- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Impact of Dementia on Costs of Modifiable Comorbid Conditions
Alzheimer disease and other dementias (ADOD) have a substantial impact on the prevalence and costs of certain comorbid conditions compared with matched beneficiaries without ADOD.
ABSTRACT
Objectives: To use the CMS 5% data sample to explore the impact of Alzheimer disease and other dementias (ADOD) on individual and population costs of certain potentially modifiable comorbid conditions, in order to assist in the design of population health management (PHM) programs for individuals with ADOD.
Study Design: A cross-sectional retrospective analysis was performed on parts A and B claims data of 1,056,741 Medicare beneficiaries 65 years and older with service dates in 2010.
Methods: The primary analysis compared the prevalence and costs of 15 comorbid conditions among those with and without ADOD in the entire sample of 1,056,741; in addition, a subset of beneficiaries without ADOD were matched by age, sex, and race on a 1:1 basis to beneficiaries with ADOD. Prevalence and cost ratios were calculated to examine the impact of potentially modifiable study comorbid conditions in both populations.
Results: The prevalence of ADOD in the entire sample was 9.4%, and their costs represented 22.8% of the total. In the matched sample, all 15 comorbid conditions chosen for the study were more prevalent and showed higher mean individual costs in beneficiaries with ADOD compared with those without. The ADOD population also had higher costs and prevalence than the non-ADOD population when single comorbid conditions were examined separately. Study conditions with the highest individual cost ratios were urinary tract infections (UTIs), diabetes with complications, and fractures. Study conditions with the highest population cost ratios were fractures, UTIs, and diabetes without complications.
Conclusions: Prevalence and costs of all study comorbidities were higher in beneficiaries with ADOD compared with those without. Individual cost ratios and population cost ratios may be useful for PHM programs trying to cost-effectively manage individuals with ADOD and comorbid chronic conditions.
Am J Manag Care. 2018;24(11):e344-e351Takeaway Points
Alzheimer disease and other dementias (ADOD) have a substantial impact on the prevalence and costs of certain comorbid conditions that may be modifiable by care management.
- In the Medicare 5% sample, 9.4% of individuals had at least 1 claim for ADOD and were linked to 22.8% of total costs.
- After 1:1 matching on age, sex, and race, patients with ADOD represented 50% of the sample but 70% of the costs.
- Among those with ADOD, prevalence and costs were higher for all 15 study comorbid conditions.
- Understanding the impact and underlying causes of comorbidities in those with ADOD should help stakeholders prioritize care management efforts.
Alzheimer disease and other dementias (ADOD) make up a group of devastating and expensive medical conditions. According to the Alzheimer’s Association, approximately 5.3 million Medicare beneficiaries have ADOD.1 The estimated prevalence among fee-for-service (FFS) beneficiaries is 11%, and the prevalence among those with dual-eligibility status is estimated to be 20%.2 In 2017, Medicare and Medicaid were expected to cover $159 billion, or 61%, of the $259 billion in total healthcare and long-term care payments for individuals with ADOD. The combination of longer lives and aging baby boomers is expected to magnify the ADOD epidemic.3 By 2050, the number of Medicare beneficiaries with ADOD is projected to nearly triple to 13.8 million,4 with the associated healthcare costs exceeding $1 trillion.1
Patients with ADOD have a higher prevalence of chronic conditions (eg, hypertension, diabetes, chronic obstructive pulmonary disease [COPD]) and also higher healthcare costs than the general Medicare population.5-8 These higher costs can be caused by failure to optimally manage these chronic conditions (and other conditions) in patients with ADOD, leading to exacerbations or complications with attendant need for increased utilization of costly healthcare services, including emergency department visits and hospitalizations, and more frequent and longer transitions of care, including increased use of postacute services, such as skilled nursing facilities.
