- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Highlighting Interconnected Pathways, Emerging Therapies in CKD and HF
As the prevalence of both chronic kidney disease (CKD) and heart failure (HF) increases, therapies targeting shared pathways are one of the most promising strategies to alter the trajectory of these diseases.
A comprehensive review published in ESC Heart Failure underscored the intertwined nature of chronic kidney disease (CKD) and chronic heart failure (HF), outlining promising advances in therapies that could transform care for patients facing both conditions.1
The review highlighted how often these 2 diseases coexist, particularly in older adults. Roughly half of patients with HF have some degree of kidney disease, and 1 in 4 older adults with CKD also suffer from HF. This overlap worsens outcomes, with comorbid CKD increasing mortality risk in patients with HF by 32% to 51%, depending on the type of HF.
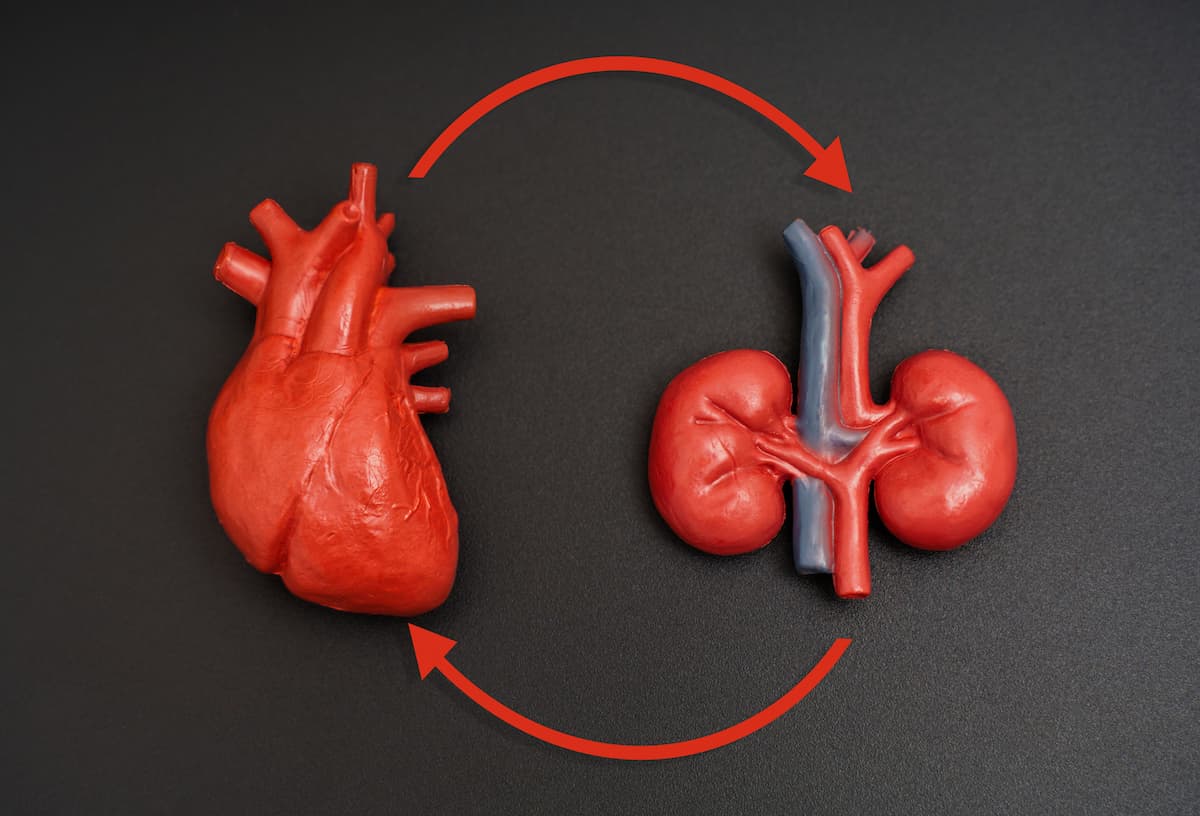
Several therapies address both CKD and HF simultaneously, including RAS inhibitors, which have been shown to slow CKD progression and reduce HF hospitalizations. | Image credit: Katie Chizhevskaya - stock.adobe.com
According to the researchers, CKD and HF are linked by a web of shared risk factors, such as diabetes, obesity, and hypertension, as well as overlapping biological pathways. Inflammation, endothelial dysfunction, neurohormonal activation, and fibrosis play pivotal roles in fueling both diseases.
