cancer treatment provide more options for patients but add complexity to treatment decisions. HealthHelp’s Integrative Oncology program coordinates care to maximize efficiency and ensure optimal outcomes for cancer patients.

Rapidly developing medical technology presents both benefits and challenges to cancer patients and physicians. Although the number of treatment options now available improve quality of life and survival rates for patients, they also make physicians’ selection and coordination of treatments more complex. Care is further complicated by the rising cost of cancer treatment. Total costs are projected to be between $158 billion and $173 billion in 2020, a 39% increase from 2010.1 In addition, some newer cancer drugs now cost $10,000 to $30,000 per month. Patients typically pay 20% to 30% out-of-pocket for drugs, so an average year’s worth of new drugs could cost $24,000 to $36,000 in addition to health insurance premiums.2 These expenses exceed many patients’ ability to pay, and many are forced to simply forego treatments.3 It is critical that patients receive the best possible treatment at the lowest possible cost.
Integrative Oncology
Achieving efficiency and optimization of treatment is the goal of HealthHelp’s new Integrative Oncology program. HealthHelp uses evidence-based guidelines to advise and educate physicians on the most appropriate tests and procedures based on their patients’ symptoms and health history. The goal is to improve provider compliance with oncology care guidelines, which improves patient care and outcomes, while reducing waste caused by unnecessary testing and procedures.
HealthHelp is the first specialty-benefits manager in the nation to offer an Integrative Oncology program. The process begins by identifying a patient’s risk level and, through adaptive algorithms, determining the most appropriate care alongside specialty nursing and physician support. As a patient’s risk level changes, clinical decisions adapt to the patient. HealthHelp is unique in the utilization management industry in that its specialists, drawn from major academic and medical institutions, will proactively call physicians before they even make an authorization request for their patients, in order to provide guidance on their choice of testing and treatment. This physician peer-to-peer program gives the provider a sounding board to discuss appropriate care and offers education on the best treatment for each patient. This multi-institution advanced treatment planning can also influence tumor board decisions on how to best care for patients.
The Integrative Oncology program considers the totality of the patient receiving a full array of services, encompassing the management of 3 modes of therapy:
- Radiation therapy, including intensity-modulated radiation therapy (IMRT), brachytherapy, 2D/3D conformal radiation, stereotactic radiosurgery and radiotherapy, and proton beam therapy.
- Medical oncology, including chemotherapy, hormone therapy, prophylactics, and biologic agents.
- Oncology surgery, including wedge resections, lobectomy, lumpectomy, and others.
This integrative approach to cancer care makes it easy for physicians in different specialties to collaborate and coordinate the treatment a patient receives, developing one cohesive continuum of care. Since patients with cancer frequently work with multiple physicians, cross-specialty coordination is especially important to ensure quality care. The Integrative Oncology program gives radiology and oncology providers access to patient information that may have been administered by a provider in an alternate department or even an alternate facility. This helps to eliminate duplicate or unnecessary testing, which increase patient risk and costs.
The main components of the Integrative Oncology program are:
- Risk assessment and screening. Patient risk is calculated in real time during the authorization process, and the patient is categorized into a risk population based on published, evidence-based literature. Based on his or her category of risk, the patient will be steered to the most cost-effective and appropriate treatment.
- Imaging and staging work-up. This follows a patient when a positive screening has occurred or a request for an authorization comes in for incidental findings, such as lumps, nodules, or masses. There are extensive prediagnosis guidelines for the initial work-up to ensure physicians select the proper sequence of imaging to prevent overtesting or unnecessary testing.
- Biopsies and interventions. HealthHelp’s risk segmentation ensures that high-risk individuals get timely diagnosis and early resection of low-stage cancerous findings, while low-risk individuals do not receive excessive interventions and imaging due to high false-positive rates. Proper upfront screening and imaging schedules are also used to prevent unnecessary biopsies and interventions that are inconvenient and cause anxiety among patients.