Population health management (PHM) is a technique used to improve the health of defined populations by identifying at-risk patients; deploying individualized interventions, including care management (CM), designed to improve adherence to evidence-based care plans; and measuring outcomes across the population, including improvement in clinical status and reductions in preventable acute events.9 Management of patients with ADOD with comorbid conditions via these programs is more complex than management of patients with similar conditions without ADOD. First, identification of the at-risk population with ADOD through claims data is challenging because ADOD are generally not the primary or even secondary diagnosis listed. Second, PHM interventions are usually focused on engaging directly with patients and activating them to increase care plan adherence. Because of their dementia, patients with ADOD may not be able to follow their prescribed care plans or report their symptoms accurately. They often must rely on informal or formal caregivers not generally targeted by PHM programs to coordinate their medical care.10
The objective of this study was to use the CMS 5% data sample to explore the impact of ADOD on individual and population costs of certain comorbid conditions that are potentially modifiable by CM and other management strategies in order to assist in the design of PHM programs for individuals with ADOD.11,12 It was hypothesized that the inability of individuals with ADOD to manage the modifiable comorbid conditions examined in this study would have a significant impact on their healthcare costs. Prior studies examining the differences in cost between patients with and without ADOD used matching based on the presence of comorbid conditions, removing any cost differential caused by the inability to manage from independent consideration. For this reason, our study was designed to match beneficiaries based only on age, sex, and race so as to reveal the full impact of ADOD on the costs of the modifiable comorbid study conditions.
This study aims to help PHM stakeholders gain insights into the unique challenges of managing the healthcare costs of individuals with ADOD at a population level and at an individual level. We believe that the results provide stakeholders in PHM with a framework for allocating resources and interventions, including CM, where they would have the greatest impact on cost, population health, and the patient experience.
METHODS
Total Population
A cross-sectional retrospective analysis was performed on parts A and B claims data from a 5% CMS sample of 1,056,741 FFS Medicare beneficiaries 65 years and older with service dates in 2010. This data set included individual files for place of service (outpatient, skilled nursing facility, inpatient, home health, and hospice) and eligibility data (age, sex, and race). Part D (drug) claims data are not included in this data sample; thus, drug costs are not part of this analysis.
Population Selection Criteria
Consistent with methodologies13 used in prior ADOD cost and utilization studies,7 individuals with ADOD were selected based on having at least 1 instance of an ADOD diagnostic code (International Classification of Diseases, Ninth Revision [ICD-9] codes 290, 294, and 331). All 10 diagnostic fields available in the CMS claims data set were examined for the presence of an ADOD diagnostic code. The 2 populations of interest were beneficiaries with at least 1 diagnosis of ADOD and beneficiaries with no diagnosis of ADOD, designated the non-ADOD population in this paper. The data were stratified by the presence or absence of 1 or more of the modifiable comorbid conditions.
Modifiable Comorbidities
Fifteen modifiable comorbid diagnostic groups based on Agency for Healthcare Research and Quality Clinical Classifications Software (CCS) groupings14 were selected by the authors (P.S., T.W., and C.S.), each of whom has a different skill set related to PHM (MD/MBA, PhD [epidemiology], and the former CEO of a disease management company, respectively). T.W. provided P.S. with a list of all CCS diagnostic groups; P.S. selected disease groups based on the estimated cost and prevalence of the condition in the study population from prior literature and a professional assessment of the modifiability (ie, prevention, reduction of complications, or avoidance of acute incidents) of the clinical course by employing PHM interventions.
As is typical in the selection of chronic conditions to manage in PHM programs, the study conditions chosen are potentially modifiable via the application of PHM interventions (including CM), thus providing an opportunity for significant cost savings. Mental health conditions, such as depression, that may be amenable to PHM were not included because they can be challenging and costly to definitively diagnose in the presence of dementia.15
The 15 study comorbid conditions, followed by the CCS codes in parentheses, were asthma (128), congestive heart failure (CHF) (108), chronic renal failure (158), COPD (127), diabetes with complications (50), diabetes (diabetes without complications) (49), fractures (225-239), influenza (123), myocardial infarction/coronary artery disease (100-101), osteoporosis (206), pneumonia (122), stroke (109), syncope (245), ulcer/gastritis (139-140), and urinary tract infection (UTI) (159).
