- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Gene Therapy Enhances Visual Processing for Inherited Retinal Disease
Gene therapy partially restores visual processing in the geniculostriate pathway of patients with Leber congenital amaurosis type 2 while maintaining compensatory activity in the retinotectal pathway.
A recent study from the University of Pennsylvania investigates how gene therapy targeting mutations in the RPE65 gene changes the brain's visual processing pathways. The study, published in Brain, focuses on the use of voretigene neparvovec-rzyl (Luxturna) on patients with Leber congenital amaurosis type 2 (LCA2), a rare genetic disease that causes severe visual impairment.1
The study, which included 7 patients with LCA2, used functional MRI (fMRI) to measure changes in brain activity in the geniculostriate (GS) pathway, which includes the lateral geniculate nucleus (LGN) and primary visual cortex (V1) involved in conscious visual perception, and the retinotectal (RT) pathway, which includes the superior colliculus (SC), traditionally involved in reflexive and orienting responses to visual stimuli.
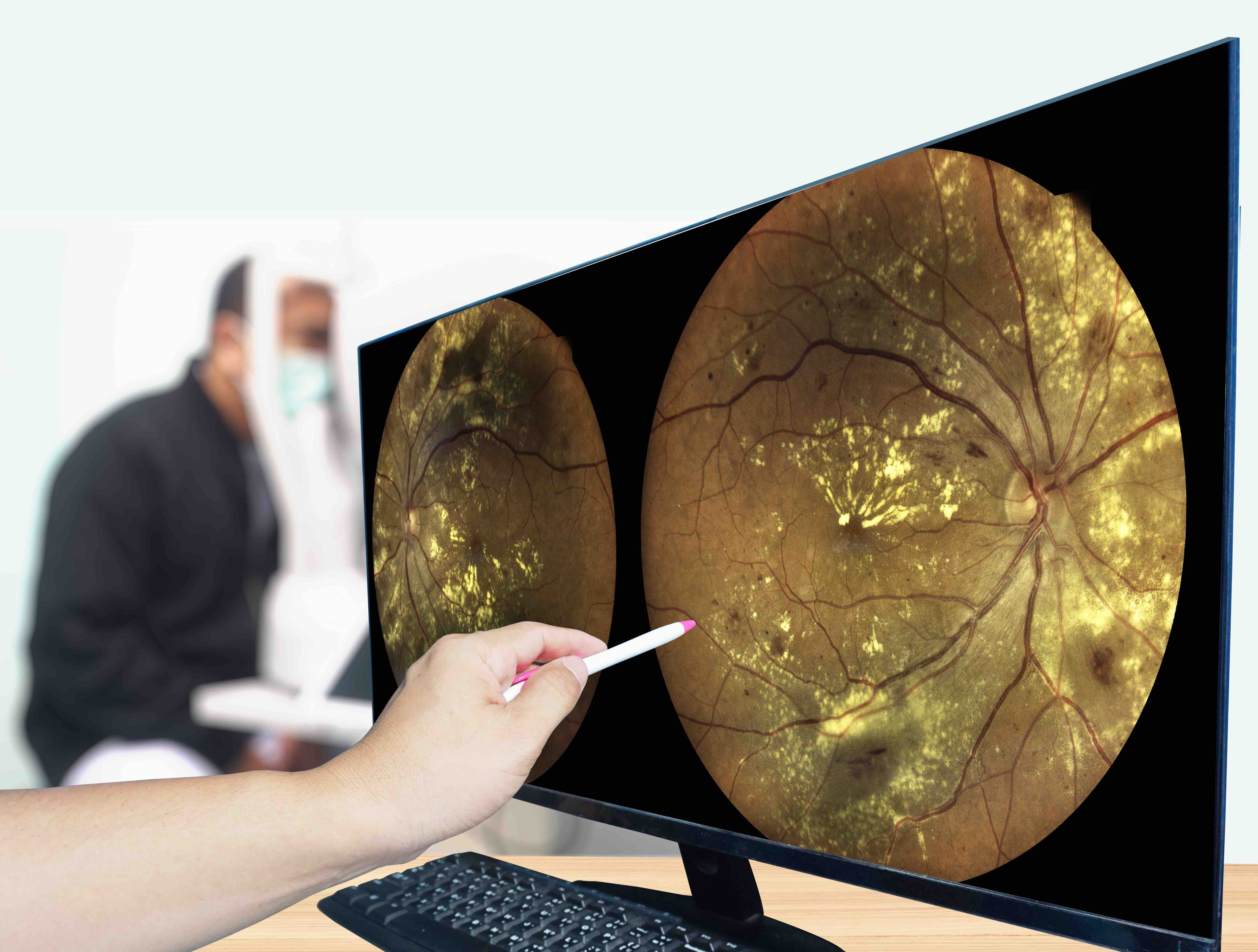
One year after gene therapy, visual fMRI responses remained elevated in the LGN and V1 regions of the geniculostriate pathway of the brain. | Image Credit: © Richman Photo - stock.adobe.com
In the first stage of the study (phase 1/1), patients received gene therapy in their weaker eye through a dose-escalation trial, testing low, medium, and high doses of voretigene neparvovec. This phase showed visual and structural improvements without a clear dose-related effect. A follow-up study (phase 1/2) was performed in which only the high dose was administered to the previously untreated eye in the same patients. fMRI tests were conducted just before and after the second stage of treatment.
