- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
In Myelofibrosis, Ruxolitinib Before and After Allo-HSCT May Improve Success Rate
A review by authors from China examines evidence involving different treatment approaches.
When ruxolitinib (Jakafi, Incyte) is given to patients with myelofibrosis in the period before and after they receive a stem cell transplant, it appears to cut the risk of graft-vs-host disease (GVHD) and may boost the transplant's chances for success, according to a review. Overall, potential benefits outweigh the risk of adverse effects, according to authors from West China Hospital at Sichuan University in China.
The review, which first appeared online this spring, received final publication this week in Annals of Hematology.1 The authors examine multiple studies involving the use of ruxolitinib, the Janus kinase (JAK) 1/2 inhibitor, before and after allogeneic hematopoietic stem cell transplantation (allo-HSCT), a procedure that calls for infusing stem cells from a healthy donor into the patient.
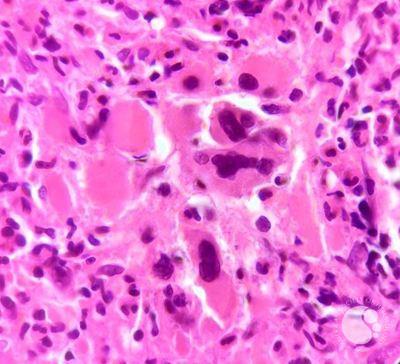
Ruxolitinib given to patients with myelofibrosis before and after stem cell transplant cuts the risk of graft-vs-host disease and may boost the transplant's chances for success.
Image credit: ASH Image bank
As explained by the authors, myelofibrosis is Philadelphia chromosome-negative myeloproliferative neoplasm with an estimated median survival of 6 years.2 Following FDA approval in 2011,3 ruxolitinib has offered patients with myelofibrosis significant relief from symptoms and improvement in quality of life; however, at present only allo-HSCT offers a potential cure for the condition.
The downside of a transplant, as the authors discussed, is that it creates the risk of GVHD and other complications. In recent years, the authors wrote, clinicians have taken different approaches to the use of ruxolitinib surrounding allo-HSCT; patients have been tapered off therapy well in advance or treated up the week of the procedure.
As the authors explained, the goal is to strike the balance between the ability of ruxolitinib to stave off GVHD with concerns that recovery of the immune system after transplant may be hampered by the use of JAK inhibitors. They cite the 2015 European Primary Myelofibrosis Guidelines,2 which called for starting ruxolitinib at least 2 months before transplantation, “followed by gradual adjustment to the maximum tolerated dose and slow tapering over 5–7 days before pretransplant conditioning to achieve complete discontinuation 1 day before the conditioning.”1
The mechanism of JAK inhibitors justifies caution in using them in advance of allo-HSCT. “Considering that JAK2 is also a signaling pathway on which numerous hematopoietic growth factors are dependent, ruxolitinib significantly affects hematopoiesis, leading to an inherent risk of delayed engraftment and graft malfunction after [myelofibrosis] transplantation,” the authors wrote.1 This is why some transplant centers reduce therapy or halt it completely in advance of transplant. But the risk to the patient is a cytokine storm, a kind of “rebound effect” known as ruxolitinib discontinuation syndrome (RDS), which can cause myelofibrosis to rapidly progress ahead of transplant.
Thus, based on the evidence, the authors call for tapering off ruxolitinib more gradually, following replacement with chemotherapy and immunosuppressive therapy just before the procedure.
As for treatment post-transplant, the authors cite several studies that support use of ruxolitinib, including a retrospective cohort study that found the best outcomes among a group of patients who received therapy before and after transplant, as determined by measurements of the spleen and faster engrafting rates.4
Most of the evidence in the review involves ruxolitinib; the authors briefly discussed the JAK inhibitors fedratinib, pacritinib, momelotinib, jaktinib, and gandotinib.
Beyond their general conclusion that use of ruxolitinib under specific protocols before and after allo-HSCT offered the best potential for post-transplant success, the authors stated that more evidence is needed. “At present the post-HCT impact of peri-implantation use of [ruxolitinib] or other JAK inhibitors awaits support from larger prospective randomized trials.”
References
1. Wang Z, Jin X, Zeng J, Xiong Z, Chen X. The application of JAK inhibitors in the peri-transplantation period of hematopoietic stem cell transplantation for myelofibrosis. Ann Hematol. 2024;103:3293-3301. doi.org:10.1007/s00277-024-05703-1
2. Kröger NM, Deeg JH, Olavarria E, et al. Indication and management of allogeneic stem cell transplantation in primary myelofibrosis: a consensus process by an EBMT/ELN international working group. Leukemia. 2015;29(11):2126–2133. doi.org:10.1038/leu.2015.233
3. FDA approves Incyte's Jakafi (ruxolitinib) for patients with myelofibrosis. Incyte. News release. November 16, 2011. Accessed September 5, 2024. https://investor.incyte.com/news-releases/news-release-details/fda-approves-incytes-jakafitm-ruxolitinib-patients-myelofibrosis
4. Pu JJ, Poulose J, Malysz J, et al. Impact of ruxolitinib on myelofibrosis patients post allogeneic stem cell transplant—a pilot study. BJ Haem. 2019;186(5):e130-e133. doi:10.1111/bjh.15967