Costs
Cost differences were calculated between ADOD and non-ADOD groups, both overall and by each modifiable comorbid condition. Costs were reported as they existed in the claims data sets; no adjustment was made for inflation to current rates. It should be noted that costs reflect actual parts A and B payments made by CMS on behalf of the Medicare program for all covered services in 2010 and do not include co-payments, deductibles, and other out-of-pocket expenses paid by beneficiaries.
Analytic Methods
Demographic and comorbid condition analyses were performed on the entire population of 1,056,741 beneficiaries to compare age, sex, race, and costs between individuals with and without ADOD. The percentage of total costs and percentage of total individuals were evaluated overall and within each comorbid condition population.
Because the unmatched populations of patients with and without ADOD in the 5% sample differed significantly in terms of age, sex, and race distributions, the 2 populations were matched on a 1:1 basis using propensity score matching16 for these 3 variables using SAS version 9.3 (SAS Institute Inc; Cary, North Carolina). To facilitate the exploration of the impact of ADOD on the costs of the study comorbidities, the populations were purposefully not matched on the study comorbid conditions.
The following metrics were calculated in the ADOD and matched non-ADOD populations.
Prevalence ratio. A prevalence ratio (PR) was calculated for each modifiable study comorbid condition as represented by the diagnoses listed in the claims data by dividing the number of individuals with ADOD (numerator) by the number of individuals without an ADOD claim (denominator):
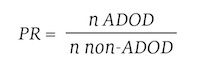
A PR of greater than 1 indicated that the ADOD population had a higher prevalence of the comorbid condition than the non-ADOD population. A ranking of PRs from highest (rank = 1) to lowest was assigned to each study comorbid condition.
Individual cost ratio. An individual cost ratio (ICR) was determined for each of the 15 modifiable study comorbid conditions by looking at the mean costs of individuals who had only 1, and no other, study comorbidity as represented by the diagnoses listed in the claims data (but they may have had other comorbidities not studied). The ratio was calculated by determining the difference in cost between the mean cost of beneficiaries with ADOD with a single study comorbidity (mean cost ADOD with 1 comorbid condition) and the mean cost of beneficiaries without ADOD with the same single comorbidity (mean cost non-ADOD with 1 comorbid condition). These differences in costs between the 2 populations were calculated for each of the 15 subpopulations with each single study comorbid condition. A simple mean of the individual differences was calculated (the simple mean effectively weighing each study comorbid condition equally) and used as the denominator in the equation:
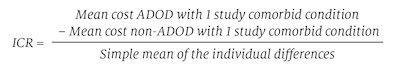
The result was labeled the ICR, as it compares the mean cost per patient of those with and without ADOD and with a single study comorbid condition. The ICRs were ranked from highest (rank = 1) to lowest per study comorbidity if sufficient sample size was evident.
Population cost ratio. A population cost ratio (PCR) was determined for each modifiable study comorbid condition population by multiplying the ICR by the number of patients with ADOD with the specific comorbid condition from the prevalence table and dividing by 10,000 to scale the PCR values into a comparable range with other ratios:
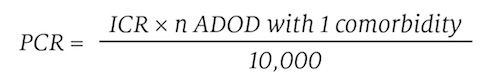
A ranking of PCRs from highest (rank = 1) to lowest was assigned to each modifiable study comorbid condition.
RESULTS
Total (unmatched) Population Findings
The identification of patients with ADOD depended on the examination of all diagnostic fields that were available in the CMS data (eAppendix Table [available at ajmc.com]). For example, only 35% of individuals with ADOD would have been identified if just the first field had been examined. Inclusion of the first 4 fields was required to identify 80% of the cases, and all 10 fields were required to identify all 99,483 patients.