For example, activation of the renin-angiotensin system (RAS) and sympathetic nervous system initially helps maintain circulation in failing hearts or kidneys. But chronic overactivation drives fibrosis, fluid overload, and adverse cardiac remodeling, worsening both conditions. Likewise, inappropriate activation of the mineralocorticoid receptor (MR) promotes oxidative stress, endothelial dysfunction, and tissue scarring in the heart and kidneys.
This, explained the researchers, creates a self-perpetuating cycle where worsening HF impairs kidney perfusion, while CKD accelerates cardiac dysfunction.
The authors point out that CKD is often underdiagnosed in HF patients. While estimated glomerular filtration rate testing is routine, urine albumin-to-creatinine ratio (UACR) testing, a sensitive marker of early kidney damage, is underused. Low UACR testing rates (4% to 53% in high-risk groups) leave many patients with undetected kidney disease.
On the HF side, natriuretic peptide testing and echocardiography remain central to diagnosis, but interpreting biomarkers like NT-proBNP can be complicated by impaired kidney function. Integrating kidney and cardiac markers may improve risk stratification.
Encouragingly, several therapies address both CKD and HF simultaneously, including RAS inhibitors (angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, and angiotensin-receptor-neprilysin inhibitors), which have been proven to slow CKD progression and reduce HF hospitalizations.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors (dapagliflozin, empagliflozin, and canagliflozin) have also shown robust benefits in reducing CKD progression and lowering HF hospitalization risk, independent of diabetes status. In a meta-analysis of 13 phase 3 trials, accounting for over 90,000 patients, SGLT2 inhibitors were associated with a 40% risk in kidney disease compared with placebo. In a separate meta-analysis of 10 trials, accounting for more than 70,000 patients with high-risk cardiac disease, SGLT2 inhibitors were associated with a lower risk of cardiovascular death or hospitalization resulting from HF compared with placebo (8.10% vs 11.56%).2
Additionally, mineralocorticoid receptor antagonists (finerenone, spironolactone, and eplerenone) reduce fibrosis, inflammation, and proteinuria, with positive effects on both heart and kidneys.
A fourth group of treatments initially developed for type 2 diabetes—glucagon-like peptide-1 (GLP-1) receptor agonists—not only improve glycemic control and reduce weight but may also provide anti-inflammatory and renal protective effects.
Together, a “quadruple therapy” approach of RAS inhibition, SGLT2 inhibition, MR antagonism, and GLP-1 receptor agonism could significantly reduce cardiovascular events and CKD progression, particularly in patients with diabetes and albuminuria, note the researchers.
Despite progress, challenges remain. Polypharmacy is common, given the overlapping conditions and associated comorbidities. Patient adherence, drug interactions, and cost also complicate management. Moreover, gaps exist in understanding how best to tailor therapies across different HF phenotypes and CKD stages.
“Treatment of patients with CKD and HF is complicated by the potential for adverse drug interactions between CKD and HF medications, reduced tolerance to RAS and beta-blockers, diuretic resistance, and impaired efficacy of implantable cardioverter defibrillator and resynchronization device therapy,” explained the researchers.
The authors emphasize the need for earlier diagnosis, better biomarker-based risk stratification, and more personalized treatment strategies. Advances in multi-omics and precision medicine could help identify which patients are most likely to benefit from specific therapies.
References
1. Bauersachs J, Kato ET, Rangaswami J. Interconnected pathways and emerging therapies in chronic kidney disease and heart failure: a comprehensive review. ESC Heart Fail. Published online June 18, 2025. doi:10.1002/ehf2.15345
2. Lala A, Levin A, Khunti K. The interplay between heart failure and chronic kidney disease. 2025;27(7):3568-3582. doi:10.1111/dom.16371