- Prognostic assessment. Oncologists and the clinical team reach out and gather information on cancer patients who are undergoing staging and work-up for prognostic assessment. This takes into account the patient’s disease stage, clinical parameters, histopathology, and molecular characterization to determine the patient’s prognosis. This is key to treatment planning and distinguishing between a curative or a palliative path for the patient.
- Treatments and surgeries. This includes chemotherapy, biotherapeutics, ancillaries, radiation therapy, excisions, and surgeries.
- End-of-life care with palliative and curative pathways. By constantly reevaluating a patient’s stage and prognostic indicators, and through case management, the patient’s wishes can be more closely followed if palliative care is needed. If a palliative pathway is determined, to ensure maximum patient comfort, HealthHelp coordinates physical therapy/occupational therapy, pain management, home health nursing, and other services.
- Advocacy/peer oncologist. HealthHelp monitors a patient’s timeline of diagnosis, staging, treatments, and other care needs, so that when appropriate, a peer oncologist can intervene in the process. The peer oncologist creates personalized interactions with both providers and patients to ensure coordination of care, treatment planning, and shared decision making.
- Genetic testing and precision testing. Not everyone is a candidate for genetic testing. Whereas it may be warranted for patients identified as being at greater risk for cancer, it’s an unnecessary expense for many patients. Similarly, certain chemotherapy drugs target specific cancers caused by genetic mutations, such as Avastin (bevacizumab) for recurrent glioblastoma, a type of brain cancer. With precision testing, a biopsy will show whether a patient’s tissue responds to the medication. If it does, the drug is authorized because it clearly works on that patient. If the tissue doesn’t respond, there is no point in prescribing the medication.
By design, our integrative oncology management strategy achieves 3 objectives:
- Ensuring patient safety. This is the most crucial objective of the program. It ensures safety through pathways and treatment guidelines that enhance outcomes for patients undergoing cancer treatment. Patients who need emergency therapy are exempt from review.
- Following evidence-based guidelines. Leveraging evidence-based guidelines eliminates variations in cancer treatment, promotes consistent care, and reduces toxicity. The Integrative Oncology program establishes pathways and treatment plans based on:
- Nationally and internationally recognized standards of care
- Peer-reviewed literature published by societies such as the American Society for Radiation Oncology, American Society of Clinical Oncology, American Society of Hypertension, and National Institute for Health and Care Excellence, as well as Journal of the National Comprehensive Cancer Network,
- Landmark studies and phase 3 trials
3. Striving for cost-effective care. Evaluating current scientific literature when developing clinical pathways identifies treatments that produce the highest efficacy at the lowest toxicity and cost for each stage and state of cancer. HealthHelp’s current radiation therapy and medical oncology programs save payers 15% to 30% and 12% to 25%, respectively, prior to their integration into one continuous process as part of the new integrative oncology program.
Nondenial Model
The Integrative Oncology program leverages HealthHelp’s proven benefits management platform, which is based on a nondenial model of preauthorization. If an initial review finds that a physician’s request does not meet clinical guidelines for approval, the request escalates to a specialty nurse and, if necessary, a peer-to-peer consultation with a specialty physician. The specialist collaborates with the requesting physician to determine the best test or treatment, which usually leads to an agreed-upon change in the procedure or the procedure being withdrawn. However, physicians can be reassured that their requested tests or treatments will be approved even if they don’t align with the preauthorization recommendation. Although HealthHelp will deny a physician’s authorization request if there is concern for patient safety or quality of care (such as overtesting, overtreating, or risk of complications), the real focus is on educating providers to order the right test or procedure for a given patient. Over time, by managing the use of medical and radiation oncology, the peer consultation program enhances physicians’ knowledge and sustains savings by changing long-term ordering patterns as ordering physicians increasingly adhere to best practices.