Table 1 highlights that the ADOD population was more likely to be female than the overall population. The age distribution of the ADOD population was strikingly different from the non-ADOD population, with 47% of the ADOD population older than 85 years compared with 15% of the non-ADOD population. Whites and Asians were more likely to be part of the non-ADOD population, whereas blacks and Hispanics were more common in the ADOD population. The non-ADOD and ADOD populations were statistically different by age, sex, and race (all P <.0001) in the unmatched populations.
Table 2 shows that the overall prevalence of ADOD was 9.4%. Individuals with ADOD accounted for 22.8% of the total costs. This table also details the breakdown of ADOD for subpopulations that correspond to each study comorbid population that have at least 1 named comorbid condition (but they could have more than 1). The table shows, for example, that 24.1% of the total population had a claim for both UTI and ADOD, accounting for 36.0% of the total cost of those with UTI. In addition, 28.3% of the total population had claims for stroke and ADOD, accounting for 35.7% of costs, and 22.5% had ADOD and syncope and accounted for 33.7% of costs.
Matched Population Findings
After matching the 2 groups for age, race, and gender, both had 99,483 members and the age (P >.9999), sex (P = .9048), and race (P >.9999) differences seen in the overall sample were no longer statistically significant (Table 1). Mean costs for the matched ADOD population ($17,377) were 2.29 times higher than costs for the non-ADOD population ($7580), or a difference of $9797 per person.
Table 3 shows results in the matched samples. Individuals with ADOD had PRs greater than 1 in all 15 modifiable study comorbid conditions. The highest PRs (3.0) were found for ulcer/gastritis, UTI, and pneumonia. CHF and chronic renal failure had the lowest PR rankings at 2.0 and 1.7, respectively. Table 3 also shows that only 19% of the ADOD population had none of the selected study comorbid conditions compared with 36% of the non-ADOD population.
Table 4 shows the characteristics of the subpopulations with a single study comorbidity. In this table, the percentage of individuals in the matched populations who have only the study comorbidity is compared with the percentage of those who have at least the study comorbidity. Compared with the non-ADOD population, the ADOD population showed a lower and more uniform percentage of people who had at least the study comorbidity.
Table 5 summarizes the mean costs of individuals for each of the selected study comorbidities in the matched sample. The mean costs of individuals with ADOD were consistently higher than the mean costs of those without ADOD for each study comorbid condition. The single comorbidity with the highest ICR, at 1.5, was UTI. Individuals with ADOD and only UTI had $8503 higher mean costs than individuals with only UTI in the non-ADOD population. Diabetes with complications was ranked second, with an ICR of 1.4. It showed $8092 higher mean costs in the ADOD population compared with those in individuals without ADOD and with the same single study comorbidity. Fractures, ulcer/gastritis, diabetes without complications, and asthma as single comorbidities all had ICRs greater than 1.0. Influenza had the lowest ICR (0.5), but the sample size was too small to come to any meaningful conclusion.
Table 5 also summarizes the PCRs for the matched sample. The study comorbid condition with the highest PCR was fractures (5.7), which was followed closely by UTI (5.6) and thereafter diabetes without complications (2.4), CHF (1.4), osteoporosis (1.3), and COPD (1.1).
DISCUSSION
A total 9.4% of individuals in the entire sample (n = 1,056,741) had at least 1 ADOD-related claim, and they accounted for 22.8% of total healthcare costs. The mean annual individual costs in the total sample were $11,245 higher for individuals with ADOD ($17,377) than for those without ($6132). Extrapolating this incremental per person cost to the 5.3 million Medicare beneficiaries with ADOD suggests that Medicare spends approximately $60 billion more every year (in 2010 dollars) to pay for the higher healthcare care needs of individuals with ADOD compared with those without ADOD. Other literature suggests that adjusting for differences between Medicare FFS and Medicare Advantage populations17 would not significantly change this estimate.