At the study's outset, patients with LCA2 exhibited a notable shift in visual processing from the GS pathway to the RT pathway. Visual responses in the cortical area V1 and extrastriate areas BA18/19 were markedly reduced (P = 1.2 × 10−5 and P = .01, respectively). Researchers reported similar reductions in the LGN (P = .004) compared with normally sighted controls. Conversely, fMRI responses in the SC, part of the RT pathway, were significantly elevated (P = 4 × 10−4). "This alteration in the subcortical activation pattern suggests that the retinal degeneration accompanying LCA2 disease shifts the transmission of visual signals more strongly to the RT pathway and away from the GS pathway," noted the authors.
Following treatment with voretigene neparvovec, patients demonstrated partial restoration of GS pathway function. Stimulation of the treated eye resulted in significantly greater fMRI activation in the LGN (P = .003) and V1 (P = .015) regions compared to the untreated eye. LGN activation showed a strong correlation (r = −0.90; P = .04) with performance on the full field sensitivity threshold (FST) clinical assessment for the treated eyes across subjects.
One year after gene therapy, visual fMRI responses remained elevated in the LGN and V1 regions (P = .006 and P = .004, respectively). Notably, this increase was selective to the GS pathway, as no significant changes were seen in the SC (P = .33) or the pulvinar (P = .68), suggesting that “that gene therapy treatment protocol selectively strengthens GS pathway.”
The authors added, "It is interesting to note that the retained elevation of visual responses in the SC following gene therapy may indicate that, despite the improved capacities of the GS pathway, the patients' RT pathway remained strengthened even after the retinal intervention."
The slow degeneration of the retina in LCA2 affects both cone and rod function.2 Jacobson and colleagues found that LCA2 gene therapy enhances extrafoveal rod photoreceptor targeting without improving foveal cone vision.3 Similarly, Cideciyan and colleagues showed the therapy’s impact is far greater on rods, with gains up to 4.8 log units (63,000-fold) vs 1.7 log units (50-fold) for cones.4 The improvements observed in the GS pathway, which carries both rods and cones, is attributed to the targeted delivery of the RPE65 gene via the adeno-associated virus (AAV) vector to rod-dominant retinal regions.
"These findings not only provide useful information regarding the manner in which human vision draws upon these 2 evolved visual pathways but also indicates that a single genetic manipulation can lead to positive clinical outcomes over a wide range of conditions, in this case, improving vision, as reflected by performance in light sensitivity and, to some extent, visual acuity," the authors added.
References
- Ashtari M, Bennett J, Leopold DA. Central visual pathways affected by degenerative retinal disease before and after gene therapy. Brain. 2024;147(9):3234-3246. doi:10.1093/brain/awae096
- Cideciyan AV. Leber congenital amaurosis due to RPE65 mutations and its treatment with gene therapy. Prog Retin Eye Res. 2010;29(5):398-427. doi:10.1016/j.preteyeres.2010.04.002
- Jacobson SG, Cideciyan AV, Ratnakaram R, et al. Gene therapy for Leber congenital amaurosis caused by RPE65 mutations: safety and efficacy in 15 children and adults followed up to 3 years. Arch Ophthalmol. 2012;130(1):9-24. doi:10.1001/archophthalmol.2011.298