One recent study of a large state Medicaid program clearly demonstrated the sustainable effects of the HealthHelp model. Over a period of 2 years, the HealthHelp program was responsible for a 46.3% decrease in advanced imaging, resulting in over $42 million in savings. Although there was a sharp decline in utilization immediately after program implementation, a steady decline in utilization over the entire 2-year period was also observed. This continual decrease in utilization supports the efficacy of HealthHelp’s unique education-focused model. Furthermore, the focus on physician education enhances patient outcomes and safety by ensuring patients receive the right test or procedure at the right place at the right time.
Peer Collaboration
HealthHelp’s physician-collaborative peer consultation model has helped thousands of ordering physicians decide the best treatment for their patients. Real-time access to peer experts provides timely and invaluable insight into treatment options. HealthHelp’s clinical pathways were developed in collaboration with leading medical and oncology experts from across the country. The company employs independent radiologists, medical and radiation oncologists, orthopedic surgeons, cardiologists, and sleep specialists from established academic institutions and top teaching hospitals in the world to determine medical necessity based on nationally recognized standards of care.
Medical Oncology
TABLE 1
FIGURE
The success and effectiveness of the Medical Oncology program is exemplified by a case study of one of HealthHelp’s clients, a regional health plan in the Southwest. In 2013, the plan saw that 3 of 4 medical oncology requests resulted in a peer-to-peer consultation, resulting in a relatively high percentage change in treatment plan or withdrawal of request (). Due to the high-cost nature of medical oncology, even a slight change results in large savings and a sizeable return on investment (ROI). For this client, 216 cases were impacted, resulting in a 15.7% ROI ().
TABLE 1.
Number of Requests and Impact of HealthHelp’s Medical Oncology Program for a Regional Health Plan (2013)a
Medical
Oncology
Q1 2013
Q2 2013
Q3 2013
Q4 2013
Total
Measures
N, %
N, %
N, %
N, %
N, %
Peer-peer
230, 82.4
196, 73.7
394, 74.6
345, 70.1
1165, 74.4
Impacted
39, 14.0
47, 17.7
80, 15.2
50, 10.2
216, 13.8
Procedures
avoided
14, 5.0
16, 16.0
43, 8.1
27, 5.5
100, 6.4
Approved immediately
49, 17.6
70, 26.3
134, 25.4
147, 29.9
400, 25.6
Total
279, 100
266, 100
528, 100
492, 100
1565, 100
aTable shows the number (N) of requested procedures approved immediately vs escalated to peer-to-peer review. For procedures escalated to peer-to-peer, the number impacted (altered or avoided) as well as the number avoided are provided. Percent of total cases in each category is listed next to the number of cases.
FIGURE.
Count of Medical Oncology Consults by Type for a Regional Health Plan (2013)
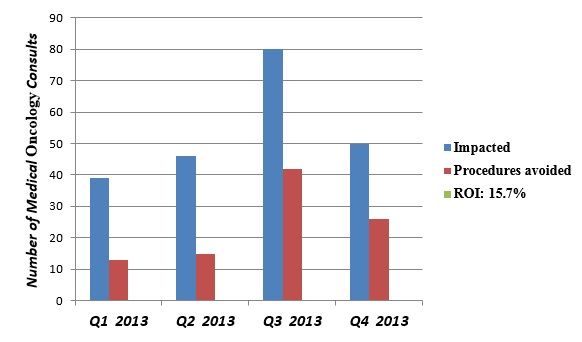
ROI indicates return of investment.
Savings are achieved by shifting to more cost-effective treatments and following clinical guidelines. For example, a switch from Neulasta to Neupogen means the average cost shifts from $4360 to $450. Colon cancer with KRAS mutation does not respond to erbitux (cetuximab); physicians should avoid this and other ineffective treatments that may only result in toxicity among patients. Thus, payers and patients save money while improving safety and outcomes for patients.
Radiation Therapy
HealthHelp’s Radiation Therapy rogram improves quality and safety by reducing 4 undesirable outcomes:
- Excessive radiation exposure. The radiation dose per treatment is too high or the total radiation dose exceeds a recommended level, which could result in secondary cancers.