Because there were significant differences in the distribution of sex, race, and age between the ADOD and non-ADOD groups in the total population, we used propensity score matching, a quasi-experimental methodology frequently applied to adjust for confounding effects in observational studies,18 to create a non-ADOD subpopulation that was controlled for these parameters. This resulted in 2 equal-sized groups (n = 99,483) that were well matched for sex (χ2 P = .9048), race (P >.9999), and age (P >.9999). We purposely did not match for any comorbid conditions, including the 15 that were the subject of this paper, because we wanted to observe the impact of ADOD on the costs of care for those conditions. After matching, 50% of the matched group were classified as having ADOD and 50% as not having ADOD (by design), yet 70% of the overall cost of care was attributed to the ADOD sample. These differences cannot be due to age, gender, or race.
In order to determine the cost impact of ADOD on each of the 15 study comorbidities and provide population health managers with insights that could help them prioritize individual and population-based interventions, we calculated comorbid condition ICRs and PCRs. We did this by isolating costs among individuals who had only 1 of the selected study comorbidities (although they may have had comorbidities other than the 15 study conditions).
The analysis of the matched population shows that all 15 modifiable comorbid conditions had PRs greater than 1.0 and mean individual costs that were higher for those with ADOD compared with those without. These findings demonstrate that patients with ADOD have both a higher prevalence of certain chronic comorbid conditions and a higher mean per-person cost for those illnesses.
When managing individuals with ADOD, the ICR suggests that a focus on UTIs, severe diabetes with complications, and prevention of fractures is likely to have the biggest impact on costs. However, when organizations are deploying PHM to optimize management of ADOD, they should consider using insights from the PCR calculations to prioritize interventions that minimize fractures, UTIs, and diabetes without complications, in that order.
The fact that both UTIs and fractures are in the top 3 study comorbid conditions for managing individual and/or population costs highlights that preventing or mitigating acute incidents related to these 2 conditions is likely to be cost-effective. The high individual costs of diabetes with complications and the population costs of diabetes without complications underscore the importance of managing diabetes.
The results of this study suggest that efforts to reduce the costs of managing individuals with ADOD require not only management of the neurologic disorder but also more effective management of certain costly comorbid conditions. However, it is clear that a deeper understanding of how ADOD impacts, and likely exacerbates, those conditions—as well as more clarity on the best approaches to preventing or managing them in the face of ADOD—is needed in order to guide payers, providers, and caregivers (both formal and informal) as they develop and deploy their CM solutions.
Finally, an important finding in this study was that the prevalence and incremental costs of ADOD would have been significantly underreported if only the first of the 10 diagnostic fields were used in claims analysis. Failure to accurately identify all individuals with ADOD could lead to a significant missed opportunity to effectively identify and manage this costly patient population.
Limitations
This study relied on medical claims data only. Inherent problems with claims occur because claims are designed to capture data for billing purposes, not medical management. In addition, the 5% sample did not include any pharmacy data (Part D).
The method used to calculate ICRs could be limited for 2 reasons. First, it ignores the potential additive or multiplicative effect of each single study comorbidity in the presence of another single study comorbidity. However, higher costs in ADOD are seen in each subpopulation with each single study comorbid condition. Thus, considering a second study comorbid condition would logically tend to show costs greater than the costs of the subpopulation with a single study comorbid condition. This is easily illustrated by calculating the mean cost per person identified by a study comorbidity in Table 2 to the same in Table 5; for example, in line 1 of Table 2 the mean cost in the asthma subpopulation can be calculated at $21,905 ($87,446,016 / 3992), whereas the mean costs in Table 5 for those with the single comorbid condition of asthma are listed at $9500; similar findings are found for all comorbid conditions. Thus, considering other comorbidities would obviously tend to raise, not lower, costs in each subpopulation considered. Second, the calculation method includes the costs associated with comorbidities that were not included in this study, and these nonstudy comorbidities would logically tend to increase costs. As mentioned above, the 15 study comorbid conditions captured 81% of the ADOD population; therefore, 19% of our ADOD population had none of the study comorbid conditions we selected. This is compared with 36% of the non-ADOD population. Thus, the non-ADOD population tends to have more nonstudy comorbid conditions than the ADOD population; we do not know for sure the impact on cost. Further research into the impact of other comorbid conditions is certainly warranted.