- Insufficient radiation dose to eradicate a tumor. The radiation dose per treatment is too low, or the total radiation dose is less than recommended.
- Procedures with limited evidence to support improved survival. For example, stereotactic and proton-beam therapy have less than 5 years of data to show that they improve survival, whereas 2D/3D and IMRT have more than 10 years of data to support improved survival.
- Significant complications. Understanding patient clinical information and using best-practices guidelines can ensure patients receive medically appropriate procedures. Further, HealthHelp’s program provides continuity of care through triage to approg-priate wellness services, care advocates, and palliative care, which prevent many avoidable complications.
TABLE 2
Overall, about 30% of preauthorization consultations go to a peer-to-peer physician review, 14% are impacted, and 5% are withdrawn (). Recent study results confirm that while the consultative preauthorization process reduces utilization, it still provides doctors and patients access to appropriate testing. The study analyzed 4 years of clinical data, looking at cases where physicians’ preauthorization review with a consulting radiologist led to a modified test request.
TABLE 2.
Percentage of Requests in Radiation Therapy Receiving Peer-to-Peer Review, and National Impact (2013)
Radiation Therapy
2013 Total
Measures
Commercial
Medicare
Peer-to-peer
28.8%
37.2%
Impacted
15.3%
13.7%
Procedures avoided
5.3%
4.4%
The research examined data from 4 common neuroimaging sequences:
- Request for head computed tomography (CT) modified to head magnetic resonance imaging (MRI)
- Request for both head CT and intracranial computed tomography angiography (CTA) or both head MRI and intracranial magnetic resonance angiography (MRA) modified to a request for a single study
- Request for a CT of both the head and sinuses modified to a request for a single study
- Request for an MRI of the head and orbits modified to a request for a single study.
In 3 of the sequences, no provider reinitiated a study within 30 days. (Researchers chose a 30-day test period because it seemed a reasonable time frame for a doctor to order follow-up testing for a somewhat urgent problem if the first test was inadequate.) In the fourth sequence, only 4 of 64 (6%) withdrawn requests for head CT/MRI or head CTA/MRA were re-initiated within 30 days. Overall, for 99.2% of the requests that were modified through peer-to-peer consultation, the original requested test was not performed in the subsequent 30 days. This low re-initiation rate confirms that the collaborative consultation fulfilled the providers’ clinical objective.4 Again, patients received the right test at the right time, the first time.
Summary
EBO
HealthHelp’s Integrative Oncology Specialty Health Management program brings together a continual pathway for managing each cancer type, which creates cost savings and improved patient outcomes by utilizing the adaptive and unique program design. It enables patients to receive medically appropriate care, care management, and end-of-life services; provides education and risk management for providers; and generates significant savings for payers. Long-term improved outcomes are achieved by reforming the behavior of providers through a consultative and educative process. The focus is on giving the right care at the right time across the entire cancer continuum. This model program delivers sustainable cost savings to payers and patients while promoting patient safety and quality of treatment.
Author information
Amit Gupta, MD, is chief strategy and products officer, HealthHelp.
Address for correspondence
Amit Gupta, MD
HealthHelp
16495 Northchase Dr
Suite 1300
References
Houston, TX 77060
- Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. doi:10.1093/jnci/djq495.
- Glover L. Oncologists worry about rising costs of cancer treatment. US News & World Report website. http://health.usnews.com/health-news/patient-advice/articles/2015/07/01/oncologists-worry-about-rising-costs-of-cancer-treatment. Published July 1, 2015. Accessed April 18, 2016.
- Young RC. Value-based cancer care. N Engl J Med. 2015;373(27):2593-2595. doi:10.1056/NEJMp1508387.
- Powell AC, Hippe DS, Long JW, Robinson JD. Reinitiation of withdrawn or modified neuroimaging requests after collaborative consultation. Acad Radiol. 2015;22(11):1433-1438. doi:10.1016/j.acra.2015.08.005.