Although the very nonrestrictive definition of ADOD using ICD-9 codes might appear to be a limitation, it would actually lead to “bias toward the null” for 2 reasons: (1) individuals with ADOD but not classified as such would be in the non-ADOD group, on the mean, raising their costs; and (2) individuals without ADOD from a clinical point of view but misclassified as having ADOD, presumably because they had an ADOD diagnostic code in any of the 10 diagnostic fields, would tend to lower the costs of the ADOD group. Thus, the results would likely have been more dramatic if any of these individuals were correctly classified from a clinical point of view.
Finally, it is important to note that the purpose of this paper was not to develop CM or population health strategies for patients with multiple chronic conditions, nor was it to discuss how multiple comorbidities interact, although these are certainly important issues. Rather, it was to illustrate that not only do beneficiaries with ADOD have a higher prevalence of the study comorbidities, but that ADOD also has a significant effect on the cost of select comorbidities. A primary goal was to provide information about the characteristics and costs of a population of Medicare beneficiaries that may help guide care managers and population health managers as they prioritize their efforts.
CONCLUSIONS
ADOD have a substantial impact on the prevalence and costs of certain comorbid conditions that may be modifiable by care management. In the Medicare sample, 9.4% of individuals with at least 1 claim for ADOD were linked to 22.8% of total costs; after 1:1 matching on age, sex, and race, patients with ADOD represented 50% of the sample and 70% of the costs. Among those with ADOD, prevalence and costs were higher for all of the 15 study comorbid conditions. Understanding the impact and underlying causes of comorbidities in those with ADOD can help stakeholders prioritize care management efforts. 
Acknowledgments
The authors thank the Population Health Impact Institute, a 501c3 educational and research organization, for permitting analysis of the CMS 5% data via a data use agreement (DUA Number: LDSS-2010-20422) with CMS for this study.Author Affiliations: The Doctor Weighs In (PRS), Larkspur, CA; Population Health Impact Institute (PRS, TW), Loveland, OH; Ceresti Health (PRS, CES, DS), Carlsbad, CA; Population Health Strategies (CES), Laguna Beach, CA; Trajectory Healthcare (TW), Loveland, OH.
Source of Funding: None.
Author Disclosures: Dr Salber received a small amount of Ceresti Health stock for helping to develop a caregiver curriculum. Ms Selecky is a strategic advisor to Ceresti Health and chief commercial officer on a part-time basis and receives stock options as compensation for her work. Mr Soenksen is the chief executive officer of, a board member at, and an investor in Ceresti Health, which is focused on helping family caregivers of patients who are unable to self-manage their chronic conditions due to having dementia. Dr Wilson is chair of the board of Population Health Impact Institute, a 501c3 organization; owns stock in Trajectory Healthcare, LLC; and received patents 7,685,011 and 7,685,012, from which he receives royalties.
Authorship Information: Concept and design (PRS, CES, DS, TW); acquisition of data (TW); analysis and interpretation of data (PRS, CES, DS, TW); drafting of the manuscript (PRS, CES, DS, TW); critical revision of the manuscript for important intellectual content (PRS, CES, TW); statistical analysis (TW); and administrative, technical, or logistic support (PRS, CES).
Address Correspondence to: Thomas Wilson, PhD, DrPH, Trajectory Healthcare, 10663 Loveland-Madeira Rd #210, Loveland, OH 45140. Email: twilson@trajectory-inc.com.REFERENCES
1. Alzheimer’s Association. 2017 Alzheimer’s disease facts and figures. Alzheimers Dement. 2017;13(4):325-373. doi: 10.1016/j.jalz.2017.02.001.
2. Chronic Conditions Among Medicare Beneficiaries: Chartbook: 2012 Edition. Baltimore, MD: CMS; 2012. cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/Downloads/2012Chartbook.pdf. Accessed June 4, 2017.
3. Larson EB, Yaffe K, Langa KM. New insights into the dementia epidemic. N Engl J Med. 2013;369(24):2275-2277. doi: 10.1056/NEJMp1311405.
4. Herbert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology. 2013;80(19):1778-1783. doi: 10.1212/WNL.0b013e31828726f5.
5. Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA. 2012;307(2):165-172. doi: 10.1001/jama.2011.1964.
6. Bynum JPW, Rabins PV, Weller W, Niefield M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187-194. doi: 10.1111/j.1532-5415.2004.52054.x.
7. Zhao Y, Kuo TC, Weir S, Kramer MS, Ash AS. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer’s. BMC Health Serv Res. 2008;8:108. doi: 10.1186/1472-6963-8-108.
8. Suehs BT, Davis CD, Alvir J, et al. The clinical and economic burden of newly diagnosed Alzheimer’s disease in a Medicare Advantage population. Am J Alzheimers Dis Other Demen. 2013;28(4):384-392. doi: 10.1177/1533317513488911.
9. Lutes M, Wilson TW. Population health management: new perspectives on a familiar concept. EBG Advisors website. ebgadvisors.com/content/uploads/2017/01/EBG-Advisors-Population-Health-Management-White-Paper-May-2014.pdf. Published May 2014. Accessed June 10, 2018.
10. McCormick WC, Kukull WA, van Belle G, Bowen JD, Teri L, Larson EB. Symptom patterns and comorbidity in the early stages of Alzheimer’s disease. J Am Geriatrics Soc. 1994;42(5):517-521. doi: 10.1111/j.1532-5415.1994.tb04974.x.
11. Mechanic R. Will care management improve the value of U.S. health care? The Health Industry Forum website. healthforum.brandeis.edu/meetings/materials/MechanicPrinceton.pdf. Published May 20-21, 2004. Accessed February 21, 2014.
12. Tan ZS, Jennings L, Reuben D. Coordinated care management for dementia in a large academic health system. Health Aff (Millwood). 2014;33(4):619-625. doi: 10.1377/hlthaff.2013.1294.
13. Newcomer R, Clay T, Luxemberg JS, Miller RH. Misclassification and selection bias when identifying Alzheimer’s disease solely from Medicare claims records. J Am Geriatr Soc. 1999;47(2):215-219. doi: 10.1111/j.1532-5415.1999.tb04580.x.
14. Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS), 2015. Rockville, MD: Agency for Healthcare Research and Quality; 2016. hcup-us.ahrq.gov/toolssoftware/ccs/CCSUsersGuide.pdf. Accessed June 10, 2016.
15. Amen DG, Krishnamani P, Meysami S, Newberg A, Raji CA. Classification of depression, cognitive disorders, and co-morbid depression and cognitive disorders with perfusion SPECT neuroimaging. J Alzheimers Dis. 2017;57(1):253-266. doi: 10.3233/JAD-161232.
16. Parsons LS. Performing a 1:N case-control match on propensity score [paper 165-29]. SAS Institute website. www2.sas.com/proceedings/sugi29/165-29.pdf. Accessed December 12, 2017.
17. AHIP Center for Policy and Research. Medicare Advantage demographics report. America’s Health Insurance Plans website. ahip.org/wp-content/uploads/2015/02/MADemo_Report2015.pdf. Published February 2015. Accessed July 10, 2018.
18. He H, Hu J, He J. Chapter 2: overview of propensity score methods. In: He H, Wu P, Chen DG, eds. Statistical Causal Inferences and Their Applications in Public Health Research. Switzerland: Springer International Publishing; 2016. pdfs.semanticscholar.org/1376/2b47079f07eff7340667134bf66f3587be0e.pdf. Accessed June 4, 2018.

Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

